Tuesday Poster Session
Category: IBD
P5501 - In the Blink of an Eye: An Uncommon IBD Extra-Intestinal Manifestation of Panuveitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ashley Matias, MD (she/her/hers)
Naval Medical Center Portsmouth
Portsmouth, VA
Presenting Author(s)
Ashley Matias, MD1, Ian Uber, MD1, Allison Bush, MD2, Nieka Harris, 1
1Naval Medical Center Portsmouth, Portsmouth, VA; 2Uniformed Services University of the Health Sciences, Portsmouth, VA
Introduction: Extraintestinal manifestations (EIMs) frequently occur in inflammatory bowel disease (IBD). Ocular involvement is the third most common EIMs and can occur independently from intestinal inflammation. Uveitis refers to inflammation of any part within the uvea, which includes the iris, ciliary body, and choroid. Panuveitis, a rare EIM, is diffuse inflammation of all parts of the uvea that can also involve the retina secondarily. The management of panuveitis is complex, requiring a multi-disciplinary approach and close monitoring. We present a case of panuveitis secondary to inflammatory bowel disease, highlighting an uncommon and difficult to treat EIM.
Case Description/
Methods: A 21-year-old male presented with hematochezia and was found to have pan colonic erythema and ulcerations on endoscopy. Histology demonstrated active chronic colitis with cryptitis/crypt abscesses; collectively concerning for inflammatory colonic Crohn’s disease. The patient’s symptoms improved on steroids and vedolizumab induction. The patient was tapered off steroids and five months later he presented to the emergency department with blurry vision of the right eye. Ophthalmologic evaluation was consistent with acute iritis with treatment including topical steroids every hour and twice daily atropine drops. On subsequent follow ups, the patient continued to have inflammation and eventually developed involvement of the optic nerve concerning for panuveitis. Oral steroids were restarted, and the patient was transitioned to infliximab infusions. A repeat colonoscopy showed diffuse colitis with deep ulcerations of segmental involvement. Subsequently he was referred to a retinal specialist with recommendation to start methotrexate. The patient reached clinical remission in the setting of infliximab infusions, methotrexate (MTX), azathioprine and oral steroids. His ophthalmologic exam improved to baseline with a plan to taper off steroids and MTX.
Discussion: EIMs occur in approximately 25-40% of IBD patients and can affect the joints, skin, eyes and liver to name a few. Ocular involvement is most commonly episcleritis or anterior uveitis which are treated with topical medications. Panuveitis is a rare EIM and treatment often requires additional systemic immunosuppressive agents as well as oral corticosteroids. This case highlights the importance of a comprehensive evaluation of any ocular complaints in patients with IBD and escalating immunosuppression in more severe cases of ocular EIMs.
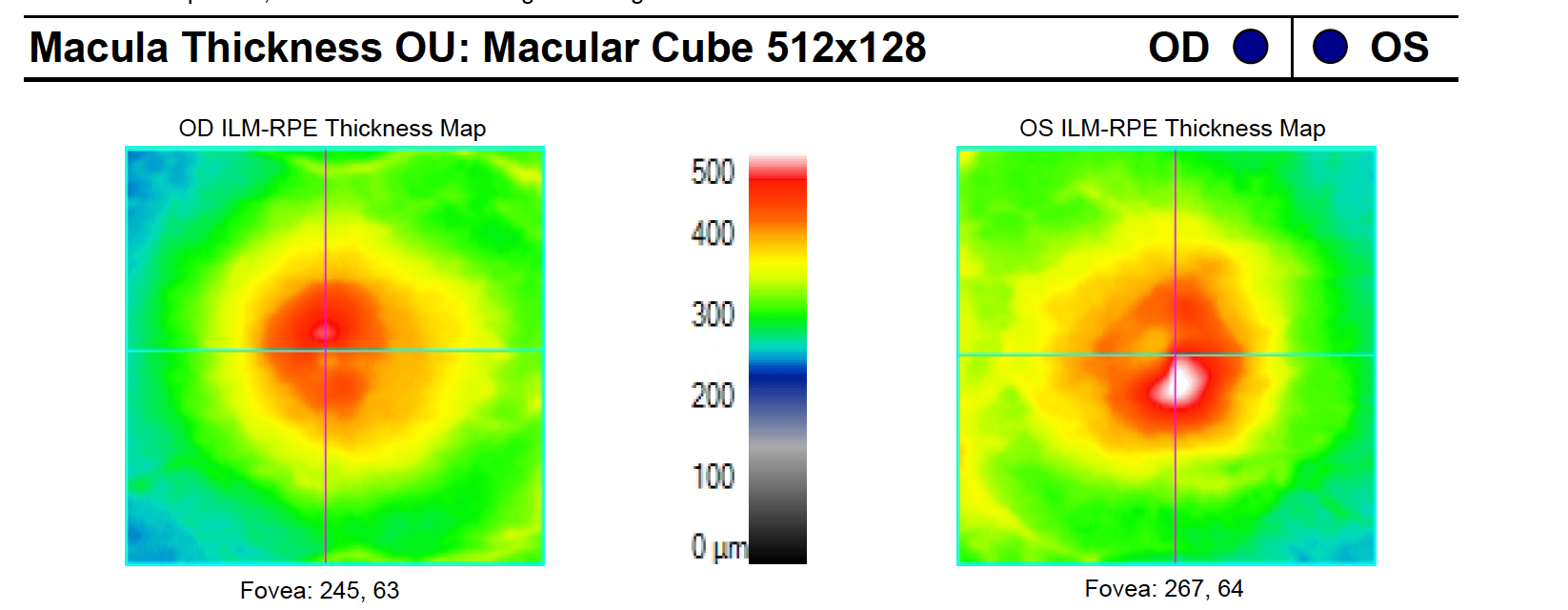
Figure: Initial colonoscopy findings, concerning for Crohns disease.
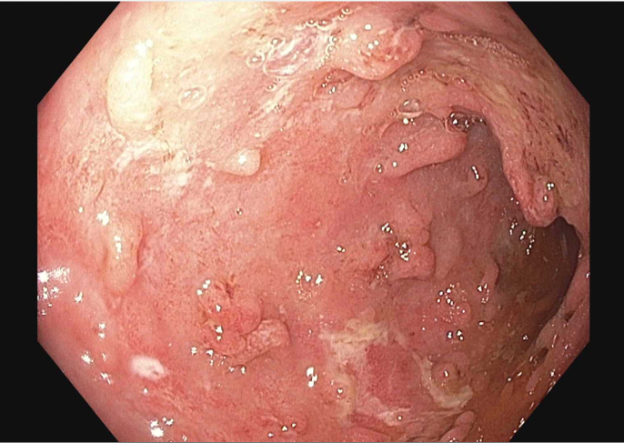
Figure: Measurements of macular thickness, reflective of retinal inflammation. Both eyes show increased macular thickness suggestive of retinitis.
Disclosures:
Ashley Matias indicated no relevant financial relationships.
Ian Uber indicated no relevant financial relationships.
Allison Bush indicated no relevant financial relationships.
Nieka Harris indicated no relevant financial relationships.
Ashley Matias, MD1, Ian Uber, MD1, Allison Bush, MD2, Nieka Harris, 1. P5501 - In the Blink of an Eye: An Uncommon IBD Extra-Intestinal Manifestation of Panuveitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Naval Medical Center Portsmouth, Portsmouth, VA; 2Uniformed Services University of the Health Sciences, Portsmouth, VA
Introduction: Extraintestinal manifestations (EIMs) frequently occur in inflammatory bowel disease (IBD). Ocular involvement is the third most common EIMs and can occur independently from intestinal inflammation. Uveitis refers to inflammation of any part within the uvea, which includes the iris, ciliary body, and choroid. Panuveitis, a rare EIM, is diffuse inflammation of all parts of the uvea that can also involve the retina secondarily. The management of panuveitis is complex, requiring a multi-disciplinary approach and close monitoring. We present a case of panuveitis secondary to inflammatory bowel disease, highlighting an uncommon and difficult to treat EIM.
Case Description/
Methods: A 21-year-old male presented with hematochezia and was found to have pan colonic erythema and ulcerations on endoscopy. Histology demonstrated active chronic colitis with cryptitis/crypt abscesses; collectively concerning for inflammatory colonic Crohn’s disease. The patient’s symptoms improved on steroids and vedolizumab induction. The patient was tapered off steroids and five months later he presented to the emergency department with blurry vision of the right eye. Ophthalmologic evaluation was consistent with acute iritis with treatment including topical steroids every hour and twice daily atropine drops. On subsequent follow ups, the patient continued to have inflammation and eventually developed involvement of the optic nerve concerning for panuveitis. Oral steroids were restarted, and the patient was transitioned to infliximab infusions. A repeat colonoscopy showed diffuse colitis with deep ulcerations of segmental involvement. Subsequently he was referred to a retinal specialist with recommendation to start methotrexate. The patient reached clinical remission in the setting of infliximab infusions, methotrexate (MTX), azathioprine and oral steroids. His ophthalmologic exam improved to baseline with a plan to taper off steroids and MTX.
Discussion: EIMs occur in approximately 25-40% of IBD patients and can affect the joints, skin, eyes and liver to name a few. Ocular involvement is most commonly episcleritis or anterior uveitis which are treated with topical medications. Panuveitis is a rare EIM and treatment often requires additional systemic immunosuppressive agents as well as oral corticosteroids. This case highlights the importance of a comprehensive evaluation of any ocular complaints in patients with IBD and escalating immunosuppression in more severe cases of ocular EIMs.
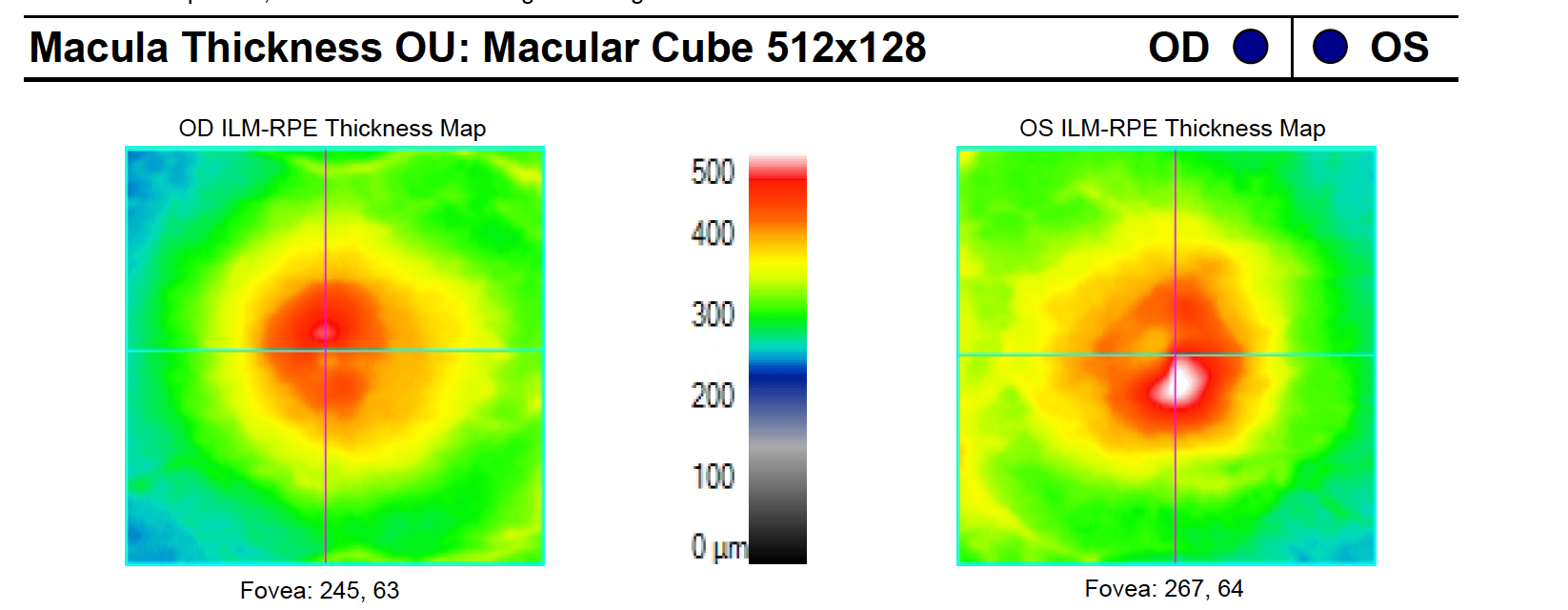
Figure: Initial colonoscopy findings, concerning for Crohns disease.
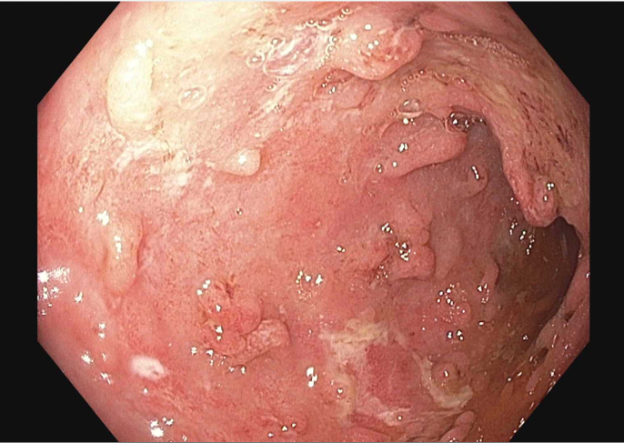
Figure: Measurements of macular thickness, reflective of retinal inflammation. Both eyes show increased macular thickness suggestive of retinitis.
Disclosures:
Ashley Matias indicated no relevant financial relationships.
Ian Uber indicated no relevant financial relationships.
Allison Bush indicated no relevant financial relationships.
Nieka Harris indicated no relevant financial relationships.
Ashley Matias, MD1, Ian Uber, MD1, Allison Bush, MD2, Nieka Harris, 1. P5501 - In the Blink of an Eye: An Uncommon IBD Extra-Intestinal Manifestation of Panuveitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
