Tuesday Poster Session
Category: IBD
P5498 - Crohn’s Remission Gone Rogue: The Curious Case of Obstructing Giant Inflammatory Pseudopolyps
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Andrew L. Petrou, MD (he/him/his)
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Andrew L. Petrou, MD1, Nicholas Scalzo, MD1, Emily L. Romanoff, MD1, Harlan G. Rich, MD2, Sean Fine, MD1, Michael Madrid, MD1, Harry Rosenberg, MD1
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Crohn’s disease (CD) is a chronic, relapsing inflammatory bowel disease (IBD) characterized by transmural inflammation that can affect any part of the gastrointestinal tract. One complication of IBD is the development of inflammatory pseudopolyps (IPs), which are benign mucosal projections arising from repeated cycles of inflammation and regeneration. Rarely, IPs can grow larger than 1.5 cm and are termed giant inflammatory pseudopolyps (GIPs). Surgical intervention is reserved for GIPs that cause obstruction or for cases in which malignancy cannot be excluded. Here, we report a case of a patient with quiescent CD who developed massive GIPs requiring surgery.
Case Description/
Methods: A 54 year-old male with a longstanding history of CD and HIV (CD4 count > 400) presented for follow up. After diagnosis at age 16, the patient remained in clinical remission on aminosalicylate therapy until age 24 when he required a partial colectomy after developing an SBO secondary to CD. Over the years he failed multiple medications including infliximab, adalimumab, and vedolizumab. On establishing care locally, a colonoscopy off therapy showed multiple clusters of diminutive IPs in the descending and transverse colon. Histology revealed chronic mildly active disease in the sigmoid colon. He denied symptoms of active CD, and CRP was normal. A colonoscopy repeated 14 months later for rectal bleeding revealed a new obstructive mass in the proximal descending colon and a partially obstructive mass in the distal descending colon. Superficial biopsies were consistent with inflammatory polyps. He underwent subtotal colectomy for luminal obstruction and to definitively exclude malignancy. Histology was consistent with IPs but otherwise showed normal colonic mucosa.
Discussion: GIPs are a rare complication of IBD and are uncommon in patients with quiescent CD. They can develop rapidly even in the absence of active disease, which suggests that long-term, subclinical mucosal injury may be sufficient to drive exaggerated regenerative changes. Surgical resection can be both therapeutic and diagnostic in cases where malignancy cannot be excluded via biopsy alone. Even with quiescent CD, complications relating to GIPs can arise and present challenges for patients. This case highlights the need for individualized follow-up strategies that consider not only inflammatory activity but also mucosal damage and morphologic evolution over time.
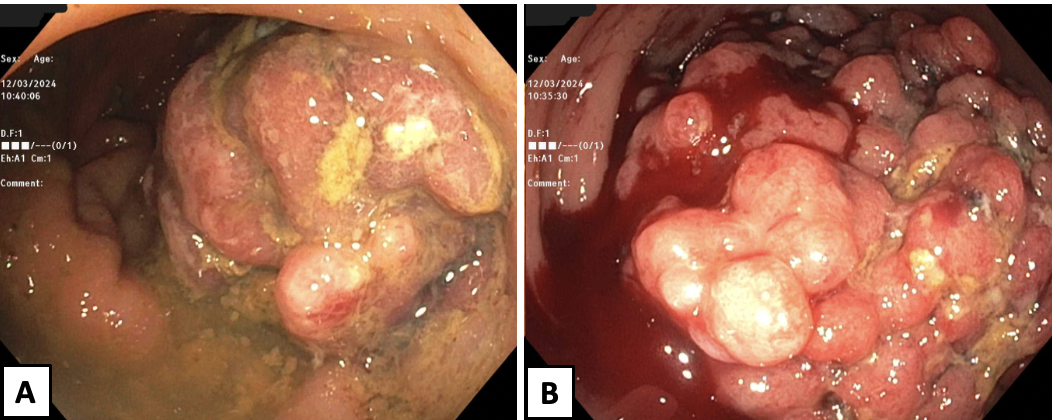
Figure: Figure 1. A. Partially obstructing mass in distal descending colon. B. Obstructing mass in proximal descending colon at which point scope could not be advanced and colonoscopy was aborted.
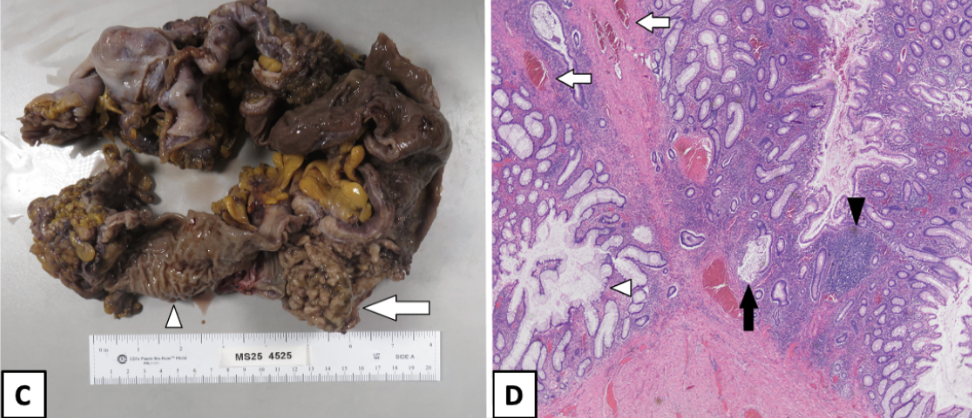
Figure: Figure 2. C. Gross photograph of a subtotal colectomy specimen demonstrating prominent exophytic inflammatory pseudopolyps (arrow), projecting above the denuded mucosal surface. Adjacent normal colonic mucosa (arrowhead) is shown for comparison. D. H&E-stained section (20×) from the base of an inflammatory pseudopolyp. The pseudopolyp is characterized by a crypt abscess with crypt rupture and mucin extravasation (solid arrow), a dense lymphoplasmacytic infiltrate (solid arrowhead), dilated crypts with distorted architecture (white arrowhead), and prominent thick-walled blood vessels (white arrows).
Disclosures:
Andrew Petrou indicated no relevant financial relationships.
Nicholas Scalzo indicated no relevant financial relationships.
Emily Romanoff indicated no relevant financial relationships.
Harlan Rich indicated no relevant financial relationships.
Sean Fine indicated no relevant financial relationships.
Michael Madrid indicated no relevant financial relationships.
Harry Rosenberg indicated no relevant financial relationships.
Andrew L. Petrou, MD1, Nicholas Scalzo, MD1, Emily L. Romanoff, MD1, Harlan G. Rich, MD2, Sean Fine, MD1, Michael Madrid, MD1, Harry Rosenberg, MD1. P5498 - Crohn’s Remission Gone Rogue: The Curious Case of Obstructing Giant Inflammatory Pseudopolyps, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2Brown Medicine/Brown Physicians, Inc., Providence, RI
Introduction: Crohn’s disease (CD) is a chronic, relapsing inflammatory bowel disease (IBD) characterized by transmural inflammation that can affect any part of the gastrointestinal tract. One complication of IBD is the development of inflammatory pseudopolyps (IPs), which are benign mucosal projections arising from repeated cycles of inflammation and regeneration. Rarely, IPs can grow larger than 1.5 cm and are termed giant inflammatory pseudopolyps (GIPs). Surgical intervention is reserved for GIPs that cause obstruction or for cases in which malignancy cannot be excluded. Here, we report a case of a patient with quiescent CD who developed massive GIPs requiring surgery.
Case Description/
Methods: A 54 year-old male with a longstanding history of CD and HIV (CD4 count > 400) presented for follow up. After diagnosis at age 16, the patient remained in clinical remission on aminosalicylate therapy until age 24 when he required a partial colectomy after developing an SBO secondary to CD. Over the years he failed multiple medications including infliximab, adalimumab, and vedolizumab. On establishing care locally, a colonoscopy off therapy showed multiple clusters of diminutive IPs in the descending and transverse colon. Histology revealed chronic mildly active disease in the sigmoid colon. He denied symptoms of active CD, and CRP was normal. A colonoscopy repeated 14 months later for rectal bleeding revealed a new obstructive mass in the proximal descending colon and a partially obstructive mass in the distal descending colon. Superficial biopsies were consistent with inflammatory polyps. He underwent subtotal colectomy for luminal obstruction and to definitively exclude malignancy. Histology was consistent with IPs but otherwise showed normal colonic mucosa.
Discussion: GIPs are a rare complication of IBD and are uncommon in patients with quiescent CD. They can develop rapidly even in the absence of active disease, which suggests that long-term, subclinical mucosal injury may be sufficient to drive exaggerated regenerative changes. Surgical resection can be both therapeutic and diagnostic in cases where malignancy cannot be excluded via biopsy alone. Even with quiescent CD, complications relating to GIPs can arise and present challenges for patients. This case highlights the need for individualized follow-up strategies that consider not only inflammatory activity but also mucosal damage and morphologic evolution over time.
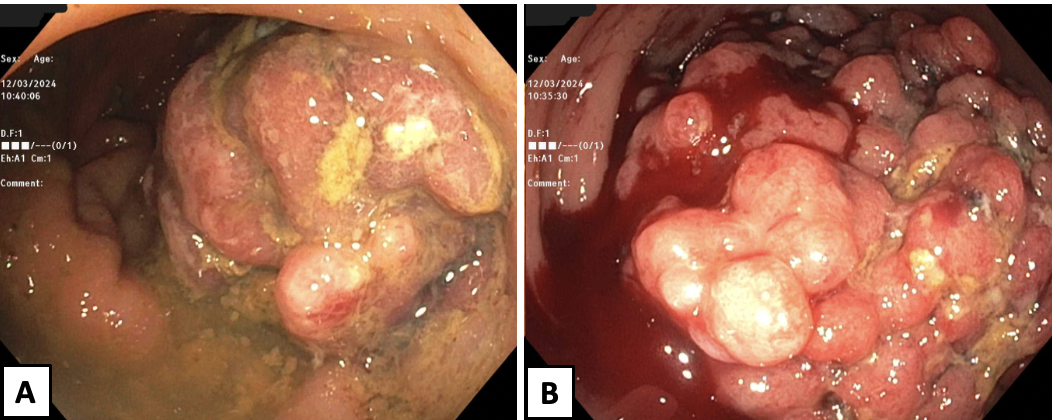
Figure: Figure 1. A. Partially obstructing mass in distal descending colon. B. Obstructing mass in proximal descending colon at which point scope could not be advanced and colonoscopy was aborted.
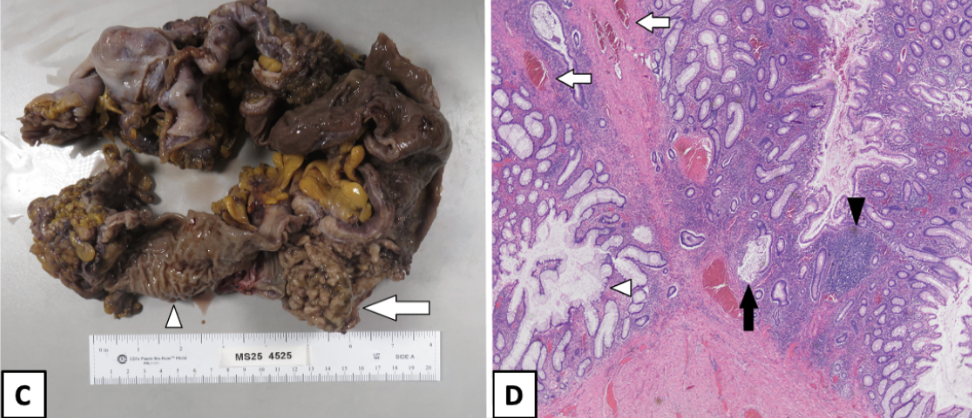
Figure: Figure 2. C. Gross photograph of a subtotal colectomy specimen demonstrating prominent exophytic inflammatory pseudopolyps (arrow), projecting above the denuded mucosal surface. Adjacent normal colonic mucosa (arrowhead) is shown for comparison. D. H&E-stained section (20×) from the base of an inflammatory pseudopolyp. The pseudopolyp is characterized by a crypt abscess with crypt rupture and mucin extravasation (solid arrow), a dense lymphoplasmacytic infiltrate (solid arrowhead), dilated crypts with distorted architecture (white arrowhead), and prominent thick-walled blood vessels (white arrows).
Disclosures:
Andrew Petrou indicated no relevant financial relationships.
Nicholas Scalzo indicated no relevant financial relationships.
Emily Romanoff indicated no relevant financial relationships.
Harlan Rich indicated no relevant financial relationships.
Sean Fine indicated no relevant financial relationships.
Michael Madrid indicated no relevant financial relationships.
Harry Rosenberg indicated no relevant financial relationships.
Andrew L. Petrou, MD1, Nicholas Scalzo, MD1, Emily L. Romanoff, MD1, Harlan G. Rich, MD2, Sean Fine, MD1, Michael Madrid, MD1, Harry Rosenberg, MD1. P5498 - Crohn’s Remission Gone Rogue: The Curious Case of Obstructing Giant Inflammatory Pseudopolyps, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
