Tuesday Poster Session
Category: IBD
P5497 - From Diverticular Disease to Ulcerative Colitis: A Case of Evolving Colonic Pathology
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Andrew L. Petrou, MD (he/him/his)
Brown University / Rhode Island Hospital
Providence, RI
Presenting Author(s)
Andrew L. Petrou, MD1, Grace Wilgucki, DO2, Audrey Ballard, MD1, Sean Fine, MD1
1Brown University / Rhode Island Hospital, Providence, RI; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Ulcerative colitis (UC) is characterized by mucosal inflammation of the colon, typically beginning in the rectum and extending proximally. While its etiology remains incompletely understood, UC is believed to arise from a complex interplay of genetic, environmental, and immunological factors. Diverticular disease, in contrast, is a common condition associated with localized colonic wall outpouchings. Here, we present an unusual case of a patient who developed refractory UC a few years following surgical resection for diverticular disease. To our knowledge, this constellation of clinical events has rarely been described, and this case contributes to a deeper understanding of overlapping gastrointestinal disease processes and their potential triggers.
Case Description/
Methods: A 36-year-old male with diverticulitis status post sigmoid colectomy in 2022, presented two years later with rectal bleeding and abdominal pain. On initial evaluation, fecal calprotectin was within normal limits; however, upon re-presentation, it was elevated to >3000 µg/g. Colonoscopy with biopsies revealed mucosal inflammation with histologic features consistent with UC. Initial management included corticosteroids and mesalamine, followed by a transition to ozanimod; however, he continued to endure symptoms of rectal bleeding, urgency and worsening abdominal pain. He required multiple courses of prednisone to maintain functionality. He failed treatment with Infliximab, and as a result, therapy was escalated to combination treatment with upadacitinib and vedolizumab. He is currently maintained on vedolizumab monotherapy with a favorable clinical response.
Discussion: This case illustrates a rare scenario: the development of refractory UC in a patient with no prior history of IBD, a few years after surgical intervention for complicated diverticular disease. At the time of the surgical resection, there was no clinical, endoscopic, or histopathological evidence of UC. The subsequent emergence of severe, treatment-resistant UC raises important considerations regarding pathogenesis, diagnosis, and management. In conclusion, this case contributes to a growing body of literature suggesting that colonic surgery, even when performed for non-IBD pathology, may in rare instances precede the development of chronic immune-mediated disease. Further research is needed to elucidate the mechanistic links between gut injury, microbial shifts, and immune activation, particularly in patients who develop de novo IBD after colonic resection.
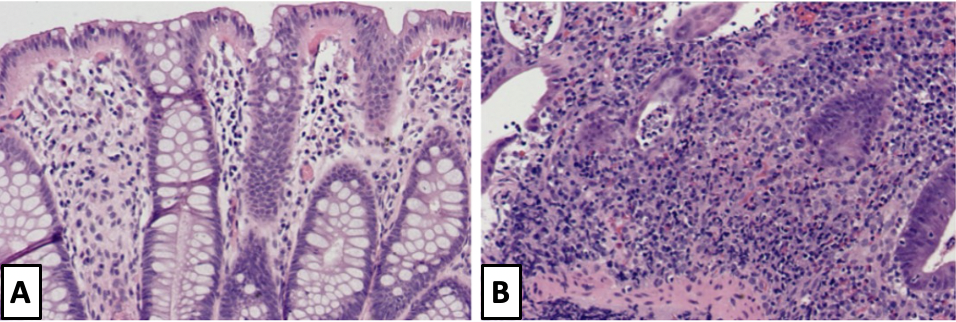
Figure: Figure 1. A. Histology of sigmoid colonic resection in 2022 demonstrating normal colonic mucosal architecture. B. Histology from biopsy of sigmoid colon taken during colonoscopy after presentation for abdominal pain and rectal bleeding with findings consistent with chronic mildly active colitis including crypt abscesses and epithelial cell neutrophil predominance.
Disclosures:
Andrew Petrou indicated no relevant financial relationships.
Grace Wilgucki indicated no relevant financial relationships.
Audrey Ballard indicated no relevant financial relationships.
Sean Fine indicated no relevant financial relationships.
Andrew L. Petrou, MD1, Grace Wilgucki, DO2, Audrey Ballard, MD1, Sean Fine, MD1. P5497 - From Diverticular Disease to Ulcerative Colitis: A Case of Evolving Colonic Pathology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brown University / Rhode Island Hospital, Providence, RI; 2Penn State Health Milton S. Hershey Medical Center, Hershey, PA
Introduction: Ulcerative colitis (UC) is characterized by mucosal inflammation of the colon, typically beginning in the rectum and extending proximally. While its etiology remains incompletely understood, UC is believed to arise from a complex interplay of genetic, environmental, and immunological factors. Diverticular disease, in contrast, is a common condition associated with localized colonic wall outpouchings. Here, we present an unusual case of a patient who developed refractory UC a few years following surgical resection for diverticular disease. To our knowledge, this constellation of clinical events has rarely been described, and this case contributes to a deeper understanding of overlapping gastrointestinal disease processes and their potential triggers.
Case Description/
Methods: A 36-year-old male with diverticulitis status post sigmoid colectomy in 2022, presented two years later with rectal bleeding and abdominal pain. On initial evaluation, fecal calprotectin was within normal limits; however, upon re-presentation, it was elevated to >3000 µg/g. Colonoscopy with biopsies revealed mucosal inflammation with histologic features consistent with UC. Initial management included corticosteroids and mesalamine, followed by a transition to ozanimod; however, he continued to endure symptoms of rectal bleeding, urgency and worsening abdominal pain. He required multiple courses of prednisone to maintain functionality. He failed treatment with Infliximab, and as a result, therapy was escalated to combination treatment with upadacitinib and vedolizumab. He is currently maintained on vedolizumab monotherapy with a favorable clinical response.
Discussion: This case illustrates a rare scenario: the development of refractory UC in a patient with no prior history of IBD, a few years after surgical intervention for complicated diverticular disease. At the time of the surgical resection, there was no clinical, endoscopic, or histopathological evidence of UC. The subsequent emergence of severe, treatment-resistant UC raises important considerations regarding pathogenesis, diagnosis, and management. In conclusion, this case contributes to a growing body of literature suggesting that colonic surgery, even when performed for non-IBD pathology, may in rare instances precede the development of chronic immune-mediated disease. Further research is needed to elucidate the mechanistic links between gut injury, microbial shifts, and immune activation, particularly in patients who develop de novo IBD after colonic resection.
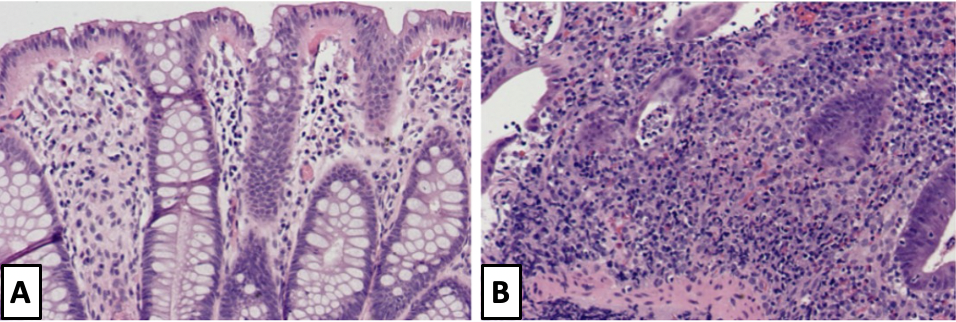
Figure: Figure 1. A. Histology of sigmoid colonic resection in 2022 demonstrating normal colonic mucosal architecture. B. Histology from biopsy of sigmoid colon taken during colonoscopy after presentation for abdominal pain and rectal bleeding with findings consistent with chronic mildly active colitis including crypt abscesses and epithelial cell neutrophil predominance.
Disclosures:
Andrew Petrou indicated no relevant financial relationships.
Grace Wilgucki indicated no relevant financial relationships.
Audrey Ballard indicated no relevant financial relationships.
Sean Fine indicated no relevant financial relationships.
Andrew L. Petrou, MD1, Grace Wilgucki, DO2, Audrey Ballard, MD1, Sean Fine, MD1. P5497 - From Diverticular Disease to Ulcerative Colitis: A Case of Evolving Colonic Pathology, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
