Tuesday Poster Session
Category: IBD
P5496 - A Stroke Too Soon: Embolic Event in a Young Patient Treated With Upadacitinib for Ulcerative Colitis - A Case for Caution?
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RC
Raja Chandra Chakinala, MD
Guthrie Robert Packer Hospital, Department of Gastroenterology
Sayre, PA
Presenting Author(s)
Raja Chandra Chakinala, MD1, Amlish Gondal, MD2, Arthur Cecchini, MD3, Shraddha Bhattarai, MD3, Matthew Lincoln, DO3
1Guthrie Robert Packer Hospital, Sayre, PA, Sayre, PA; 2Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 3Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Upadacitinib is an oral, selective Janus kinase 1 (JAK1) inhibitor approved for moderate to severe ulcerative colitis (UC). Its use is linked to increased risk of major adverse cardiovascular events (MACE)—including myocardial infarction and stroke—and venous thromboembolism (VTE), especially in patients aged 50 or older with at least one cardiovascular risk factor. However, limited safety data in UC patients have not shown a significant increase in MACE or VTE risk to date. We present a case of multifocal ischemic stroke in a young adult on Upadacitinib to raise clinical awareness of potential vascular complications.
Case Description/
Methods: A 46-year-old male non-smoker presented with headache, dizziness, nausea, and vomiting following a motor vehicle accident, preceded by visual blurring. His medical history included UC diagnosed 12 years earlier, GERD, and appendectomy. Notably, his mother died at a young age due to cerebral thrombosis.
He was initially managed with mesalamine for nine years. After clinical and endoscopic relapse, Adalimumab was initiated but discontinued after two years due to severe injection site reactions. Subsequently, Vedolizumab was started with good disease control; however, insurance formulary changes resulted in loss of coverage. Ustekinumab was prescribed but denied, leading to initiation of Upadacitinib. He completed an eight-week induction and was maintained on 15 mg daily until presentation.
Brain MRI showed multiple infarcts in bilateral cerebellar, right frontal, bilateral parietal, and right temporal lobes without large vessel occlusion or carotid stenosis (Figure 1). Cardiac workup including EKG, telemetry, and echocardiogram showed no arrhythmia or structural abnormalities. An emergent ventriculostomy was placed for hydrocephalus, but despite decompression, he developed tonsillar herniation requiring surgical resection of ischemic cerebellar tissue. Hospitalization was further complicated by segmental pulmonary embolism.
Discussion: Treatment selection for moderate-to-severe UC must balance efficacy, patient-specific risk profiles, and medication accessibility. This case underscores the importance of considering both personal and familial thrombotic history and adds to the limited literature on cerebrovascular events associated with JAK1 inhibitors in UC. The role of pre-treatment hypercoagulability testing warrants further investigation, as current hematology guidelines do not specifically address testing in patients with a family history of thrombosis.
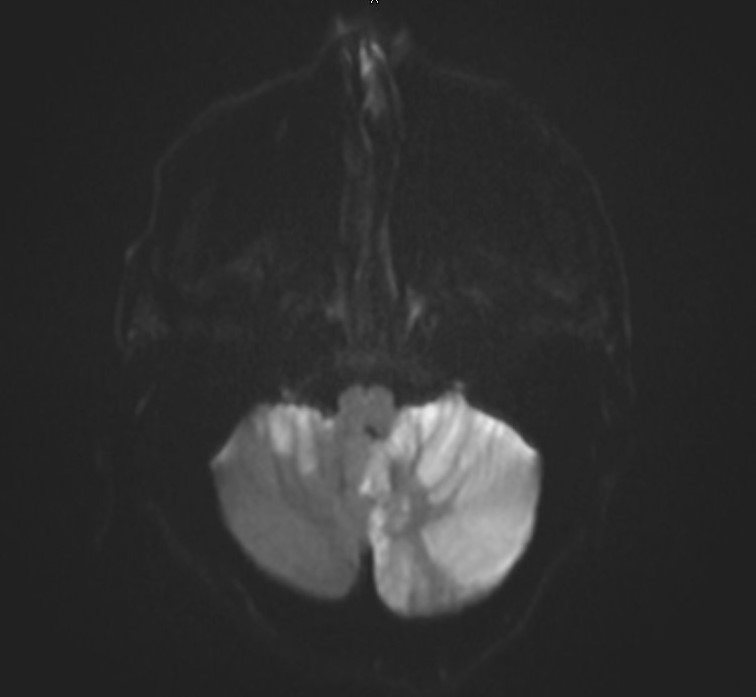
Figure: Diffusion-Weighted MRI indicating acute cerebellar infarction
Disclosures:
Raja Chandra Chakinala indicated no relevant financial relationships.
Amlish Gondal indicated no relevant financial relationships.
Arthur Cecchini indicated no relevant financial relationships.
Shraddha Bhattarai indicated no relevant financial relationships.
Matthew Lincoln indicated no relevant financial relationships.
Raja Chandra Chakinala, MD1, Amlish Gondal, MD2, Arthur Cecchini, MD3, Shraddha Bhattarai, MD3, Matthew Lincoln, DO3. P5496 - A Stroke Too Soon: Embolic Event in a Young Patient Treated With Upadacitinib for Ulcerative Colitis - A Case for Caution?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Guthrie Robert Packer Hospital, Sayre, PA, Sayre, PA; 2Guthrie Robert Packer Hospital, Department of Internal Medicine, Sayre, PA; 3Guthrie Robert Packer Hospital, Sayre, PA
Introduction: Upadacitinib is an oral, selective Janus kinase 1 (JAK1) inhibitor approved for moderate to severe ulcerative colitis (UC). Its use is linked to increased risk of major adverse cardiovascular events (MACE)—including myocardial infarction and stroke—and venous thromboembolism (VTE), especially in patients aged 50 or older with at least one cardiovascular risk factor. However, limited safety data in UC patients have not shown a significant increase in MACE or VTE risk to date. We present a case of multifocal ischemic stroke in a young adult on Upadacitinib to raise clinical awareness of potential vascular complications.
Case Description/
Methods: A 46-year-old male non-smoker presented with headache, dizziness, nausea, and vomiting following a motor vehicle accident, preceded by visual blurring. His medical history included UC diagnosed 12 years earlier, GERD, and appendectomy. Notably, his mother died at a young age due to cerebral thrombosis.
He was initially managed with mesalamine for nine years. After clinical and endoscopic relapse, Adalimumab was initiated but discontinued after two years due to severe injection site reactions. Subsequently, Vedolizumab was started with good disease control; however, insurance formulary changes resulted in loss of coverage. Ustekinumab was prescribed but denied, leading to initiation of Upadacitinib. He completed an eight-week induction and was maintained on 15 mg daily until presentation.
Brain MRI showed multiple infarcts in bilateral cerebellar, right frontal, bilateral parietal, and right temporal lobes without large vessel occlusion or carotid stenosis (Figure 1). Cardiac workup including EKG, telemetry, and echocardiogram showed no arrhythmia or structural abnormalities. An emergent ventriculostomy was placed for hydrocephalus, but despite decompression, he developed tonsillar herniation requiring surgical resection of ischemic cerebellar tissue. Hospitalization was further complicated by segmental pulmonary embolism.
Discussion: Treatment selection for moderate-to-severe UC must balance efficacy, patient-specific risk profiles, and medication accessibility. This case underscores the importance of considering both personal and familial thrombotic history and adds to the limited literature on cerebrovascular events associated with JAK1 inhibitors in UC. The role of pre-treatment hypercoagulability testing warrants further investigation, as current hematology guidelines do not specifically address testing in patients with a family history of thrombosis.
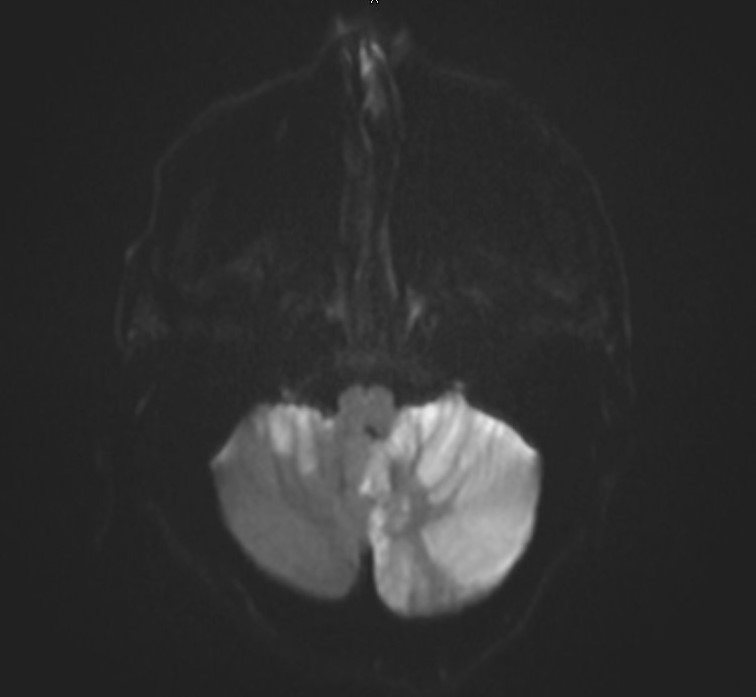
Figure: Diffusion-Weighted MRI indicating acute cerebellar infarction
Disclosures:
Raja Chandra Chakinala indicated no relevant financial relationships.
Amlish Gondal indicated no relevant financial relationships.
Arthur Cecchini indicated no relevant financial relationships.
Shraddha Bhattarai indicated no relevant financial relationships.
Matthew Lincoln indicated no relevant financial relationships.
Raja Chandra Chakinala, MD1, Amlish Gondal, MD2, Arthur Cecchini, MD3, Shraddha Bhattarai, MD3, Matthew Lincoln, DO3. P5496 - A Stroke Too Soon: Embolic Event in a Young Patient Treated With Upadacitinib for Ulcerative Colitis - A Case for Caution?, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
