Tuesday Poster Session
Category: IBD
P5494 - Intestinal Ultrasound-Assisted Endoscopic Management of Acute Bowel Obstruction in a Patient With Crohn’s Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Yusuke Miyatani, MD
University of Hawaii, John A. Burns School of Medicine, Department of Medicine
Honolulu, HI
Presenting Author(s)
Award: ACG Presidential Poster Award
Yusuke Miyatani, MD1, Natalie K. Choi, 2, Emma A. Picker, 2, Noa Krugliak Cleveland, MD2, David T. Rubin, MD3
1University of Hawaii, John A. Burns School of Medicine, Department of Medicine, Honolulu, HI; 2University of Chicago, Chicago, IL; 3University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL
Introduction: Endoscopic balloon dilation (EBD) is an established option for the management of fibrostenosing Crohn’s disease (CD). With the rise in intestinal ultrasound (IUS) utilization in the management of CD, there are opportunities to understand the pathophysiology of this condition and its treatment in new ways. We describe the first successful IUS-guided EBD in a patient with CD who presented with bowel obstruction.
Case Description/
Methods: A 27yo man with ileocolonic CD and ileocecectomy 11 years prior was in remission on infliximab when he presented with acute right lower quadrant (RLQ) abdominal pain, nausea, and vomiting after eating chicken and vegetables. Physical examination revealed tenderness in the RLQ without peritoneal signs. Point-of-care IUS demonstrated a 3 cm of stricture at the ileocolic anastomosis with bowel wall thickening (BWT, 4.8 mm), mild hyperemia (modified Limberg 1), narrowing of the lumen, proximal luminal dilation (2.6 cm), and preserved bowel wall stratification (Figure 1). There was no evidence of active inflammation elsewhere. Same-day colonoscopy (unprepped and unsedated) with EBD was performed. Endoscopy confirmed a stricture limited to the ileocolonic anastomosis without inflammation; vegetable matter was easily dislodged from the stenotic area. Endoscopic balloon dilation to 15 mm was performed, and relieved the obstruction and confirmed no active CD proximally. Post-dilation his symptoms resolved and same day repeat IUS showed improvement in upstream luminal dilation (2.1 cm). Over the next 2 weeks, serial IUS confirmed sustained resolution of proximal luminal dilation but no change in BWT or vascularity (Figure 2). At six months follow-up, he remains asymptomatic.
Discussion: We describe the first report of IUS-guided EBD and post-dilation serial monitoring with IUS in a patient with CD and anastomotic obstruction. IUS provided crucial and unique pre-procedural diagnostic detail, including the length of the stricture, absence of inflammatory features and allowed for both steroid- and ionizing radiation-sparing and same-day endoscopic management without hospitalization. The post-EBD persistent BWT suggests structural changes due to fibrosis rather than active inflammation. This case highlights IUS as a valuable adjunct for both diagnosis and follow-up tools, potentially providing us with an understanding of the pathogenesis in patients with stricturing CD.

Figure: Figure 1. Intestinal ultrasound of the stricture at the ileocolonic anastomosis (A), proximal dilation of the small bowel (B), bowel wall thickness (mm) at the site of the stricture (C), and color Doppler view demonstrating mild hyperemia (modified Limberg 1) (D).
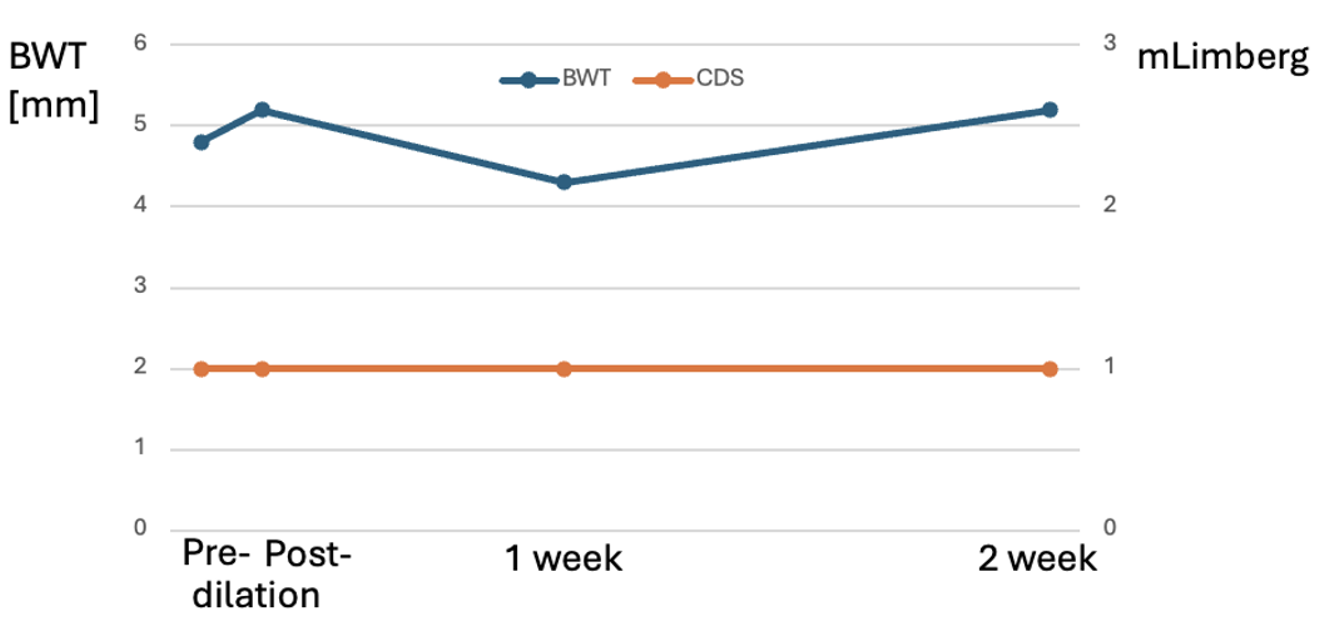
Figure: Figure 2. Longitudinal follow-up with intestinal ultrasound pre- and post-dilation with measurements of maximum bowel wall thickness (BWT) and color Doppler signal scored by modified Limberg score (mLimberg) at the anastomotic stricture.
Disclosures:
Yusuke Miyatani indicated no relevant financial relationships.
Natalie Choi indicated no relevant financial relationships.
Emma Picker indicated no relevant financial relationships.
Noa Krugliak Cleveland: Johnson & Johnson – Consultant. NueroLogica – Consultant.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Yusuke Miyatani, MD1, Natalie K. Choi, 2, Emma A. Picker, 2, Noa Krugliak Cleveland, MD2, David T. Rubin, MD3. P5494 - Intestinal Ultrasound-Assisted Endoscopic Management of Acute Bowel Obstruction in a Patient With Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Yusuke Miyatani, MD1, Natalie K. Choi, 2, Emma A. Picker, 2, Noa Krugliak Cleveland, MD2, David T. Rubin, MD3
1University of Hawaii, John A. Burns School of Medicine, Department of Medicine, Honolulu, HI; 2University of Chicago, Chicago, IL; 3University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL
Introduction: Endoscopic balloon dilation (EBD) is an established option for the management of fibrostenosing Crohn’s disease (CD). With the rise in intestinal ultrasound (IUS) utilization in the management of CD, there are opportunities to understand the pathophysiology of this condition and its treatment in new ways. We describe the first successful IUS-guided EBD in a patient with CD who presented with bowel obstruction.
Case Description/
Methods: A 27yo man with ileocolonic CD and ileocecectomy 11 years prior was in remission on infliximab when he presented with acute right lower quadrant (RLQ) abdominal pain, nausea, and vomiting after eating chicken and vegetables. Physical examination revealed tenderness in the RLQ without peritoneal signs. Point-of-care IUS demonstrated a 3 cm of stricture at the ileocolic anastomosis with bowel wall thickening (BWT, 4.8 mm), mild hyperemia (modified Limberg 1), narrowing of the lumen, proximal luminal dilation (2.6 cm), and preserved bowel wall stratification (Figure 1). There was no evidence of active inflammation elsewhere. Same-day colonoscopy (unprepped and unsedated) with EBD was performed. Endoscopy confirmed a stricture limited to the ileocolonic anastomosis without inflammation; vegetable matter was easily dislodged from the stenotic area. Endoscopic balloon dilation to 15 mm was performed, and relieved the obstruction and confirmed no active CD proximally. Post-dilation his symptoms resolved and same day repeat IUS showed improvement in upstream luminal dilation (2.1 cm). Over the next 2 weeks, serial IUS confirmed sustained resolution of proximal luminal dilation but no change in BWT or vascularity (Figure 2). At six months follow-up, he remains asymptomatic.
Discussion: We describe the first report of IUS-guided EBD and post-dilation serial monitoring with IUS in a patient with CD and anastomotic obstruction. IUS provided crucial and unique pre-procedural diagnostic detail, including the length of the stricture, absence of inflammatory features and allowed for both steroid- and ionizing radiation-sparing and same-day endoscopic management without hospitalization. The post-EBD persistent BWT suggests structural changes due to fibrosis rather than active inflammation. This case highlights IUS as a valuable adjunct for both diagnosis and follow-up tools, potentially providing us with an understanding of the pathogenesis in patients with stricturing CD.

Figure: Figure 1. Intestinal ultrasound of the stricture at the ileocolonic anastomosis (A), proximal dilation of the small bowel (B), bowel wall thickness (mm) at the site of the stricture (C), and color Doppler view demonstrating mild hyperemia (modified Limberg 1) (D).
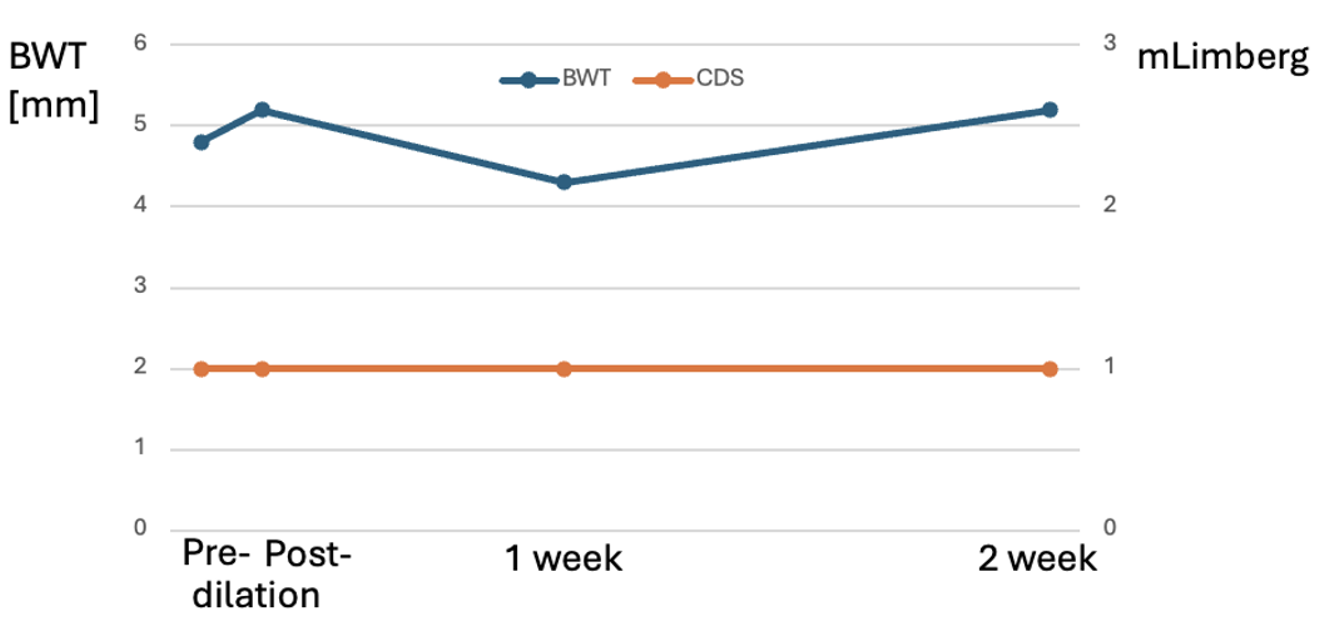
Figure: Figure 2. Longitudinal follow-up with intestinal ultrasound pre- and post-dilation with measurements of maximum bowel wall thickness (BWT) and color Doppler signal scored by modified Limberg score (mLimberg) at the anastomotic stricture.
Disclosures:
Yusuke Miyatani indicated no relevant financial relationships.
Natalie Choi indicated no relevant financial relationships.
Emma Picker indicated no relevant financial relationships.
Noa Krugliak Cleveland: Johnson & Johnson – Consultant. NueroLogica – Consultant.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Yusuke Miyatani, MD1, Natalie K. Choi, 2, Emma A. Picker, 2, Noa Krugliak Cleveland, MD2, David T. Rubin, MD3. P5494 - Intestinal Ultrasound-Assisted Endoscopic Management of Acute Bowel Obstruction in a Patient With Crohn’s Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

