Tuesday Poster Session
Category: Interventional Endoscopy
P5679 - Cold Endoscopic Mucosal Resection vs Hot Endoscopic Mucosal Resection for Large Colonic Polyp (>20mm): A Two-Center Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OK
Osama Sherjeel Khan, MD (he/him/his)
Cleveland Clinic Florida
Weston, FL
Presenting Author(s)
Osama Sherjeel Khan, MD1, William King, MD2, Akram I. Ahmad, MD1, Michael Ladna, MD3, Zaid Ansari, MD1, Logan Wright, MS4, Mamoon Rashid, MD5, Hameed Ullah, MD6, Tolga Erim, DO1, Bashar Qumseya, MD, MPH7
1Cleveland Clinic Florida, Weston, FL; 2University of Florida, Gainesville, FL; 3University of California Davis Health, Davis, CA; 4University of Central Florida College of Medicine, Gainesville, FL; 5Borland Groover, Jacksonville, FL; 6St. Luke's Hospital, Chesterfield, MO; 7University of Florida College of Medicine, Gainesville, FL
Introduction: Cold endoscopic mucosal resection (EMR) has recently emerged as a potentially safer alternative to traditional hot EMR with electrocautery. We therefore aimed to compare the safety and efficacy of cold versus hot EMR for large (≥20 mm) nonpedunculated colorectal polyps in a multicenter retrospective cohort study.
Methods: We conducted a retrospective cohort study at two U.S. tertiary centers. Included were patients who underwent EMR for a polyp at least 20 mm and had a documented follow-up colonoscopy. We excluded patients who underwent surgery, ESD, or polypectomy without submucosal injection or water immersion. EMR technique (cold vs hot) was determined by the endoscopist. The primary outcome was a composite of bleeding and perforation. Secondary outcomes included early and delayed bleeding, recurrence, and predictors of adverse events. Multivariate logistic regression was used to identify independent predictors of bleeding and recurrence.
Results: A total of 764 patients met inclusion criteria; 414 underwent hot EMR and 350 cold EMR. Composite adverse events were more common with hot EMR (10.6% vs 4.0%; univariate OR 2.43, 95% CI 1.29–4.56, p=0.01). Hot EMR was associated with higher overall bleeding (9.1% vs 4.0%; OR 2.15, 95% CI 1.13–4.07, p=0.019), early bleeding (3.6% vs 0.8%; OR 4.35, 95% CI 1.25–15.15, p=0.021), and perforation, although this was not significant (1.4% vs 0%, p=0.99). On univariate analysis, there was a trend towards more recurrence in the cold EMR group (22.6% vs 16.5%; OR 0.67, 95% CI 0.43–1.07, p=0.091). Cold EMR was associated with a significantly shorter median procedure duration compared to hot EMR (44 vs. 52 mins, p < 0.001). On multivariate analysis, cold EMR was independently associated with recurrence (OR 0.12, 95% CI 0.04–0.33, p< 0.001). Rectal location was independently associated with bleeding (OR 3.93, 95% CI 3.18–4.22, p=0.03).
Discussion: Cold EMR offers a significantly improved safety profile compared to hot EMR, with lower rates of bleeding and perforation. Although recurrence rates may be slightly higher with cold EMR, the difference is modest and offset by its superior safety, making cold EMR a favorable option for resection of large nonpedunculated colorectal polyps, especially in high-risk patients or anatomically sensitive locations
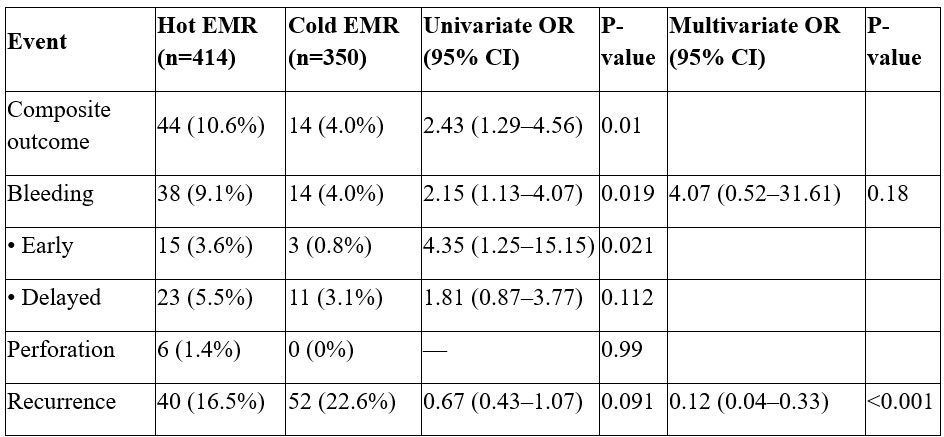
Figure: Table 1. Baseline Patient Characteristics
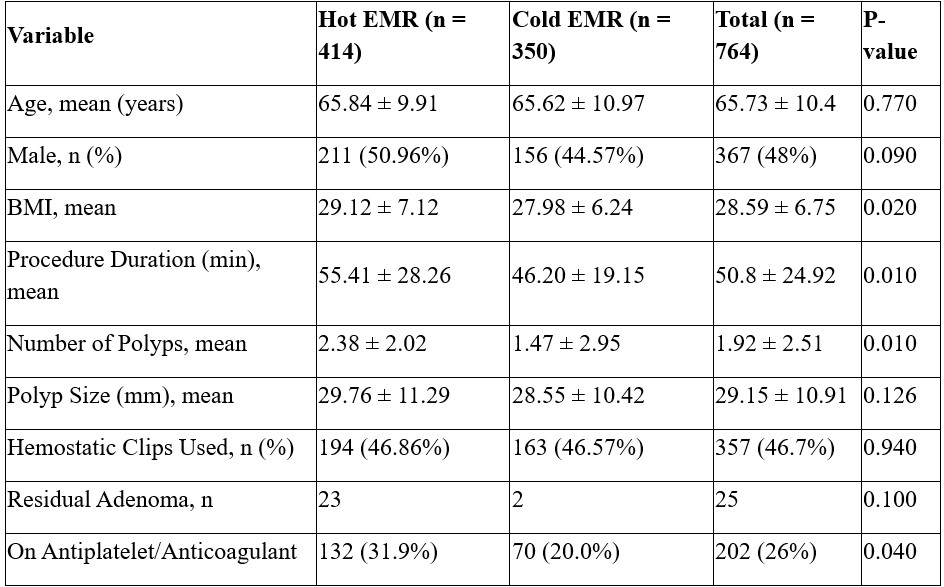
Figure: Table 2. Primary and secondary outcomes (univariate and multivariate analysis)
Disclosures:
Osama Sherjeel Khan indicated no relevant financial relationships.
William King indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Michael Ladna indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Logan Wright indicated no relevant financial relationships.
Mamoon Rashid indicated no relevant financial relationships.
Hameed Ullah indicated no relevant financial relationships.
Tolga Erim indicated no relevant financial relationships.
Bashar Qumseya: Assertio Management – Consultant. Castle Biosciences – Food and beverage compensation. Endogastric Solutions – Consultant. Medtronic – Consultant.
Osama Sherjeel Khan, MD1, William King, MD2, Akram I. Ahmad, MD1, Michael Ladna, MD3, Zaid Ansari, MD1, Logan Wright, MS4, Mamoon Rashid, MD5, Hameed Ullah, MD6, Tolga Erim, DO1, Bashar Qumseya, MD, MPH7. P5679 - Cold Endoscopic Mucosal Resection vs Hot Endoscopic Mucosal Resection for Large Colonic Polyp (>20mm): A Two-Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic Florida, Weston, FL; 2University of Florida, Gainesville, FL; 3University of California Davis Health, Davis, CA; 4University of Central Florida College of Medicine, Gainesville, FL; 5Borland Groover, Jacksonville, FL; 6St. Luke's Hospital, Chesterfield, MO; 7University of Florida College of Medicine, Gainesville, FL
Introduction: Cold endoscopic mucosal resection (EMR) has recently emerged as a potentially safer alternative to traditional hot EMR with electrocautery. We therefore aimed to compare the safety and efficacy of cold versus hot EMR for large (≥20 mm) nonpedunculated colorectal polyps in a multicenter retrospective cohort study.
Methods: We conducted a retrospective cohort study at two U.S. tertiary centers. Included were patients who underwent EMR for a polyp at least 20 mm and had a documented follow-up colonoscopy. We excluded patients who underwent surgery, ESD, or polypectomy without submucosal injection or water immersion. EMR technique (cold vs hot) was determined by the endoscopist. The primary outcome was a composite of bleeding and perforation. Secondary outcomes included early and delayed bleeding, recurrence, and predictors of adverse events. Multivariate logistic regression was used to identify independent predictors of bleeding and recurrence.
Results: A total of 764 patients met inclusion criteria; 414 underwent hot EMR and 350 cold EMR. Composite adverse events were more common with hot EMR (10.6% vs 4.0%; univariate OR 2.43, 95% CI 1.29–4.56, p=0.01). Hot EMR was associated with higher overall bleeding (9.1% vs 4.0%; OR 2.15, 95% CI 1.13–4.07, p=0.019), early bleeding (3.6% vs 0.8%; OR 4.35, 95% CI 1.25–15.15, p=0.021), and perforation, although this was not significant (1.4% vs 0%, p=0.99). On univariate analysis, there was a trend towards more recurrence in the cold EMR group (22.6% vs 16.5%; OR 0.67, 95% CI 0.43–1.07, p=0.091). Cold EMR was associated with a significantly shorter median procedure duration compared to hot EMR (44 vs. 52 mins, p < 0.001). On multivariate analysis, cold EMR was independently associated with recurrence (OR 0.12, 95% CI 0.04–0.33, p< 0.001). Rectal location was independently associated with bleeding (OR 3.93, 95% CI 3.18–4.22, p=0.03).
Discussion: Cold EMR offers a significantly improved safety profile compared to hot EMR, with lower rates of bleeding and perforation. Although recurrence rates may be slightly higher with cold EMR, the difference is modest and offset by its superior safety, making cold EMR a favorable option for resection of large nonpedunculated colorectal polyps, especially in high-risk patients or anatomically sensitive locations
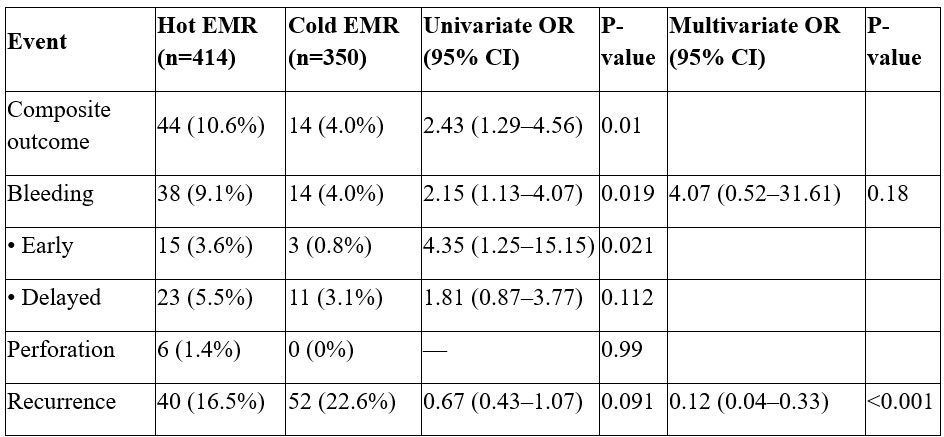
Figure: Table 1. Baseline Patient Characteristics
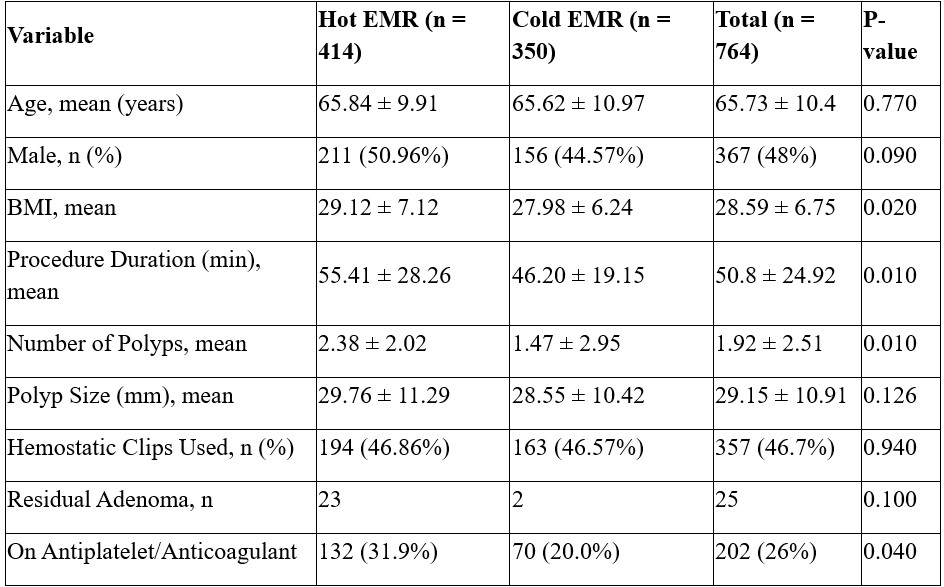
Figure: Table 2. Primary and secondary outcomes (univariate and multivariate analysis)
Disclosures:
Osama Sherjeel Khan indicated no relevant financial relationships.
William King indicated no relevant financial relationships.
Akram Ahmad indicated no relevant financial relationships.
Michael Ladna indicated no relevant financial relationships.
Zaid Ansari indicated no relevant financial relationships.
Logan Wright indicated no relevant financial relationships.
Mamoon Rashid indicated no relevant financial relationships.
Hameed Ullah indicated no relevant financial relationships.
Tolga Erim indicated no relevant financial relationships.
Bashar Qumseya: Assertio Management – Consultant. Castle Biosciences – Food and beverage compensation. Endogastric Solutions – Consultant. Medtronic – Consultant.
Osama Sherjeel Khan, MD1, William King, MD2, Akram I. Ahmad, MD1, Michael Ladna, MD3, Zaid Ansari, MD1, Logan Wright, MS4, Mamoon Rashid, MD5, Hameed Ullah, MD6, Tolga Erim, DO1, Bashar Qumseya, MD, MPH7. P5679 - Cold Endoscopic Mucosal Resection vs Hot Endoscopic Mucosal Resection for Large Colonic Polyp (>20mm): A Two-Center Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
