Tuesday Poster Session
Category: Interventional Endoscopy
P5678 - Endoscopic Submucosal Dissection vs Endoscopic Mucosal Resection for T1a and T1b Colorectal Cancer: A Meta-Analysis of Outcomes and Complications
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abu Abbasi, MD
Mercyhealth Gastroenterology Fellowship
Rockford, IL
Presenting Author(s)
Abu Fahad Abbasi, MD1, Luqman Baloch, MD1, Abdulmalik Saleem, MD2, Ahmet Sakiri, MD3, Vishali Moond, MD4, Abdul Mubeen Khan, MD1, Altaf Dawood, MD5, Naser Khan, MD5, Baseer Qazi, MD5, Babu P. Mohan, MD6, Douglas G. Adler, MD, FACG7
1Mercyhealth Gastroenterology Fellowship, Rockford, IL; 2Henry Ford Health, Detroit, MI; 3Mercyhealth Internal Medicine Residency, Rockford, IL; 4Saint Peter's University Hospital/Robert Wood Johnson Medical School loc, New Brunswick, NJ; 5Mercyhealth Gastroenterology, Rockford, IL; 6Orlando Gastroenterology PA, Orlando, FL; 7Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are widely used techniques for managing T1a and T1b colorectal cancer lesions. This meta-analysis evaluates and compares the outcomes of EMR and ESD, focusing on recurrence, en bloc resection, perforation, and bleeding rates.
Methods: A systematic review and meta-analysis were conducted per PRISMA guidelines. Studies reporting on ESD and EMR in localized, non-invasive colorectal lesions and reporting at least one outcome were included. Databases searched included PubMed, Embase, Cochrane, and Web of Science, using the search strategy. Standard meta-analysis methods using Random-effects models were used to calculate pooled results, and heterogeneity was assessed with I statistics.
Results: ESD demonstrated a significantly lower recurrence rate of 0.9% (95% CI: [0.6-1.6; I = 0%]) compared to EMR at 6.8% [(95% CI: 3.7–12.2; I = 83%; P < 0.01]). ESD achieved a higher en bloc resection rate of 93.6% (95% CI: 91.5%–95.2%; I = 54%; 11 studies) versus EMR at 70.0% (95% CI: 42.2%–89.2%; I = 98%; 11 studies; P = 0.005). Bleeding rates were lower with ESD (2.0%; 95% CI: 0.9%–4.1%; I = 71%; 10 studies) compared to EMR (5.2%; 95% CI: 3.6%–7.6%; I = 54%; 8 studies; P = 0.021). However, perforation rates were higher for ESD at 4.6% (95% CI: 2.6%–8.1%; I = 80%; 10 studies) compared to EMR at 1.1% (95% CI: 0.6%–2.2%; I = 18%; 8 studies; P = 0.02). The pooled rates are summarized in Table 1.
Discussion: This meta-analysis highlights ESD’s superiority over EMR in achieving lower recurrence and higher en bloc resection rates, reinforcing its role as the preferred technique for managing early-stage colorectal cancer. However, ESD’s higher perforation rates underline the importance of advanced endoscopic expertise and careful patient selection. Interestingly, ESD showed significantly lower bleeding rates, likely due to its precise submucosal dissection technique with enhanced visualization and hemostatic control. Limitations include substantial heterogeneity in EMR outcomes, potentially due to variations in study designs and lesion-specific characteristics. Meanwhile, statistical analysis was verified with the help AI software chatGPT. Overall, ESD provides better oncological outcomes but demands specialized training to mitigate its higher procedural risks. Future head-to-head direct studies are warranted to establish our findings.
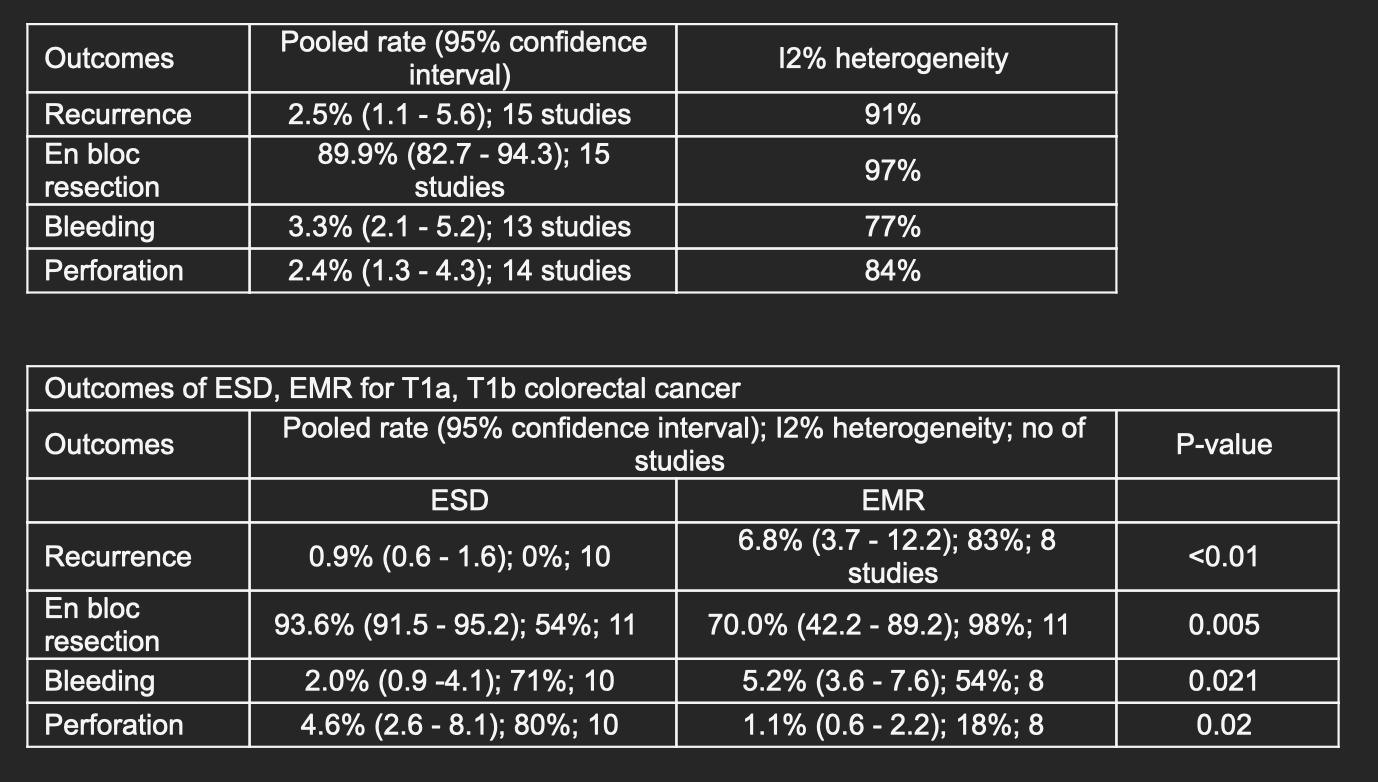
Figure: Outcome Data Tables
Disclosures:
Abu Fahad Abbasi indicated no relevant financial relationships.
Luqman Baloch indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Ahmet Sakiri indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Abdul Mubeen Khan indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Douglas Adler: Boston Scientific – Consultant.
Abu Fahad Abbasi, MD1, Luqman Baloch, MD1, Abdulmalik Saleem, MD2, Ahmet Sakiri, MD3, Vishali Moond, MD4, Abdul Mubeen Khan, MD1, Altaf Dawood, MD5, Naser Khan, MD5, Baseer Qazi, MD5, Babu P. Mohan, MD6, Douglas G. Adler, MD, FACG7. P5678 - Endoscopic Submucosal Dissection vs Endoscopic Mucosal Resection for T1a and T1b Colorectal Cancer: A Meta-Analysis of Outcomes and Complications, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mercyhealth Gastroenterology Fellowship, Rockford, IL; 2Henry Ford Health, Detroit, MI; 3Mercyhealth Internal Medicine Residency, Rockford, IL; 4Saint Peter's University Hospital/Robert Wood Johnson Medical School loc, New Brunswick, NJ; 5Mercyhealth Gastroenterology, Rockford, IL; 6Orlando Gastroenterology PA, Orlando, FL; 7Center for Advanced Therapeutic (CATE), Centura Health, Porter Adventist Hospital, Peak Gastroenterology, Denver, CO
Introduction: Endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD) are widely used techniques for managing T1a and T1b colorectal cancer lesions. This meta-analysis evaluates and compares the outcomes of EMR and ESD, focusing on recurrence, en bloc resection, perforation, and bleeding rates.
Methods: A systematic review and meta-analysis were conducted per PRISMA guidelines. Studies reporting on ESD and EMR in localized, non-invasive colorectal lesions and reporting at least one outcome were included. Databases searched included PubMed, Embase, Cochrane, and Web of Science, using the search strategy. Standard meta-analysis methods using Random-effects models were used to calculate pooled results, and heterogeneity was assessed with I statistics.
Results: ESD demonstrated a significantly lower recurrence rate of 0.9% (95% CI: [0.6-1.6; I = 0%]) compared to EMR at 6.8% [(95% CI: 3.7–12.2; I = 83%; P < 0.01]). ESD achieved a higher en bloc resection rate of 93.6% (95% CI: 91.5%–95.2%; I = 54%; 11 studies) versus EMR at 70.0% (95% CI: 42.2%–89.2%; I = 98%; 11 studies; P = 0.005). Bleeding rates were lower with ESD (2.0%; 95% CI: 0.9%–4.1%; I = 71%; 10 studies) compared to EMR (5.2%; 95% CI: 3.6%–7.6%; I = 54%; 8 studies; P = 0.021). However, perforation rates were higher for ESD at 4.6% (95% CI: 2.6%–8.1%; I = 80%; 10 studies) compared to EMR at 1.1% (95% CI: 0.6%–2.2%; I = 18%; 8 studies; P = 0.02). The pooled rates are summarized in Table 1.
Discussion: This meta-analysis highlights ESD’s superiority over EMR in achieving lower recurrence and higher en bloc resection rates, reinforcing its role as the preferred technique for managing early-stage colorectal cancer. However, ESD’s higher perforation rates underline the importance of advanced endoscopic expertise and careful patient selection. Interestingly, ESD showed significantly lower bleeding rates, likely due to its precise submucosal dissection technique with enhanced visualization and hemostatic control. Limitations include substantial heterogeneity in EMR outcomes, potentially due to variations in study designs and lesion-specific characteristics. Meanwhile, statistical analysis was verified with the help AI software chatGPT. Overall, ESD provides better oncological outcomes but demands specialized training to mitigate its higher procedural risks. Future head-to-head direct studies are warranted to establish our findings.
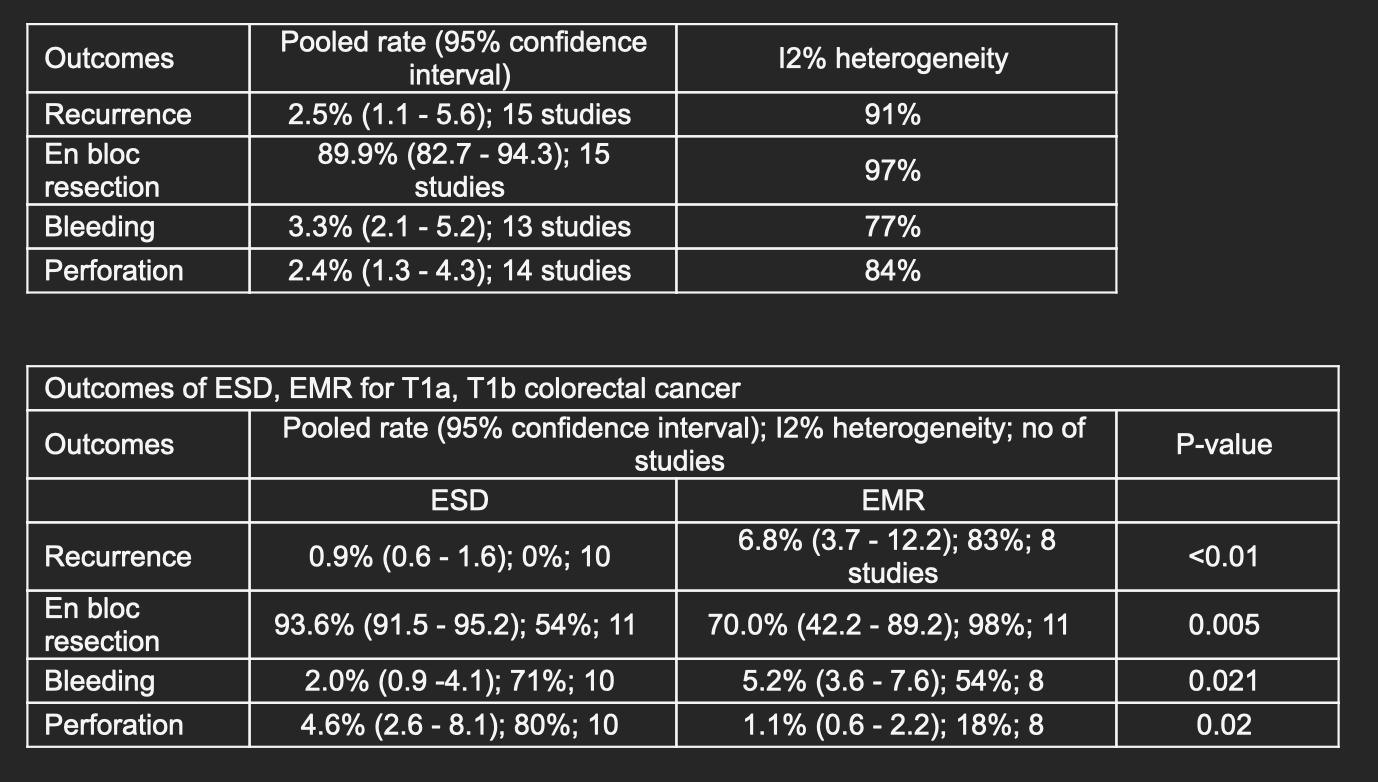
Figure: Outcome Data Tables
Disclosures:
Abu Fahad Abbasi indicated no relevant financial relationships.
Luqman Baloch indicated no relevant financial relationships.
Abdulmalik Saleem indicated no relevant financial relationships.
Ahmet Sakiri indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Abdul Mubeen Khan indicated no relevant financial relationships.
Altaf Dawood indicated no relevant financial relationships.
Naser Khan indicated no relevant financial relationships.
Baseer Qazi indicated no relevant financial relationships.
Babu Mohan indicated no relevant financial relationships.
Douglas Adler: Boston Scientific – Consultant.
Abu Fahad Abbasi, MD1, Luqman Baloch, MD1, Abdulmalik Saleem, MD2, Ahmet Sakiri, MD3, Vishali Moond, MD4, Abdul Mubeen Khan, MD1, Altaf Dawood, MD5, Naser Khan, MD5, Baseer Qazi, MD5, Babu P. Mohan, MD6, Douglas G. Adler, MD, FACG7. P5678 - Endoscopic Submucosal Dissection vs Endoscopic Mucosal Resection for T1a and T1b Colorectal Cancer: A Meta-Analysis of Outcomes and Complications, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
