Tuesday Poster Session
Category: Interventional Endoscopy
P5663 - Primary EUS-Guided Biliary Drainage Compared to ERCP for Malignant Biliary Obstruction: A Meta-Analysis of Randomized Controlled Trials
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Saqr Alsakarneh, MD, MS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Saqr Alsakarneh, MD, MS1, Osama Asad, MD2, Razan Aburumman, MD3, Yassine Kilani, MD4, Mohamad Adam, MD2, Dushyant S. Dahiya, MD5, Mohammad Bilal, MD, FACG6
1Mayo Clinic, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Henry Ford Health, Detroit, MI; 4Saint Louis University, Saint Louis, MO; 5University of Kansas School of Medicine, Kansas City, KS; 6University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Endoscopic ultrasound guided biliary drainage (EUS-BD) is an emerging technique for biliary decompression in malignant biliary obstruction (MBO). EUS-BD has been historically used as rescue therapy when ERCP fails. However, recent studies suggested its efficacy in the initial management of MBO. We aimed to compare the efficacy and safety of EUS vs ERCP when used as the primary modality for biliary decompression in MBO.
Methods: A systematic search of MEDLINE, Embase, and Cochrane databases, from inception to May 25, 2025, was conducted for randomized controlled trials (RCTs) comparing EUS and ERCP as the primary modality for MBO. Primary outcomes were technical and clinical success rates. Secondary outcomes included stent patency, reintervention, risk of post-procedure pancreatitis (PPP), overall adverse events (AEs), cholangitis, tumor in/overgrowth, procedure time, length of hospital stay (LOS), and survival time. Risk ratios (RR) with 95% confidence intervals (CI) were calculated for dichotomous outcomes, using a random-effects model. Heterogeneity was assessed using I2 statistics. Technical success was defined as the successful placement of stent, whereas clinical success defined as ≥50% reduction in serum bilirubin.
Results: A total of 8 RCTs were included (807 patients). There were no significant differences between both groups in technical success (RR=1.06; 95% CI: 0.96-1.17) or clinical success (RR=1.02; 95% CI: 0.98-1.06) [Figure 1]. However, EUS-BD was associated with lower risk of PPP (RR=0.19; 95% CI: 0.08-0.46) compared to ERCP with no heterogeneity between studies (I2=0%). There was no statistically significant difference in terms of stent patency (MD=8.2; 95% CI: -40.7-57.1), over all AEs (RR=0.65; 95% CI: 0.23-1.87) or cholangitis (RR=1.19; 95% CI: 0.39-3.61) [Table 1].
However, the risk of reintervention (RR=0.53; 95% CI: 0.29-0.96) and tumor in/overgrowth (RR=0.28; 95% CI: 0.11-0.70) were significantly lower in the EUS-BD group. Additionally, EUS-BD group had shorter procedure time (MD= -7.69; 95% CI: -13.89 to -1.49) and hospital stay (MD= -1.03; 95% CI: -1.53 to -0.53) compared to ERCP-BD.
Discussion: Our meta-analysis demonstrates that EUS-BD has similar technical and clinical success to ERCP in managing MBO, with lower rates of PPP as expected. However, these data are from expert endoscopists, and future real-world studies looking at learning curves of EUS-BD and surgical outcomes following EUS-BD are needed prior to considering EUS-BD as first line therapy for MBO.
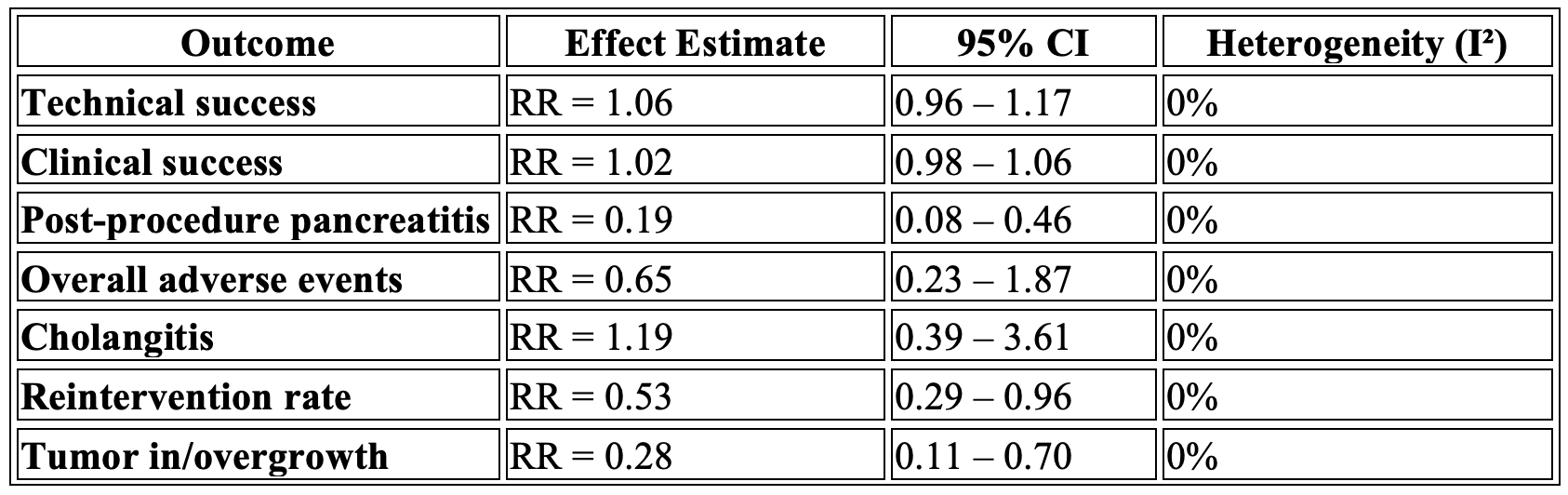
Figure: Figure 1. Forest Plot Of Technical And Clinical Success Rates
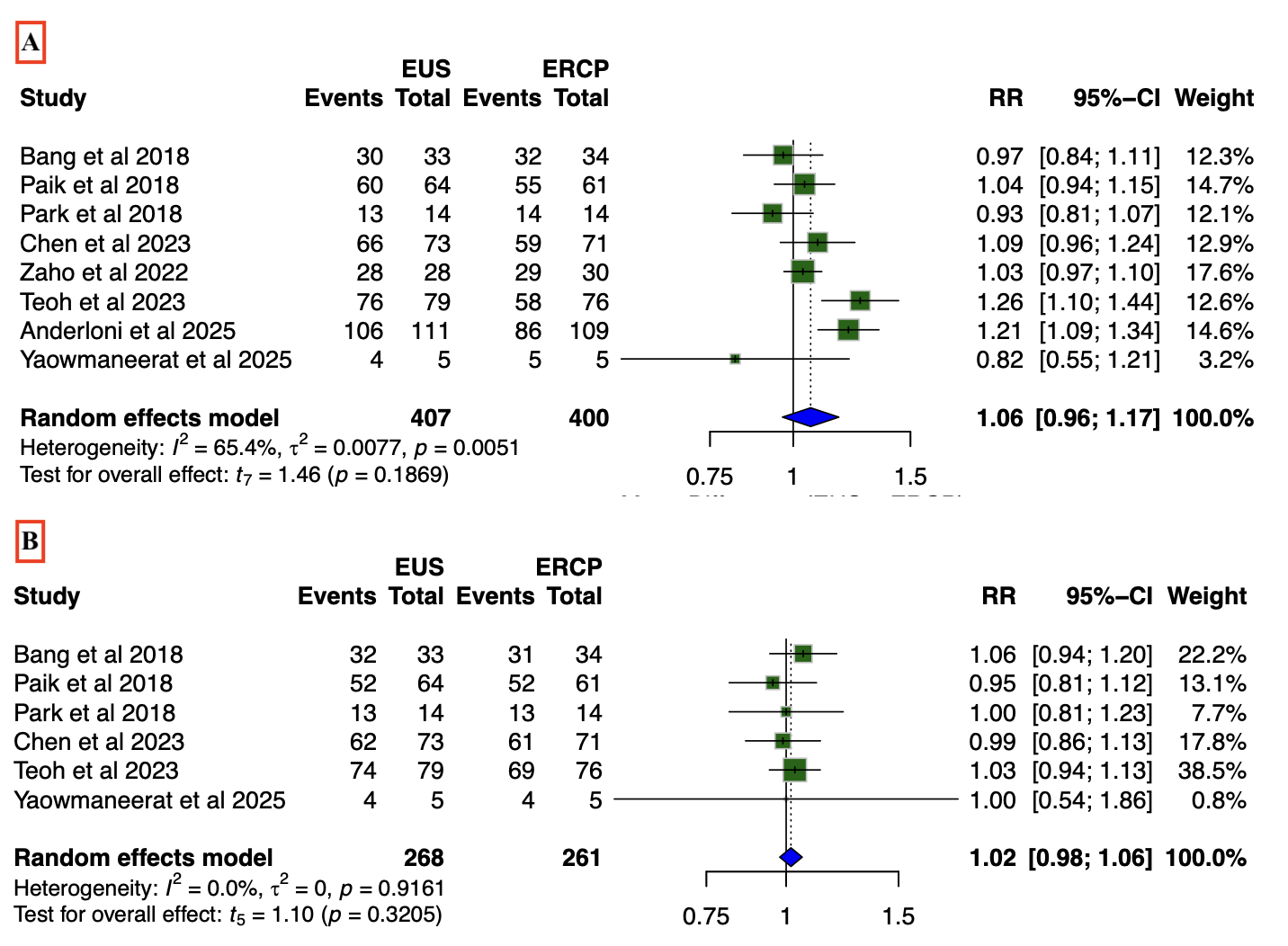
Figure: Table 1. Comparative Outcomes of EUS-BD versus ERCP-BD in Malignant Biliary Obstruction
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Osama Asad indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Mohamad Adam indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Saqr Alsakarneh, MD, MS1, Osama Asad, MD2, Razan Aburumman, MD3, Yassine Kilani, MD4, Mohamad Adam, MD2, Dushyant S. Dahiya, MD5, Mohammad Bilal, MD, FACG6. P5663 - Primary EUS-Guided Biliary Drainage Compared to ERCP for Malignant Biliary Obstruction: A Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Henry Ford Health, Detroit, MI; 4Saint Louis University, Saint Louis, MO; 5University of Kansas School of Medicine, Kansas City, KS; 6University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Endoscopic ultrasound guided biliary drainage (EUS-BD) is an emerging technique for biliary decompression in malignant biliary obstruction (MBO). EUS-BD has been historically used as rescue therapy when ERCP fails. However, recent studies suggested its efficacy in the initial management of MBO. We aimed to compare the efficacy and safety of EUS vs ERCP when used as the primary modality for biliary decompression in MBO.
Methods: A systematic search of MEDLINE, Embase, and Cochrane databases, from inception to May 25, 2025, was conducted for randomized controlled trials (RCTs) comparing EUS and ERCP as the primary modality for MBO. Primary outcomes were technical and clinical success rates. Secondary outcomes included stent patency, reintervention, risk of post-procedure pancreatitis (PPP), overall adverse events (AEs), cholangitis, tumor in/overgrowth, procedure time, length of hospital stay (LOS), and survival time. Risk ratios (RR) with 95% confidence intervals (CI) were calculated for dichotomous outcomes, using a random-effects model. Heterogeneity was assessed using I2 statistics. Technical success was defined as the successful placement of stent, whereas clinical success defined as ≥50% reduction in serum bilirubin.
Results: A total of 8 RCTs were included (807 patients). There were no significant differences between both groups in technical success (RR=1.06; 95% CI: 0.96-1.17) or clinical success (RR=1.02; 95% CI: 0.98-1.06) [Figure 1]. However, EUS-BD was associated with lower risk of PPP (RR=0.19; 95% CI: 0.08-0.46) compared to ERCP with no heterogeneity between studies (I2=0%). There was no statistically significant difference in terms of stent patency (MD=8.2; 95% CI: -40.7-57.1), over all AEs (RR=0.65; 95% CI: 0.23-1.87) or cholangitis (RR=1.19; 95% CI: 0.39-3.61) [Table 1].
However, the risk of reintervention (RR=0.53; 95% CI: 0.29-0.96) and tumor in/overgrowth (RR=0.28; 95% CI: 0.11-0.70) were significantly lower in the EUS-BD group. Additionally, EUS-BD group had shorter procedure time (MD= -7.69; 95% CI: -13.89 to -1.49) and hospital stay (MD= -1.03; 95% CI: -1.53 to -0.53) compared to ERCP-BD.
Discussion: Our meta-analysis demonstrates that EUS-BD has similar technical and clinical success to ERCP in managing MBO, with lower rates of PPP as expected. However, these data are from expert endoscopists, and future real-world studies looking at learning curves of EUS-BD and surgical outcomes following EUS-BD are needed prior to considering EUS-BD as first line therapy for MBO.
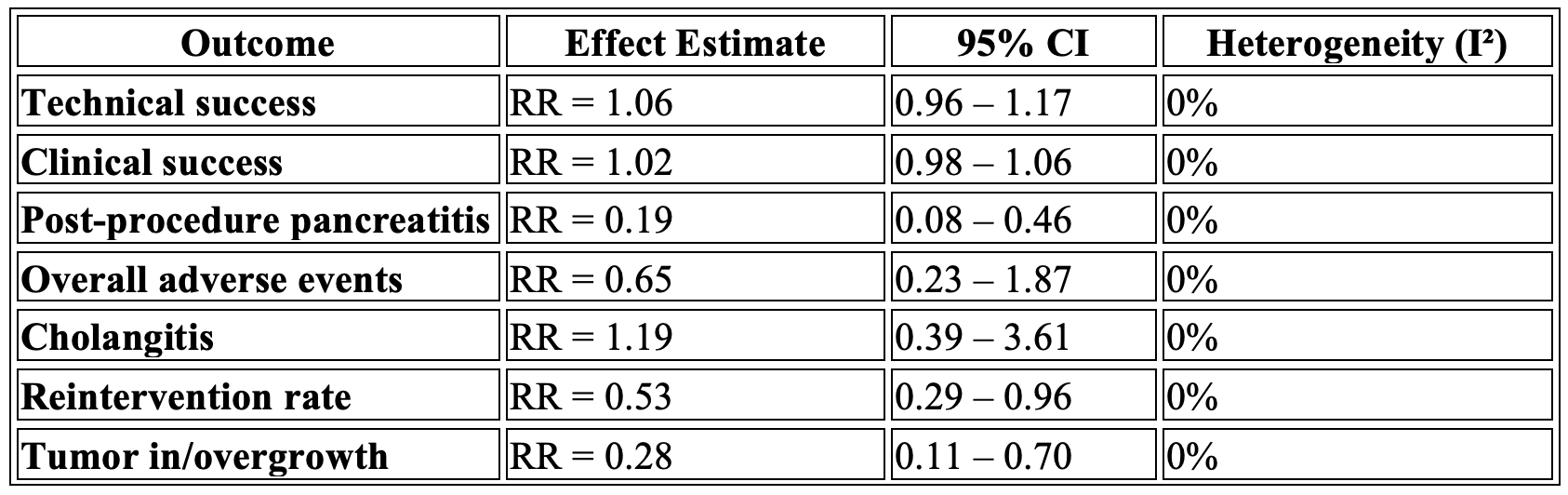
Figure: Figure 1. Forest Plot Of Technical And Clinical Success Rates
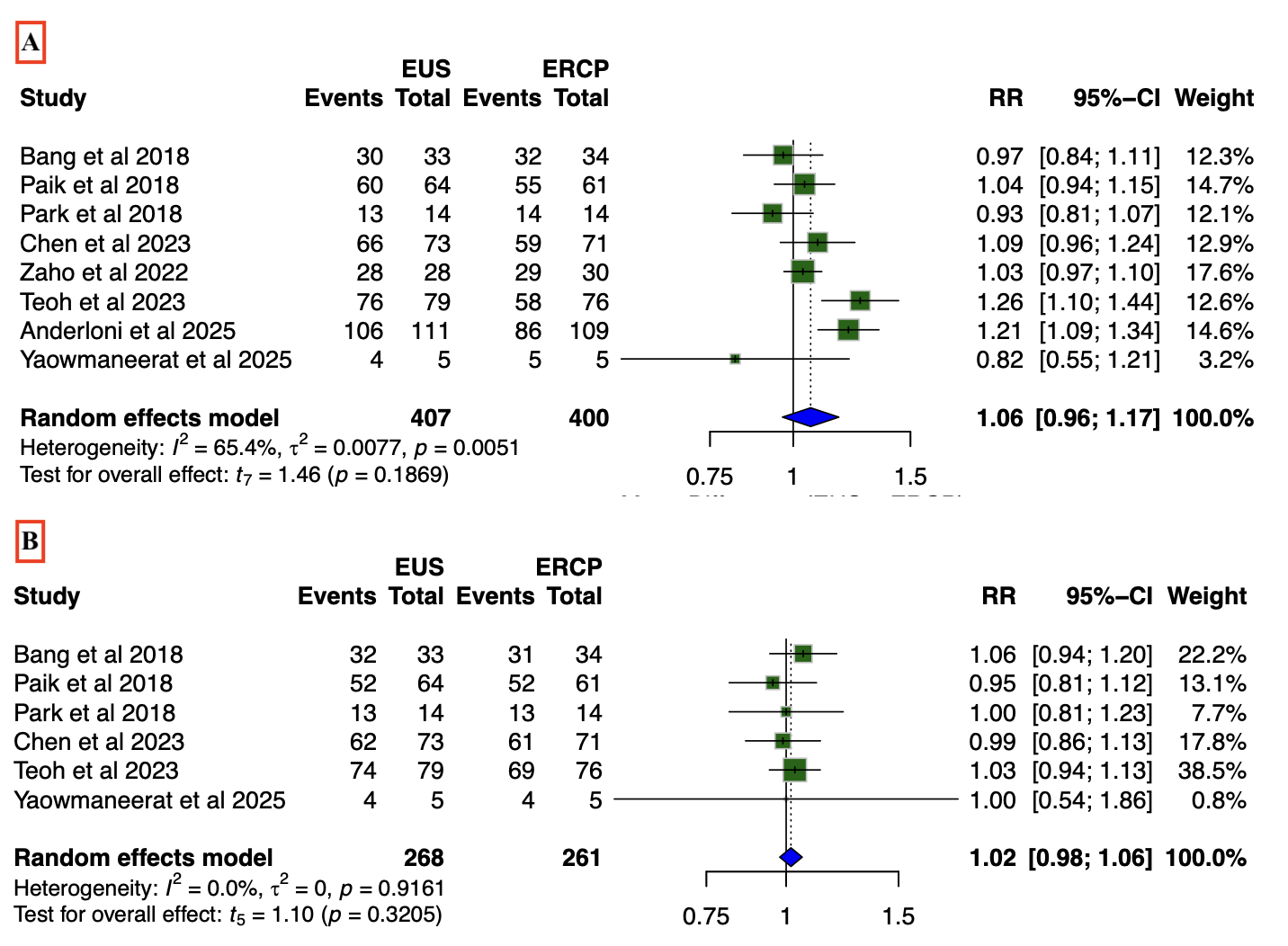
Figure: Table 1. Comparative Outcomes of EUS-BD versus ERCP-BD in Malignant Biliary Obstruction
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Osama Asad indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Yassine Kilani indicated no relevant financial relationships.
Mohamad Adam indicated no relevant financial relationships.
Dushyant Dahiya indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Saqr Alsakarneh, MD, MS1, Osama Asad, MD2, Razan Aburumman, MD3, Yassine Kilani, MD4, Mohamad Adam, MD2, Dushyant S. Dahiya, MD5, Mohammad Bilal, MD, FACG6. P5663 - Primary EUS-Guided Biliary Drainage Compared to ERCP for Malignant Biliary Obstruction: A Meta-Analysis of Randomized Controlled Trials, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
