Tuesday Poster Session
Category: Interventional Endoscopy
P5747 - A Case of a Large Walled-off Necrosis: The Answer Is Not Always LAMS
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Pranav Ramamurthy, MBBS, MD (he/him/his)
University of Massachusetts Chan Medical School-Baystate Medical Center
Springfield, MA
Presenting Author(s)
Pranav Ramamurthy, MBBS, MD1, Syed Hamza Sohail, MD2, Cristina Batarseh, MD3, Nha Duong, DO4
1University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Chicopee, MA; 4University of Massachusetts Chan Medical School-Baystate Medical Center, Granby, CT
Introduction: Complex peripancreatic collections including pseudocysts and walled-off pancreatic necrosis are often managed with endoscopic ultrasound (EUS) guided transmural drainage using lumen-apposing metal stents (LAMS). Pancreatic duct (PD) stents and transpapillary pseudocyst drainage can still have an important role based on the clinical scenario. We describe a case of a large abdominal peripancreatic collection managed via a PD stent with complete resolution.
Case Description/
Methods: A 47-year-old male with history of recurrent alcoholic pancreatitis presented with two weeks of progressive abdominal pain, fevers, and chills. Labs demonstrated leukocytosis and a lactate of 3 mmol/L. Blood cultures were positive for Citrobacter koseri and antibiotics were started. A computed tomography (CT) scan demonstrated multiple peripancreatic collections (MPC) with a large collection measuring up to 13 cm in the left hemi-abdomen (Figure 1a).
Due to the presence of MPC, we were most concerned for a PD leak as the underlying culprit. In addition, the largest collection was distant from the gastric wall therefore transmural drainage would require deep passage of the EUS scope to create a cystjejunostomy. We elected to proceed with endoscopic retrograde pancreatography (ERP) with plans to place a PD stent for the MPC.
ERP demonstrated a meandering PD (Figure 2a) which was straightened, and the wire was advanced deep into the tail of the pancreas. Pancreatogram revealed a PD neck stricture (Figure 2b) along with suspected leak sites in the pancreatic body and tail. Multiple devices (biliary dilation balloon, biliary extraction balloon, 7 Fr stent delivery system, needle knife sphincterotome, bougie biliary dilation catheter) were used but the stricture could not be traversed. Eventually we used a stent retrieval device to navigate beyond the stricture and then followed through with balloon dilation and subsequent stent insertion (Figure 2c). The patient recovered uneventfully and repeat CT scan 8 weeks later showed complete resolution of MPC including the large left sided collection (Figure 1b).
Discussion: This case highlights the utility of PD stenting for complex MPC particularly when PD leak is suspected in the presence of a downstream stricture. Bridging the stricture and leak sites with the stent can allow diversion of flow towards the major papilla and allow for resolution of MPC. Not all pancreatic collections need to be drained via LAMS and the decision should be taken on a case-by-case scenario.
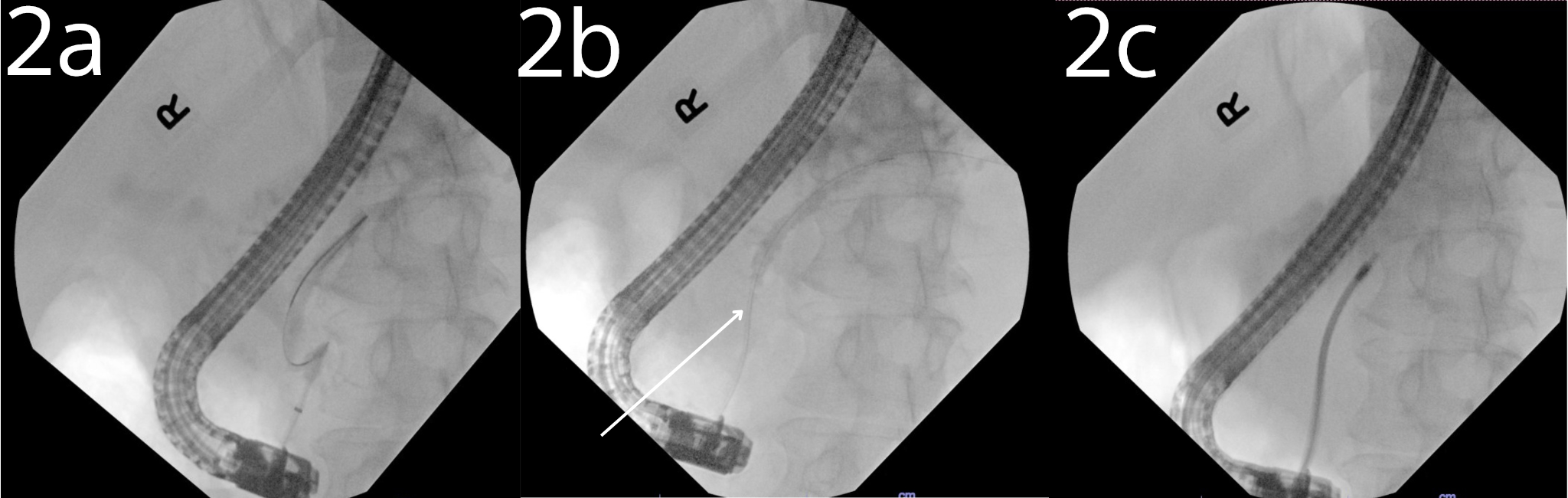
Figure: Figure 1a: Initial CT abdomen and pelvis demonstrating collections on presentation.
Figure 1b: Subsequent CT abdomen and pelvis demonstrating resolution of collections 8 weeks after PD stent placement.
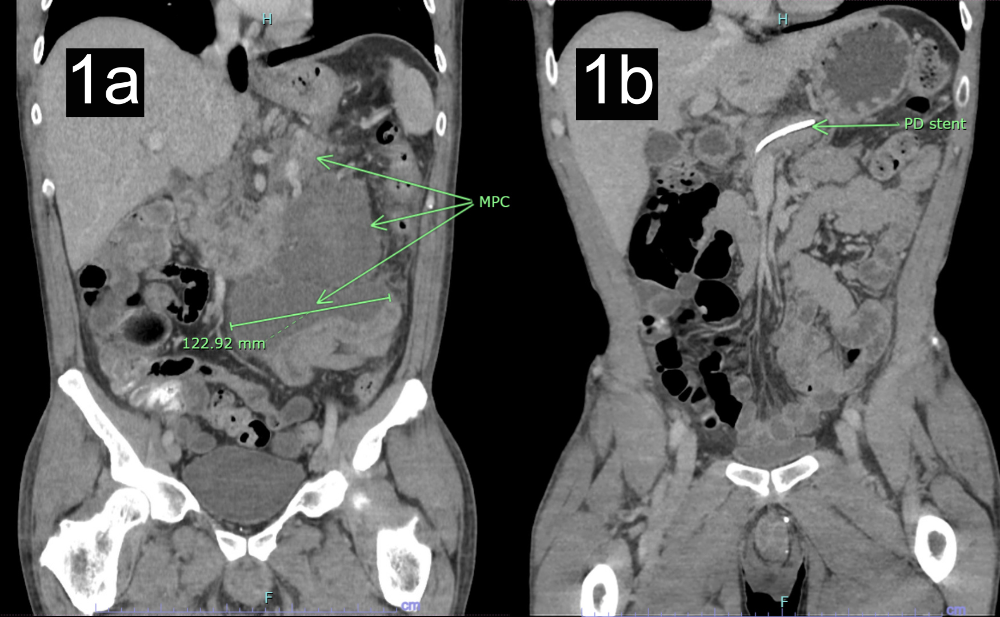
Figure: Figure 2a: Meandering pancreatic duct with sharp angulation with tip of wire knuckled in the pancreatic neck.
Figure 2b: PD wire straightened, and a stricture was seen in the neck of the pancreas (arrow).
Figure 2c: Stent retrieval device was used to negotiate the stricture successfully which allowed subsequently dilation and PD stent insertion.
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Cristina Batarseh indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Pranav Ramamurthy, MBBS, MD1, Syed Hamza Sohail, MD2, Cristina Batarseh, MD3, Nha Duong, DO4. P5747 - A Case of a Large Walled-off Necrosis: The Answer Is Not Always LAMS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Chicopee, MA; 4University of Massachusetts Chan Medical School-Baystate Medical Center, Granby, CT
Introduction: Complex peripancreatic collections including pseudocysts and walled-off pancreatic necrosis are often managed with endoscopic ultrasound (EUS) guided transmural drainage using lumen-apposing metal stents (LAMS). Pancreatic duct (PD) stents and transpapillary pseudocyst drainage can still have an important role based on the clinical scenario. We describe a case of a large abdominal peripancreatic collection managed via a PD stent with complete resolution.
Case Description/
Methods: A 47-year-old male with history of recurrent alcoholic pancreatitis presented with two weeks of progressive abdominal pain, fevers, and chills. Labs demonstrated leukocytosis and a lactate of 3 mmol/L. Blood cultures were positive for Citrobacter koseri and antibiotics were started. A computed tomography (CT) scan demonstrated multiple peripancreatic collections (MPC) with a large collection measuring up to 13 cm in the left hemi-abdomen (Figure 1a).
Due to the presence of MPC, we were most concerned for a PD leak as the underlying culprit. In addition, the largest collection was distant from the gastric wall therefore transmural drainage would require deep passage of the EUS scope to create a cystjejunostomy. We elected to proceed with endoscopic retrograde pancreatography (ERP) with plans to place a PD stent for the MPC.
ERP demonstrated a meandering PD (Figure 2a) which was straightened, and the wire was advanced deep into the tail of the pancreas. Pancreatogram revealed a PD neck stricture (Figure 2b) along with suspected leak sites in the pancreatic body and tail. Multiple devices (biliary dilation balloon, biliary extraction balloon, 7 Fr stent delivery system, needle knife sphincterotome, bougie biliary dilation catheter) were used but the stricture could not be traversed. Eventually we used a stent retrieval device to navigate beyond the stricture and then followed through with balloon dilation and subsequent stent insertion (Figure 2c). The patient recovered uneventfully and repeat CT scan 8 weeks later showed complete resolution of MPC including the large left sided collection (Figure 1b).
Discussion: This case highlights the utility of PD stenting for complex MPC particularly when PD leak is suspected in the presence of a downstream stricture. Bridging the stricture and leak sites with the stent can allow diversion of flow towards the major papilla and allow for resolution of MPC. Not all pancreatic collections need to be drained via LAMS and the decision should be taken on a case-by-case scenario.
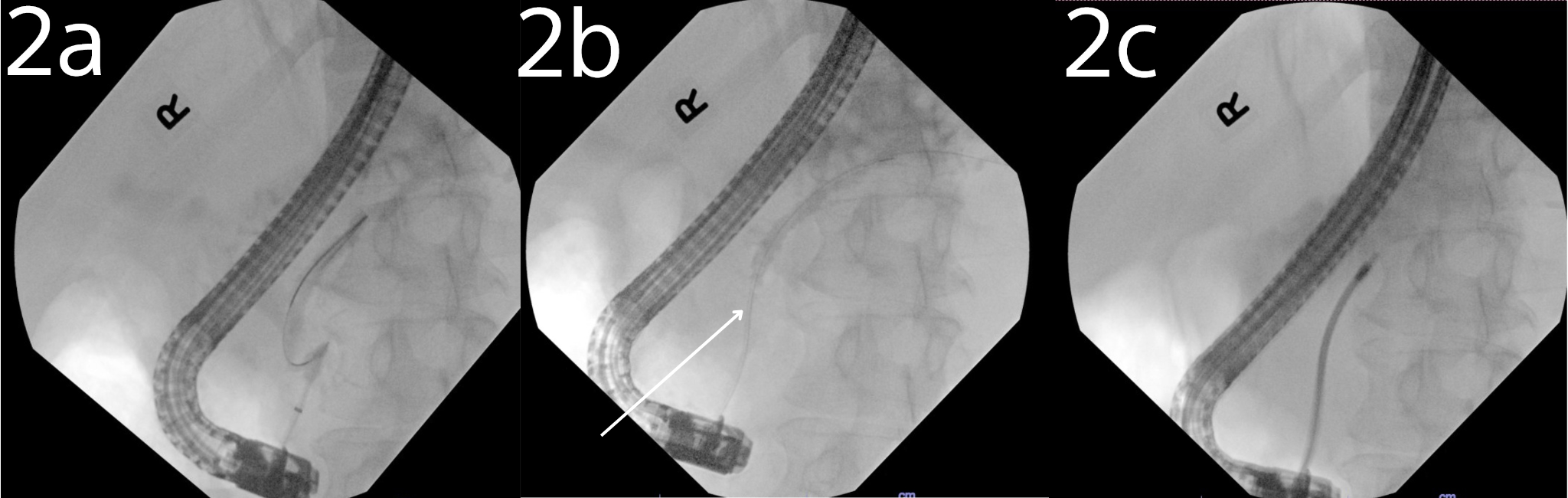
Figure: Figure 1a: Initial CT abdomen and pelvis demonstrating collections on presentation.
Figure 1b: Subsequent CT abdomen and pelvis demonstrating resolution of collections 8 weeks after PD stent placement.
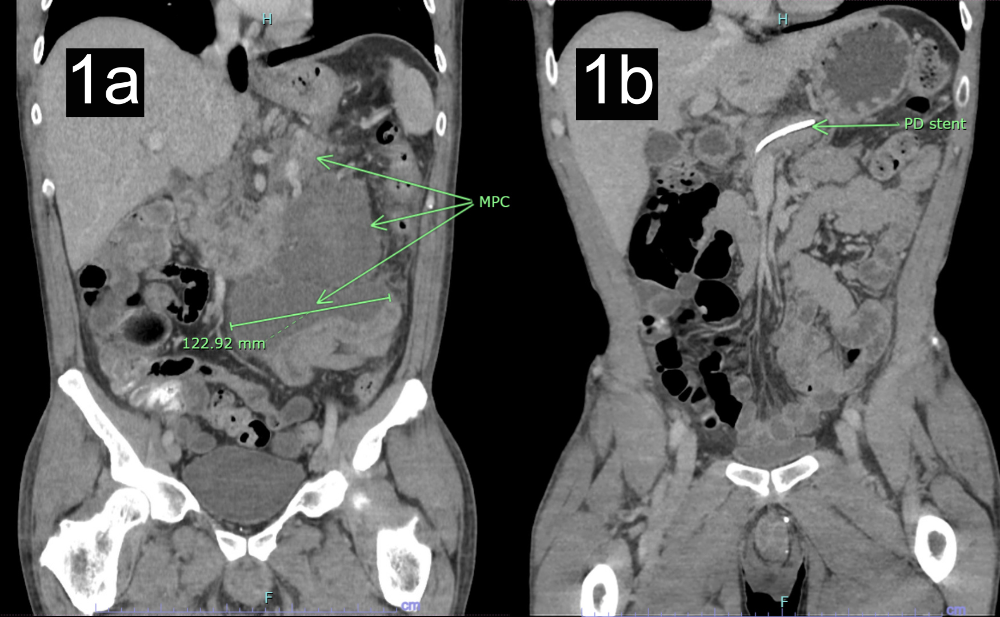
Figure: Figure 2a: Meandering pancreatic duct with sharp angulation with tip of wire knuckled in the pancreatic neck.
Figure 2b: PD wire straightened, and a stricture was seen in the neck of the pancreas (arrow).
Figure 2c: Stent retrieval device was used to negotiate the stricture successfully which allowed subsequently dilation and PD stent insertion.
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Cristina Batarseh indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Pranav Ramamurthy, MBBS, MD1, Syed Hamza Sohail, MD2, Cristina Batarseh, MD3, Nha Duong, DO4. P5747 - A Case of a Large Walled-off Necrosis: The Answer Is Not Always LAMS, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
