Tuesday Poster Session
Category: Interventional Endoscopy
P5746 - Unique Problems and Unique Solutions: A Case Necessitating Endoscopic Ultrasound-guided Antegrade Cholangiopancreatography (EACP)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Pranav Ramamurthy, MBBS, MD (he/him/his)
University of Massachusetts Chan Medical School-Baystate Medical Center
Springfield, MA
Presenting Author(s)
Pranav Ramamurthy, MBBS, MD1, Aizaz Khan, MD2, Safia Mohamed, MD2, Nha Duong, DO3
1University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Granby, CT
Introduction: Endoscopic ultrasound-guided (EUS) biliary drainage has emerged as a valuable alternative in cases where conventional endoscopic retrograde cholangiopancreaticography (ERCP) is unsuccessful. If the papilla is inaccessible, we revert to EUS guided drainage with either choledochoduodenostomy (EUS-BD) or hepaticogastrostomy (HGS). We present a unique case of malignant distal biliary obstruction (MDBO) and duodenal obstruction eventually necessitating EACP.
Case Description/
Methods: A 64-year-old male with metastatic prostate cancer underwent abdominal MRI for restaging, which revealed an incidental 3.6 cm pancreatic head mass causing MDBO. The proximal common bile duct (CBD) was 10 mm with a distal stricture in the area of the mass. The patient was symptomatic, with a bilirubin of 4.6 mg/dL. ERCP was attempted, however, tumor infiltration led to severe duodenal stricturing, preventing passage of the ERCP scope or gastroscope. Therapeutic options were discussed with the patient, which included HGS, percutaneous transhepatic biliary drainage (PTBD), or EACP. We did not offer EUS-BD due to the small caliber of the CBD and tumor infiltration within the duodenal bulb. The patient elected for EACP due to a preference to preserve the natural drainage pathway.
A 19-gauge EUS-FNA needle was used to puncture a branch of the left intrahepatic duct, and a cholangiogram confirmed positioning. A 0.025” guidewire was advanced into the CBD but even after numerous attempts, we could not traverse the stricture (Figure 1a). We then used a needle knife sphincterotome (NKS) to negotiate through the gastric wall, liver capsule, and biliary epithelium. With the NKS in the proximal CBD, we exchanged the 0.025” wire for a 0.035” wire and were able to negotiate this across the stricture into the small bowel (Figure 1b). We then performed segmental dilatation of the liver parenchyma using a 4 mm balloon to allow for passage of the stent catheter while minimizing the risk of bile leakage. A 10 mm x 80 mm uncovered metal stent was deployed across the stricture with contrast drainage confirmed (Figure 1c). The patient recovered uneventfully and was discharged two days later with a normalized bilirubin.
Discussion: EACP is not a commonly used technique for drainage of MDBO due to its technical challenges and higher risk of bile leakage. This technique was used for our patient to preserve the natural drainage pathway while avoiding PTBD. EACP should remain available in the arsenal of every advanced endoscopist who manages MDBO.
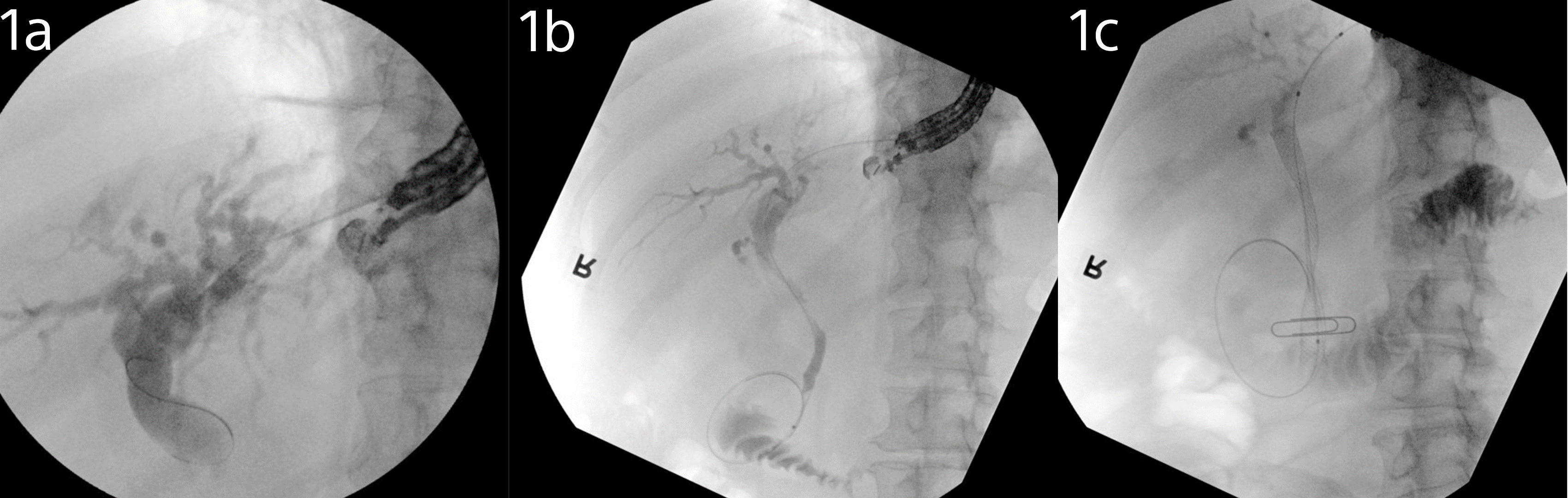
Figure: Figure 1a - 0.025” guidewire unable to traverse the common bile duct (CBD) stricture
Figure 1b - Needle-knife sphincterotome in the proximal CBD, 0.025” wire exchanged for a 0.035” wire and negotiated across the CBD stricture into the small bowel
Figure 1c - 10 mm x 80 mm uncovered metal stent deployed across the CBD stricture with contrast drainage confirmed
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Safia Mohamed indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Pranav Ramamurthy, MBBS, MD1, Aizaz Khan, MD2, Safia Mohamed, MD2, Nha Duong, DO3. P5746 - Unique Problems and Unique Solutions: A Case Necessitating Endoscopic Ultrasound-guided Antegrade Cholangiopancreatography (EACP), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School-Baystate Medical Center, Granby, CT
Introduction: Endoscopic ultrasound-guided (EUS) biliary drainage has emerged as a valuable alternative in cases where conventional endoscopic retrograde cholangiopancreaticography (ERCP) is unsuccessful. If the papilla is inaccessible, we revert to EUS guided drainage with either choledochoduodenostomy (EUS-BD) or hepaticogastrostomy (HGS). We present a unique case of malignant distal biliary obstruction (MDBO) and duodenal obstruction eventually necessitating EACP.
Case Description/
Methods: A 64-year-old male with metastatic prostate cancer underwent abdominal MRI for restaging, which revealed an incidental 3.6 cm pancreatic head mass causing MDBO. The proximal common bile duct (CBD) was 10 mm with a distal stricture in the area of the mass. The patient was symptomatic, with a bilirubin of 4.6 mg/dL. ERCP was attempted, however, tumor infiltration led to severe duodenal stricturing, preventing passage of the ERCP scope or gastroscope. Therapeutic options were discussed with the patient, which included HGS, percutaneous transhepatic biliary drainage (PTBD), or EACP. We did not offer EUS-BD due to the small caliber of the CBD and tumor infiltration within the duodenal bulb. The patient elected for EACP due to a preference to preserve the natural drainage pathway.
A 19-gauge EUS-FNA needle was used to puncture a branch of the left intrahepatic duct, and a cholangiogram confirmed positioning. A 0.025” guidewire was advanced into the CBD but even after numerous attempts, we could not traverse the stricture (Figure 1a). We then used a needle knife sphincterotome (NKS) to negotiate through the gastric wall, liver capsule, and biliary epithelium. With the NKS in the proximal CBD, we exchanged the 0.025” wire for a 0.035” wire and were able to negotiate this across the stricture into the small bowel (Figure 1b). We then performed segmental dilatation of the liver parenchyma using a 4 mm balloon to allow for passage of the stent catheter while minimizing the risk of bile leakage. A 10 mm x 80 mm uncovered metal stent was deployed across the stricture with contrast drainage confirmed (Figure 1c). The patient recovered uneventfully and was discharged two days later with a normalized bilirubin.
Discussion: EACP is not a commonly used technique for drainage of MDBO due to its technical challenges and higher risk of bile leakage. This technique was used for our patient to preserve the natural drainage pathway while avoiding PTBD. EACP should remain available in the arsenal of every advanced endoscopist who manages MDBO.
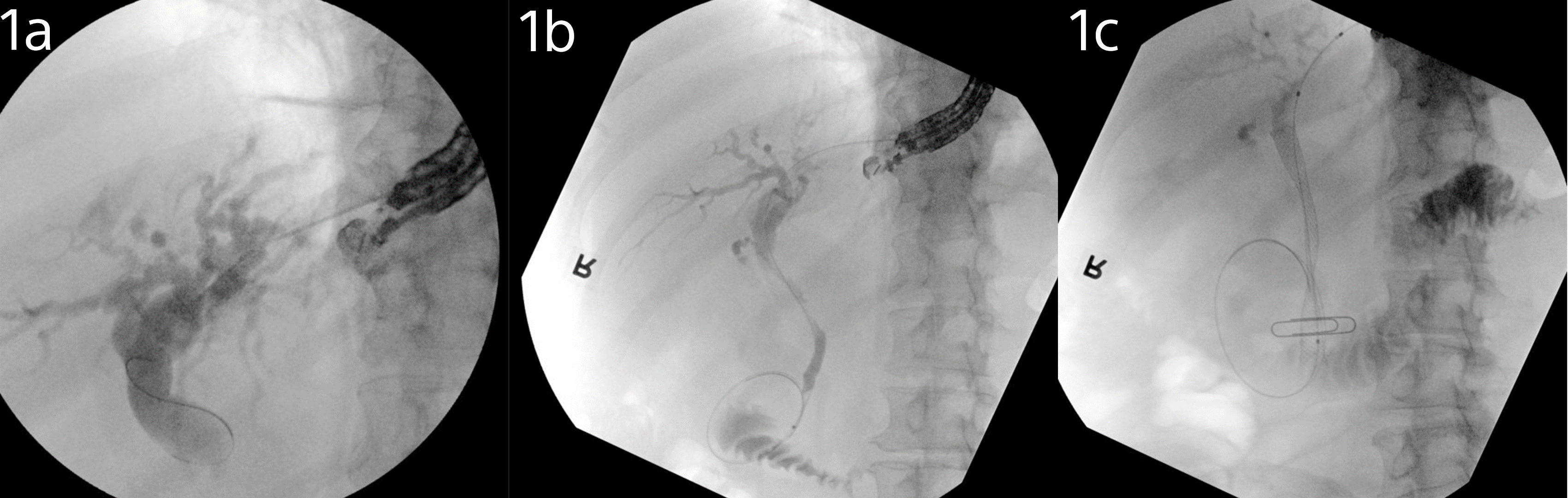
Figure: Figure 1a - 0.025” guidewire unable to traverse the common bile duct (CBD) stricture
Figure 1b - Needle-knife sphincterotome in the proximal CBD, 0.025” wire exchanged for a 0.035” wire and negotiated across the CBD stricture into the small bowel
Figure 1c - 10 mm x 80 mm uncovered metal stent deployed across the CBD stricture with contrast drainage confirmed
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Safia Mohamed indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Pranav Ramamurthy, MBBS, MD1, Aizaz Khan, MD2, Safia Mohamed, MD2, Nha Duong, DO3. P5746 - Unique Problems and Unique Solutions: A Case Necessitating Endoscopic Ultrasound-guided Antegrade Cholangiopancreatography (EACP), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
