Tuesday Poster Session
Category: Interventional Endoscopy
P5744 - Complex Endoscopic Management of Bronchobiliary Fistula Secondary to Multifocal Hepatic Abscesses
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Pranav Ramamurthy, MBBS, MD (he/him/his)
University of Massachusetts Chan Medical School-Baystate Medical Center
Springfield, MA
Presenting Author(s)
Pranav Ramamurthy, MBBS, MD1, Syed Hamza Sohail, MD2, Rony Ghaoui, MD3, Aizaz Khan, MD2
1University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School - Baystate Health, Westfield, MA
Introduction: Bronchobiliary fistula (BBF) is a rare abnormal connection between the biliary system and the bronchial tree, often resulting from trauma, tumors, or surgery. Infection is a rarer cause of BBF. We describe a rare case of BBF in a patient with multiple hepatic abscesses managed with simultaneous bronchoscopy and endoscopic retrograde cholangiopancreatography (ERCP).
Case Description/
Methods: A 44-year-old woman with a past medical history of intravenous drug use, hepatitis C, bronchiectasis and prior right colectomy was admitted with a bronchiectasis exacerbation. Her hospital course was complicated by secondary bacterial peritonitis due to a stercoral sigmoid colonic perforation. Abdominal imaging showed multifocal hepatic abscesses with pneumobilia with concern for a BBF between the bronchiectasis of the right middle lobe and the bile ducts in hepatic segment VIII (Figure 1). An exploratory laparotomy with left-sided colectomy and diverting ostomy was performed, and a percutaneous drain was placed in the largest hepatic abscess in the hepatic segment VI. Patient’s blood and peritoneal cultures were positive and treated with IV antibiotics.
The patient had ongoing bilious drainage from tracheal suctioning and a HIDA scan confirmed the presence of a persistent BBF (Figure 2). Bronchoscopy showed bile staining throughout the bilateral bronchial trees and was able to visualize active bilious reflux from the lateral segment bronchus of the right middle lobe. A 5.5 mm endobronchial valve (EBV) was placed by thoracic surgery. Same session ERCP demonstrated mild common bile duct dilatation to 12 mm with no filling defect and no intrahepatic biliary dilatation. Biliary sphincterotomy was performed and a 10 Fr x 90 mm plastic biliary stent was placed. Follow up imaging showed decrease in size of hepatic abscesses, and the patient improved symptomatically. She was discharged on IV antibiotics with plan for repeat ERCP for stent removal.
Discussion: BBFs are usually managed operatively. Prior case reports of endoscopic management report the use of ERCP-based tract embolization, but EBVs have not been reported prior. EBVs allow retrograde passage of air and purulent secretions while blocking anterograde airflow allowing the fistula to heal. Simultaneous ERCP with biliary stenting creates a favorable gradient for the BBF to heal. There are no prior reports of EBV with ERCP for BBF secondary to infection and this case represents a successful interdisciplinary approach to managing these more conservatively.
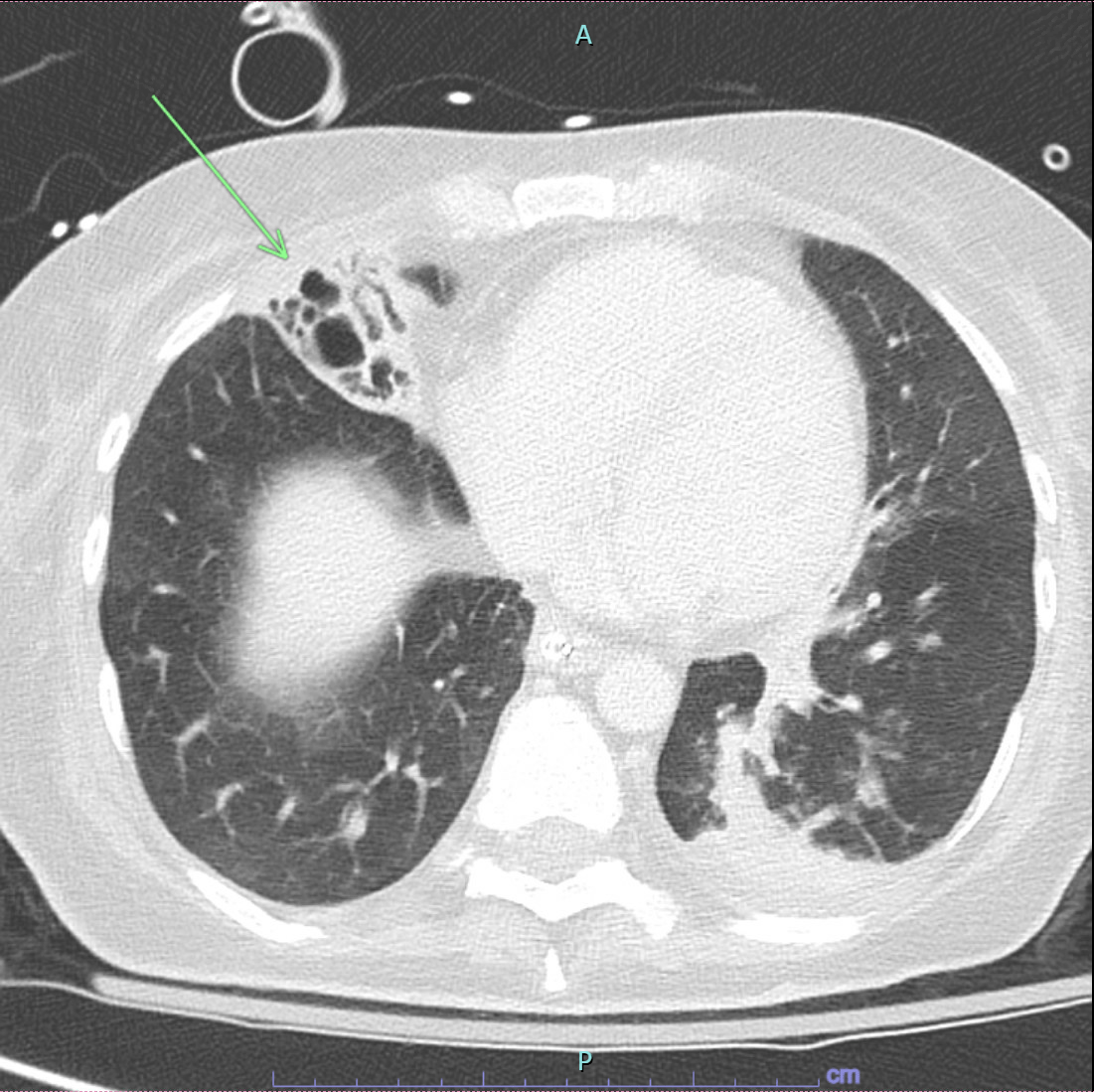
Figure: Figure 1: CT imaging demonstrating bronchobiliary fistula between the bronchiectasis of the right middle lobe and the bile ducts in hepatic segment VIII
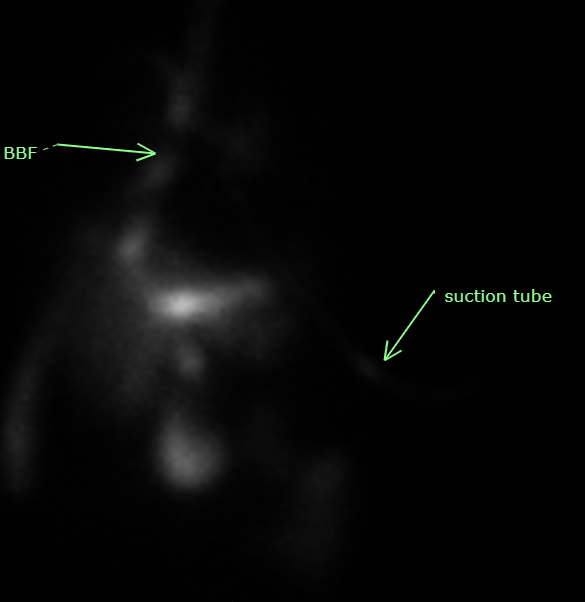
Figure: Figure 2: HIDA scan demonstrating a tubular tract of radiotracer activity extending from the dome of right lobe superiorly towards the trachea, consistent with bronchobiliary fistula.
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Rony Ghaoui indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Pranav Ramamurthy, MBBS, MD1, Syed Hamza Sohail, MD2, Rony Ghaoui, MD3, Aizaz Khan, MD2. P5744 - Complex Endoscopic Management of Bronchobiliary Fistula Secondary to Multifocal Hepatic Abscesses, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Massachusetts Chan Medical School-Baystate Medical Center, Springfield, MA; 2University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA; 3University of Massachusetts Chan Medical School - Baystate Health, Westfield, MA
Introduction: Bronchobiliary fistula (BBF) is a rare abnormal connection between the biliary system and the bronchial tree, often resulting from trauma, tumors, or surgery. Infection is a rarer cause of BBF. We describe a rare case of BBF in a patient with multiple hepatic abscesses managed with simultaneous bronchoscopy and endoscopic retrograde cholangiopancreatography (ERCP).
Case Description/
Methods: A 44-year-old woman with a past medical history of intravenous drug use, hepatitis C, bronchiectasis and prior right colectomy was admitted with a bronchiectasis exacerbation. Her hospital course was complicated by secondary bacterial peritonitis due to a stercoral sigmoid colonic perforation. Abdominal imaging showed multifocal hepatic abscesses with pneumobilia with concern for a BBF between the bronchiectasis of the right middle lobe and the bile ducts in hepatic segment VIII (Figure 1). An exploratory laparotomy with left-sided colectomy and diverting ostomy was performed, and a percutaneous drain was placed in the largest hepatic abscess in the hepatic segment VI. Patient’s blood and peritoneal cultures were positive and treated with IV antibiotics.
The patient had ongoing bilious drainage from tracheal suctioning and a HIDA scan confirmed the presence of a persistent BBF (Figure 2). Bronchoscopy showed bile staining throughout the bilateral bronchial trees and was able to visualize active bilious reflux from the lateral segment bronchus of the right middle lobe. A 5.5 mm endobronchial valve (EBV) was placed by thoracic surgery. Same session ERCP demonstrated mild common bile duct dilatation to 12 mm with no filling defect and no intrahepatic biliary dilatation. Biliary sphincterotomy was performed and a 10 Fr x 90 mm plastic biliary stent was placed. Follow up imaging showed decrease in size of hepatic abscesses, and the patient improved symptomatically. She was discharged on IV antibiotics with plan for repeat ERCP for stent removal.
Discussion: BBFs are usually managed operatively. Prior case reports of endoscopic management report the use of ERCP-based tract embolization, but EBVs have not been reported prior. EBVs allow retrograde passage of air and purulent secretions while blocking anterograde airflow allowing the fistula to heal. Simultaneous ERCP with biliary stenting creates a favorable gradient for the BBF to heal. There are no prior reports of EBV with ERCP for BBF secondary to infection and this case represents a successful interdisciplinary approach to managing these more conservatively.
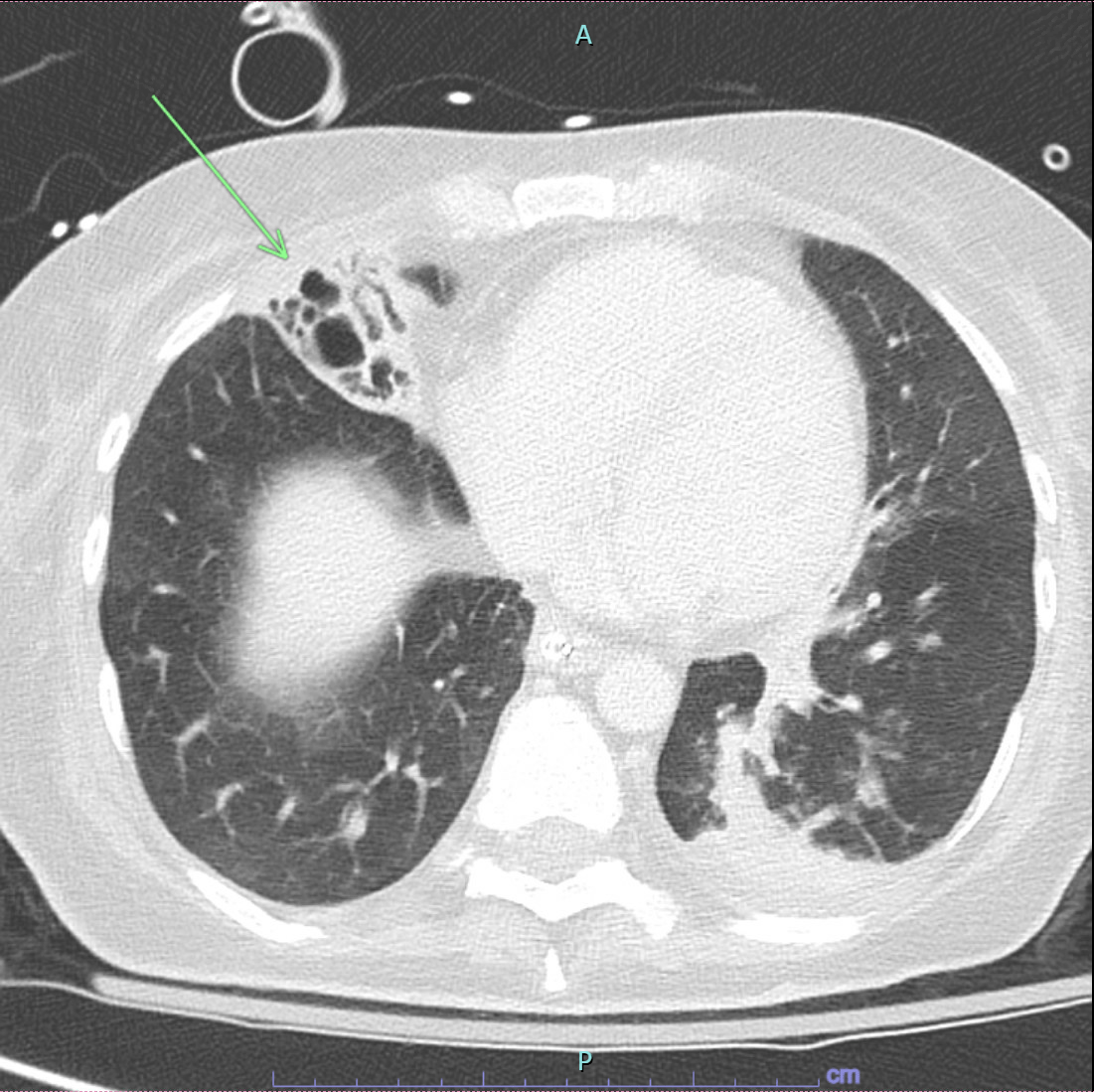
Figure: Figure 1: CT imaging demonstrating bronchobiliary fistula between the bronchiectasis of the right middle lobe and the bile ducts in hepatic segment VIII
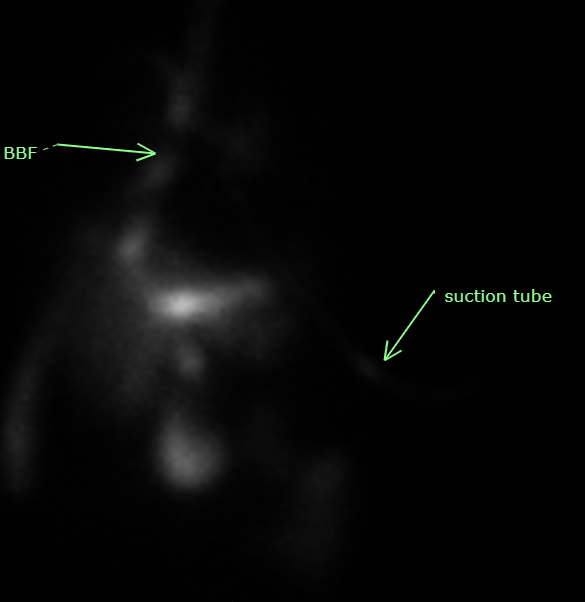
Figure: Figure 2: HIDA scan demonstrating a tubular tract of radiotracer activity extending from the dome of right lobe superiorly towards the trachea, consistent with bronchobiliary fistula.
Disclosures:
Pranav Ramamurthy indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Rony Ghaoui indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Pranav Ramamurthy, MBBS, MD1, Syed Hamza Sohail, MD2, Rony Ghaoui, MD3, Aizaz Khan, MD2. P5744 - Complex Endoscopic Management of Bronchobiliary Fistula Secondary to Multifocal Hepatic Abscesses, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
