Tuesday Poster Session
Category: Interventional Endoscopy
P5741 - Diagnostic and Therapeutic Challenges in Gastric Adenocarcinoma: A Case of Missed Detection on Biopsy and PET Imaging Requiring Multimodal Endoscopic Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sindhuja Naidoo, MBBCh
Royal College of Surgeons in Ireland
Vancouver, BC, Canada
Presenting Author(s)
Ishan Antony, MD1, Sindhuja Naidoo, MBBCh2, Akshay Kapoor, MD3, Kristen Farwell, MD3
1Beth Israel Lahey Health, Burlington, MA; 2Royal College of Surgeons in Ireland, Dublin, Dublin, Ireland; 3Lahey Hospital and Medical Center, Burlington, MA
Introduction: Gastric adenocarcinoma (GA) diagnosis remains challenging due to nonspecific symptoms and limitations in timely workup. Endoscopic biopsy may be nondiagnostic, and PET scans have variable sensitivity, particularly in signet ring histology. This case required multimodal endoscopic techniques for definitive diagnosis after initial biopsy, and PET failed to confirm GA.
Case Description/
Methods: A 64-year-old woman with recent pancreatitis, pulmonary embolism, and septic thrombophlebitis of the left internal jugular vein presented with progressive early satiety, dark urine, and weight loss. Labs showed cholestatic liver enzyme elevation. CT abdomen revealed biliary dilation, gastric antral thickening, and lymphadenopathy (Fig. 1A). MRCP confirmed bile duct thickening and lymphadenopathy.
EGD one month prior showed a fungating antral mass (Fig. 1B), but pathology from biopsies revealed only chronic inflammatory changes. PET scan demonstrated hypermetabolic lymphadenopathy without gastric uptake, raising concern for lymphoma. Due to worsening satiety and concern for gastric outlet obstruction, repeat EGD with EUS was performed, confirming a stenotic antral mass (Fig. 1C). Given significant narrowing, an uncovered metal stent was placed for symptom relief. EUS-guided fine-needle biopsies (FNB) of the mass and periceliac lymph nodes confirmed poorly differentiated adenocarcinoma with signet ring features and metastatic lymphadenopathy, establishing stage IV GA. The patient later developed obstructive jaundice, requiring biliary decompression via internal/external drains. ERCP was not attempted due to antral stenosis and lack of ampullary access. Given her decline and nutritional compromise, she was not an ideal chemotherapy candidate and ultimately decided to transition her to hospice.
Discussion: This case highlights the benefit of EUS-FNB in GA diagnosis after an inconclusive biopsy and high suspicion for malignancy. Endoscopic stenting provided symptom relief for gastric outlet obstruction, while biliary decompression required alternative approaches given anatomic challenges. Up to 10% of gastric cancers are missed at EGD. PET scan sensitivity varies, particularly in signet ring GA, where lower metabolic activity leads to false-negative results. This case underscores the need for repeat tissue sampling when there is a strong suspicion, multimodal endoscopic approaches, and strategic therapeutic decisions in complex GA cases.
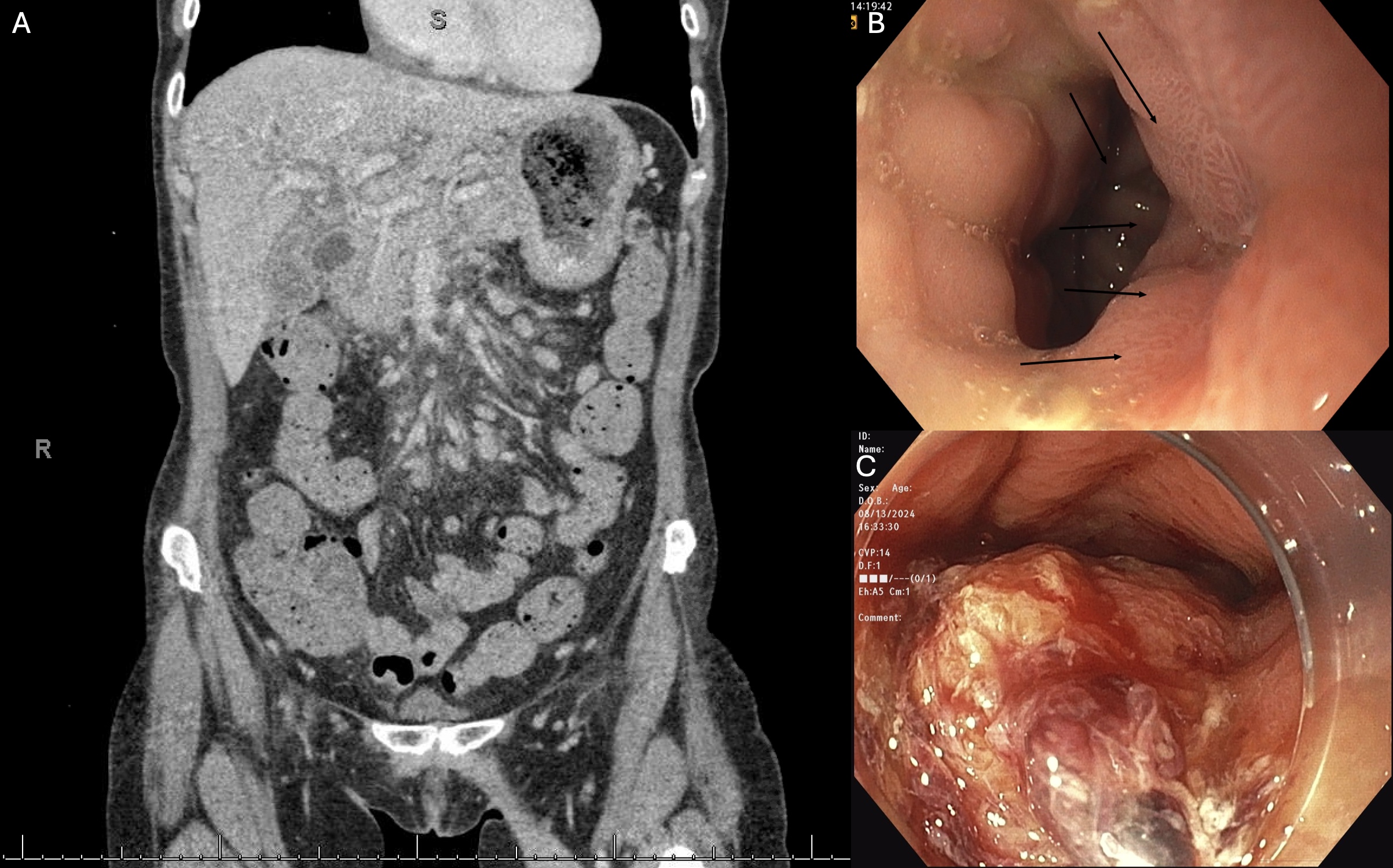
Figure: Figure 1: (A) Axial contrast-enhanced CT abdomen/pelvis demonstrating gastric wall thickening and intrahepatic biliary dilation. (B) Initial EGD showing a fungating, multilobular, ulcerated antral mass with an irregular surface. (C) Repeat EGD showing significant antral stenosis with tumor progression.

Figure: Table 1: Timeline of Diagnostic Findings, Interventions, and Disease Progression
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Sindhuja Naidoo indicated no relevant financial relationships.
Akshay Kapoor indicated no relevant financial relationships.
Kristen Farwell indicated no relevant financial relationships.
Ishan Antony, MD1, Sindhuja Naidoo, MBBCh2, Akshay Kapoor, MD3, Kristen Farwell, MD3. P5741 - Diagnostic and Therapeutic Challenges in Gastric Adenocarcinoma: A Case of Missed Detection on Biopsy and PET Imaging Requiring Multimodal Endoscopic Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Lahey Health, Burlington, MA; 2Royal College of Surgeons in Ireland, Dublin, Dublin, Ireland; 3Lahey Hospital and Medical Center, Burlington, MA
Introduction: Gastric adenocarcinoma (GA) diagnosis remains challenging due to nonspecific symptoms and limitations in timely workup. Endoscopic biopsy may be nondiagnostic, and PET scans have variable sensitivity, particularly in signet ring histology. This case required multimodal endoscopic techniques for definitive diagnosis after initial biopsy, and PET failed to confirm GA.
Case Description/
Methods: A 64-year-old woman with recent pancreatitis, pulmonary embolism, and septic thrombophlebitis of the left internal jugular vein presented with progressive early satiety, dark urine, and weight loss. Labs showed cholestatic liver enzyme elevation. CT abdomen revealed biliary dilation, gastric antral thickening, and lymphadenopathy (Fig. 1A). MRCP confirmed bile duct thickening and lymphadenopathy.
EGD one month prior showed a fungating antral mass (Fig. 1B), but pathology from biopsies revealed only chronic inflammatory changes. PET scan demonstrated hypermetabolic lymphadenopathy without gastric uptake, raising concern for lymphoma. Due to worsening satiety and concern for gastric outlet obstruction, repeat EGD with EUS was performed, confirming a stenotic antral mass (Fig. 1C). Given significant narrowing, an uncovered metal stent was placed for symptom relief. EUS-guided fine-needle biopsies (FNB) of the mass and periceliac lymph nodes confirmed poorly differentiated adenocarcinoma with signet ring features and metastatic lymphadenopathy, establishing stage IV GA. The patient later developed obstructive jaundice, requiring biliary decompression via internal/external drains. ERCP was not attempted due to antral stenosis and lack of ampullary access. Given her decline and nutritional compromise, she was not an ideal chemotherapy candidate and ultimately decided to transition her to hospice.
Discussion: This case highlights the benefit of EUS-FNB in GA diagnosis after an inconclusive biopsy and high suspicion for malignancy. Endoscopic stenting provided symptom relief for gastric outlet obstruction, while biliary decompression required alternative approaches given anatomic challenges. Up to 10% of gastric cancers are missed at EGD. PET scan sensitivity varies, particularly in signet ring GA, where lower metabolic activity leads to false-negative results. This case underscores the need for repeat tissue sampling when there is a strong suspicion, multimodal endoscopic approaches, and strategic therapeutic decisions in complex GA cases.
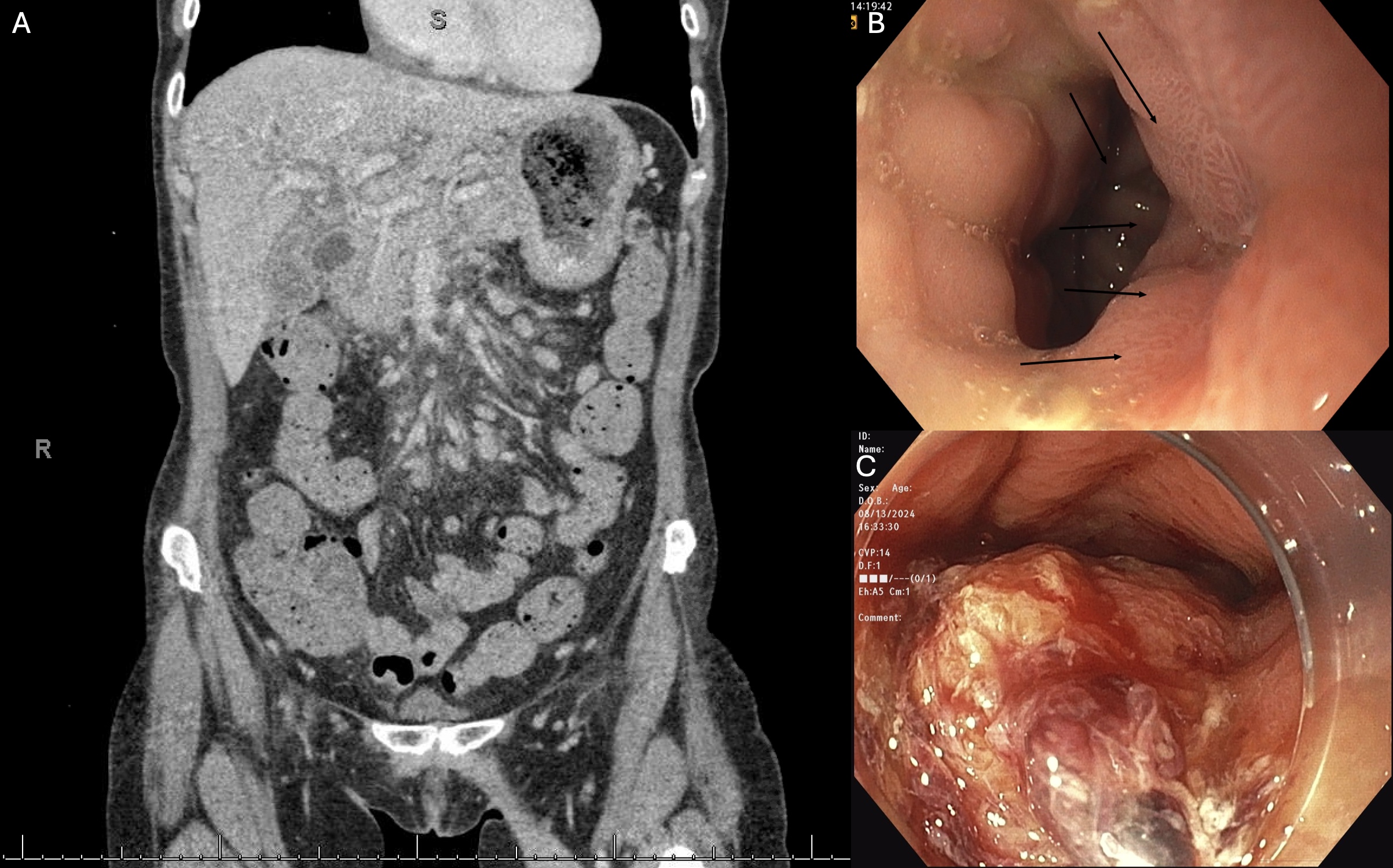
Figure: Figure 1: (A) Axial contrast-enhanced CT abdomen/pelvis demonstrating gastric wall thickening and intrahepatic biliary dilation. (B) Initial EGD showing a fungating, multilobular, ulcerated antral mass with an irregular surface. (C) Repeat EGD showing significant antral stenosis with tumor progression.

Figure: Table 1: Timeline of Diagnostic Findings, Interventions, and Disease Progression
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Sindhuja Naidoo indicated no relevant financial relationships.
Akshay Kapoor indicated no relevant financial relationships.
Kristen Farwell indicated no relevant financial relationships.
Ishan Antony, MD1, Sindhuja Naidoo, MBBCh2, Akshay Kapoor, MD3, Kristen Farwell, MD3. P5741 - Diagnostic and Therapeutic Challenges in Gastric Adenocarcinoma: A Case of Missed Detection on Biopsy and PET Imaging Requiring Multimodal Endoscopic Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

