Tuesday Poster Session
Category: Interventional Endoscopy
P5740 - Endoscopic Ultrasound With Coiling for Treatment of Hemosuccus Pancreaticus
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ishan Antony, MD
Beth Israel Lahey Health
Burlington, MA
Presenting Author(s)
Award: ACG Presidential Poster Award
Ishan Antony, MD1, Ibrahim Reyaz, MBBS2, Christopher Ward, MD3, Narinderjeet Kaur, MD, MS4, Khaldoon Khirfan, MD3
1Beth Israel Lahey Health, Burlington, MA; 2Nassau University Medical Center, East Meadow, NY; 3Lahey Hospital and Medical Center, Burlington, MA; 4SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal bleeding (GIB) typically caused by pseudoaneurysms of branches of the splenic artery. Embolization by interventional radiology is the main treatment modality, and sometimes surgery is required for refractory cases.
Case Description/
Methods: A 48-year-old woman with chronic pancreatitis due to alcohol, recent exacerbation with acute pancreatitis a few weeks before admission, splenic vein thrombosis, and a symptomatic 9 cm pseudocyst. The patient underwent endoscopic ultrasound (EUS)-guided cystgastrostomy with a lumen-apposing metal stent (LAMS). During admission, the patient started developing melena and shock. EGD was performed, which showed no evidence of bleeding at the cystgastrostomy. There was evidence of active bleeding from the site of the papilla consistent with HP. Computed tomography (CT) scan showed a 2 cm splenic artery aneurysm with active bleeding. Angiography with balloon-assisted splenic artery embolization was performed, but was not successful in achieving hemostasis. At that point, the patient was referred to our facility for further management.
The case was discussed with the multidisciplinary team. The consensus was to attempt EUS-guided treatment of the pseudoaneurysm. EUS showed a splenic artery pseudoaneurysm with artifact from the previously placed coils. Coiling of the pseudoaneurysm was performed using the 19 GA fine needle biopsy (FNA) needle using 14 cm-long cylindrical coils, followed by gel foam injection. There was immediate cessation of the bleeding at the site of the papilla. The patient tolerated the procedure without complication and remained transfusion-free for 48 hours before rebleeding.
Given persistent hemorrhage, surgical option was considered. In preparation for surgery, endoscopic retrograde pancreatography (ERP) was performed to evaluate the integrity of the pancreatic duct. ERP revealed contrast extravasation from the pancreatic duct in the tail into the pseudoaneurysm. The patient underwent distal pancreatectomy, splenectomy, and surgical debridement of the necrotic walled-off necrosis. The patient had an uneventful postoperative course.
Discussion: This case highlights the importance of considering HP in patients with chronic pancreatitis with GIB. Arteriography with embolization and vascular stenting is the main modality of treatment. Traditionally, surgery has been considered for refractory cases. EUS may have a promising role in the management of HP.
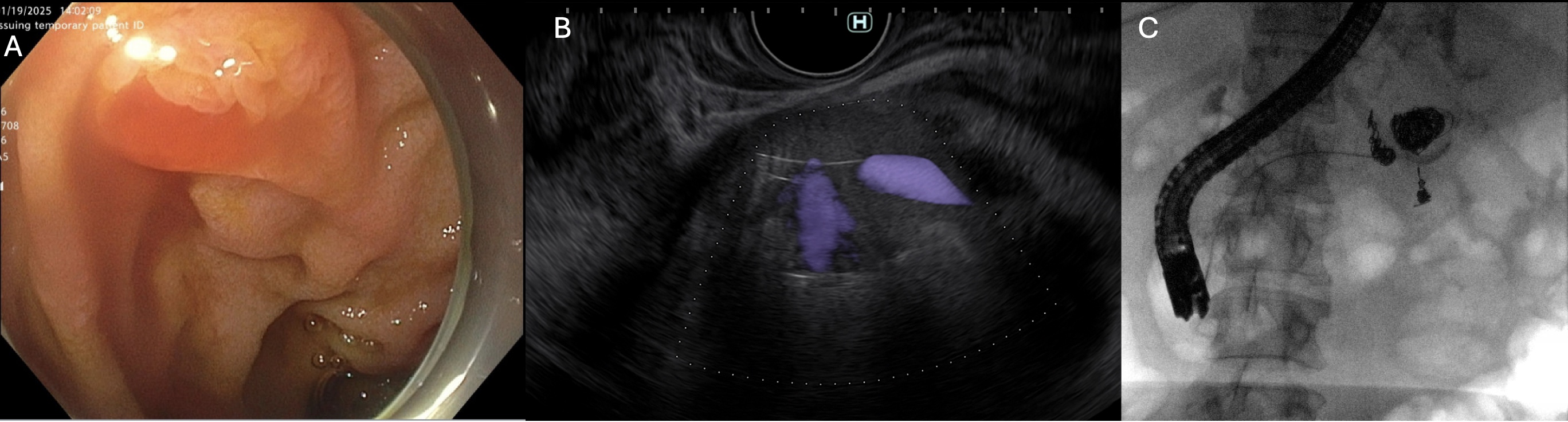
Figure: Figure 1: A) EGD image capturing active bleeding from the ampulla, B) EUS showed pseudoaneurysm with coils and active blood flow. C) ERCP fluoroscopy image demonstrating contrast extravasation from the pancreatic duct into the pseudoaneurysm.
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Ibrahim Reyaz indicated no relevant financial relationships.
Christopher Ward indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Ishan Antony, MD1, Ibrahim Reyaz, MBBS2, Christopher Ward, MD3, Narinderjeet Kaur, MD, MS4, Khaldoon Khirfan, MD3. P5740 - Endoscopic Ultrasound With Coiling for Treatment of Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Ishan Antony, MD1, Ibrahim Reyaz, MBBS2, Christopher Ward, MD3, Narinderjeet Kaur, MD, MS4, Khaldoon Khirfan, MD3
1Beth Israel Lahey Health, Burlington, MA; 2Nassau University Medical Center, East Meadow, NY; 3Lahey Hospital and Medical Center, Burlington, MA; 4SUNY Downstate Health Sciences University, Brooklyn, NY
Introduction: Hemosuccus pancreaticus (HP) is a rare cause of upper gastrointestinal bleeding (GIB) typically caused by pseudoaneurysms of branches of the splenic artery. Embolization by interventional radiology is the main treatment modality, and sometimes surgery is required for refractory cases.
Case Description/
Methods: A 48-year-old woman with chronic pancreatitis due to alcohol, recent exacerbation with acute pancreatitis a few weeks before admission, splenic vein thrombosis, and a symptomatic 9 cm pseudocyst. The patient underwent endoscopic ultrasound (EUS)-guided cystgastrostomy with a lumen-apposing metal stent (LAMS). During admission, the patient started developing melena and shock. EGD was performed, which showed no evidence of bleeding at the cystgastrostomy. There was evidence of active bleeding from the site of the papilla consistent with HP. Computed tomography (CT) scan showed a 2 cm splenic artery aneurysm with active bleeding. Angiography with balloon-assisted splenic artery embolization was performed, but was not successful in achieving hemostasis. At that point, the patient was referred to our facility for further management.
The case was discussed with the multidisciplinary team. The consensus was to attempt EUS-guided treatment of the pseudoaneurysm. EUS showed a splenic artery pseudoaneurysm with artifact from the previously placed coils. Coiling of the pseudoaneurysm was performed using the 19 GA fine needle biopsy (FNA) needle using 14 cm-long cylindrical coils, followed by gel foam injection. There was immediate cessation of the bleeding at the site of the papilla. The patient tolerated the procedure without complication and remained transfusion-free for 48 hours before rebleeding.
Given persistent hemorrhage, surgical option was considered. In preparation for surgery, endoscopic retrograde pancreatography (ERP) was performed to evaluate the integrity of the pancreatic duct. ERP revealed contrast extravasation from the pancreatic duct in the tail into the pseudoaneurysm. The patient underwent distal pancreatectomy, splenectomy, and surgical debridement of the necrotic walled-off necrosis. The patient had an uneventful postoperative course.
Discussion: This case highlights the importance of considering HP in patients with chronic pancreatitis with GIB. Arteriography with embolization and vascular stenting is the main modality of treatment. Traditionally, surgery has been considered for refractory cases. EUS may have a promising role in the management of HP.
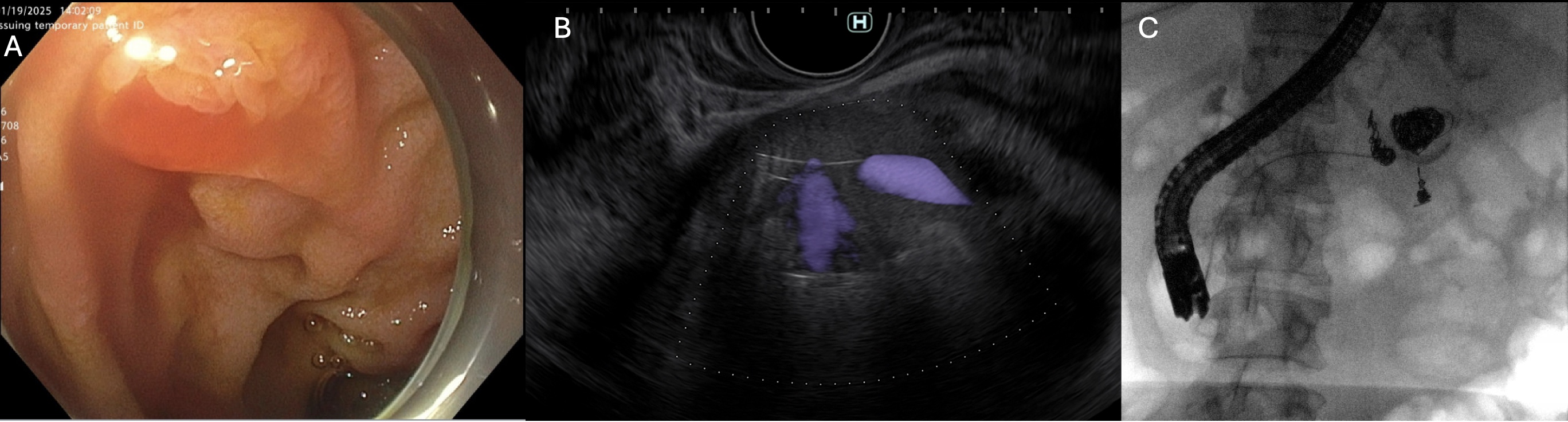
Figure: Figure 1: A) EGD image capturing active bleeding from the ampulla, B) EUS showed pseudoaneurysm with coils and active blood flow. C) ERCP fluoroscopy image demonstrating contrast extravasation from the pancreatic duct into the pseudoaneurysm.
Disclosures:
Ishan Antony indicated no relevant financial relationships.
Ibrahim Reyaz indicated no relevant financial relationships.
Christopher Ward indicated no relevant financial relationships.
Narinderjeet Kaur indicated no relevant financial relationships.
Khaldoon Khirfan indicated no relevant financial relationships.
Ishan Antony, MD1, Ibrahim Reyaz, MBBS2, Christopher Ward, MD3, Narinderjeet Kaur, MD, MS4, Khaldoon Khirfan, MD3. P5740 - Endoscopic Ultrasound With Coiling for Treatment of Hemosuccus Pancreaticus, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

