Tuesday Poster Session
Category: Liver
P5820 - Palliative Care Referrals Among Primary Care Patients With Cirrhosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Samantha Parks, MD (she/her/hers)
Medical University of South Carolina
Charleston, SC
Presenting Author(s)
Samantha Parks, MD, Andrew Schreiner, MD, MSCR, Amanda Overstreet, DO
Medical University of South Carolina, Charleston, SC
Introduction: Cirrhosis is a life-limiting chronic illness associated with a high physical and psychological symptom burden yet there remains significant inequality in the provision of palliative care and symptom-based management for patients with advanced liver disease. In response to this identified care gap, the American Gastroenterological Association (AGA) recently released a clinical practice update that recommends any patient with cirrhosis, irrespective of transplant candidacy or compensation status, receive referral to palliative care. We investigated the proportion of primary care patients diagnosed with cirrhosis that received a referral to palliative care in the outpatient setting.
Methods: We performed a retrospective cohort study of electronic health record data from a primary care clinic to determine the proportion of patients with diagnoses of cirrhosis, a complication of cirrhosis, or hepatocellular carcinoma (HCC) that received a specialty referral to ambulatory Palliative Care. Other variables gathered included demographic variables of patient age, sex, race, marital status, remote residential status, and insurance status. We performed univariate and bivariate analyses to describe the cohort and compare patient variables by palliative care referral status using two sample t tests for continuous variables and Chi square and Fisher’s exact tests for categorical variables. All statistical analyses were performed using SAS 9.4 (Cary, NC).
Results: We identified 732 eligible patients seen in primary care clinic between July 1, 2012 and December 31, 2023. Of those individuals, only 26 (3.55%) received a Palliative Care referral. A significantly lower proportion of patients receiving a referral were Female (27%), compared to patients not referred (48%, p=0.034, Table 1). There were no significant differences in referral status by race (p=0.670), marital status (p=0.300), remote residence (p=1.000), or payor (0.730).
Discussion: This study highlights that recent efforts advocating for the role of palliative care in patients with advanced liver disease have not yet translated into clinical practice. Considering that early provision of palliative care has been shown to improve quality of life, decrease symptom burden, and potentially reduce health-care use, this remains a substantial gap in the quality of care we provide to this population.
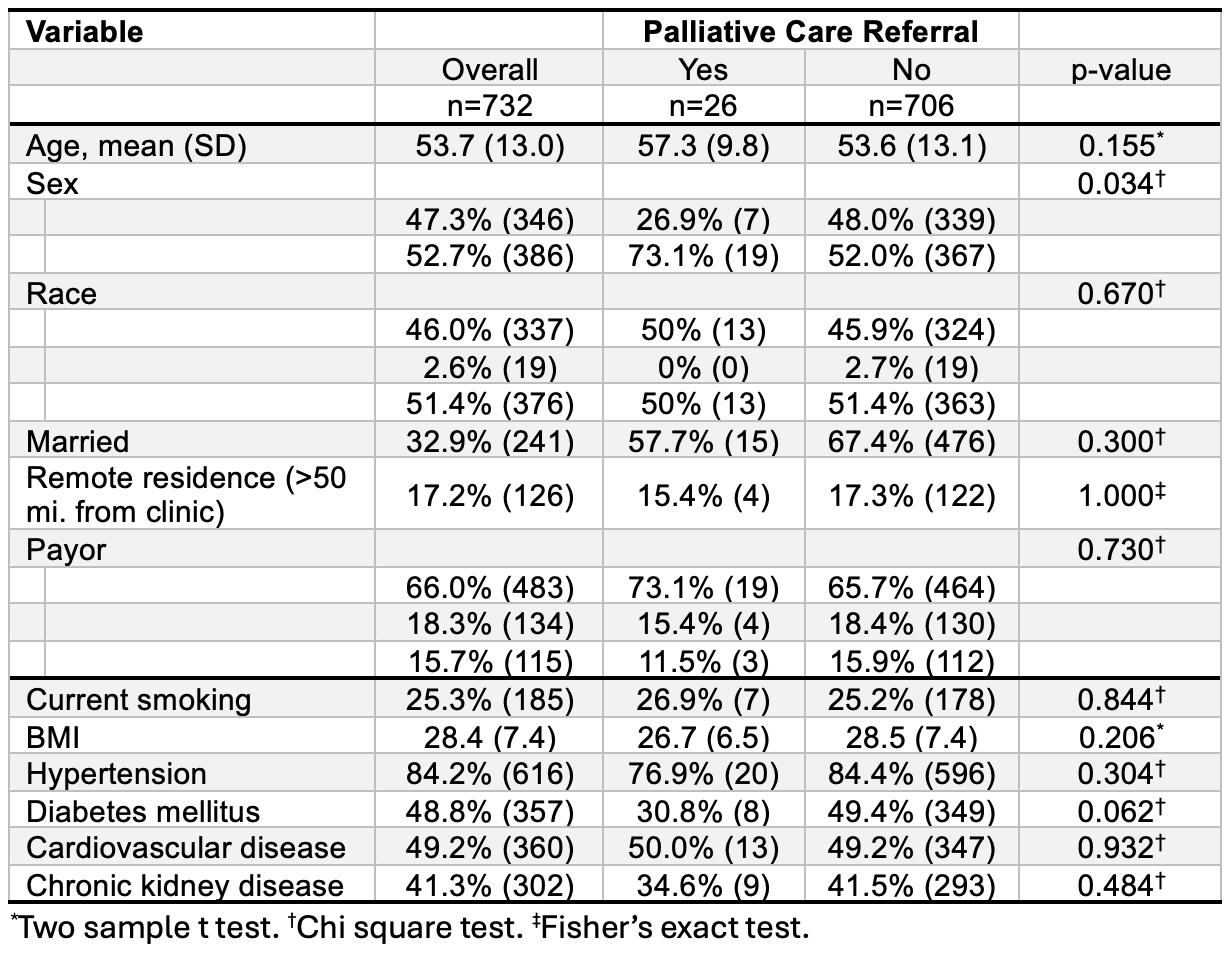
Figure: Table 1. Study cohort characteristics overall and by receipt of a referral for palliative care.
Disclosures:
Samantha Parks indicated no relevant financial relationships.
Andrew Schreiner indicated no relevant financial relationships.
Amanda Overstreet indicated no relevant financial relationships.
Samantha Parks, MD, Andrew Schreiner, MD, MSCR, Amanda Overstreet, DO. P5820 - Palliative Care Referrals Among Primary Care Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Medical University of South Carolina, Charleston, SC
Introduction: Cirrhosis is a life-limiting chronic illness associated with a high physical and psychological symptom burden yet there remains significant inequality in the provision of palliative care and symptom-based management for patients with advanced liver disease. In response to this identified care gap, the American Gastroenterological Association (AGA) recently released a clinical practice update that recommends any patient with cirrhosis, irrespective of transplant candidacy or compensation status, receive referral to palliative care. We investigated the proportion of primary care patients diagnosed with cirrhosis that received a referral to palliative care in the outpatient setting.
Methods: We performed a retrospective cohort study of electronic health record data from a primary care clinic to determine the proportion of patients with diagnoses of cirrhosis, a complication of cirrhosis, or hepatocellular carcinoma (HCC) that received a specialty referral to ambulatory Palliative Care. Other variables gathered included demographic variables of patient age, sex, race, marital status, remote residential status, and insurance status. We performed univariate and bivariate analyses to describe the cohort and compare patient variables by palliative care referral status using two sample t tests for continuous variables and Chi square and Fisher’s exact tests for categorical variables. All statistical analyses were performed using SAS 9.4 (Cary, NC).
Results: We identified 732 eligible patients seen in primary care clinic between July 1, 2012 and December 31, 2023. Of those individuals, only 26 (3.55%) received a Palliative Care referral. A significantly lower proportion of patients receiving a referral were Female (27%), compared to patients not referred (48%, p=0.034, Table 1). There were no significant differences in referral status by race (p=0.670), marital status (p=0.300), remote residence (p=1.000), or payor (0.730).
Discussion: This study highlights that recent efforts advocating for the role of palliative care in patients with advanced liver disease have not yet translated into clinical practice. Considering that early provision of palliative care has been shown to improve quality of life, decrease symptom burden, and potentially reduce health-care use, this remains a substantial gap in the quality of care we provide to this population.
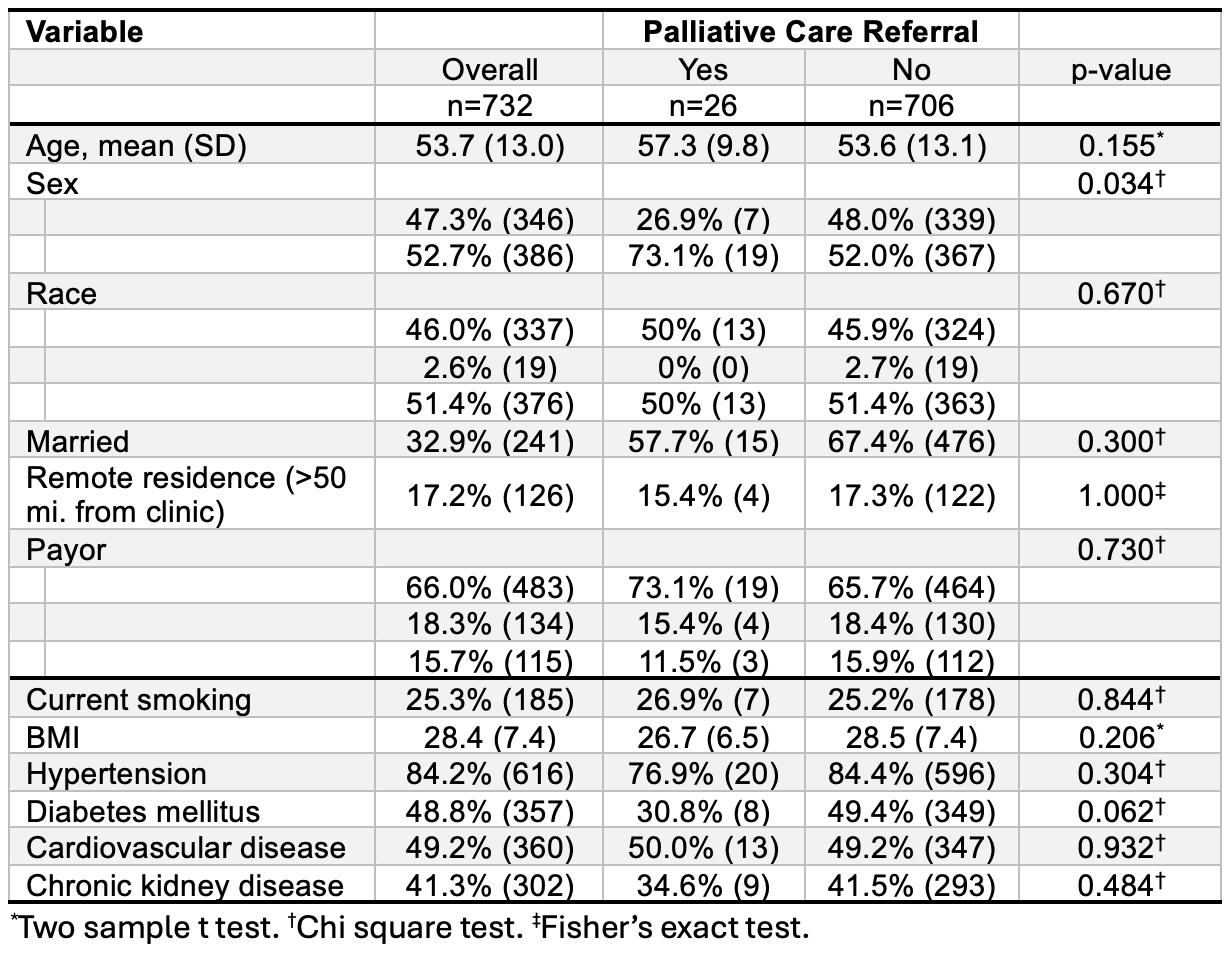
Figure: Table 1. Study cohort characteristics overall and by receipt of a referral for palliative care.
Disclosures:
Samantha Parks indicated no relevant financial relationships.
Andrew Schreiner indicated no relevant financial relationships.
Amanda Overstreet indicated no relevant financial relationships.
Samantha Parks, MD, Andrew Schreiner, MD, MSCR, Amanda Overstreet, DO. P5820 - Palliative Care Referrals Among Primary Care Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
