Tuesday Poster Session
Category: Liver
P5813 - Use of Beta Blockers in Spontaneous Bacterial Peritonitis Confers a Survival Benefit: A Retrospective Analysis of the MIMIC-IV Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Tejas Nikumbh, MD (he/him/his)
The Wright Center for Graduate Medical Education
Dunmore, PA
Presenting Author(s)
Tejas Nikumbh, MD1, Talha Liaqat, MBBS1, Himani Mongia, MD2, Sunny Kumar, MD3, Udit Asija, MD4, Vikas Khurana, MD, MBA2
1The Wright Center for Graduate Medical Education, Dunmore, PA; 2The Wright Center for Graduate Medical Education, Scranton, PA; 3Wright Center for Graduate Medical Education, Scranton, PA; 4The Wright Center for Graduate Medical Education, Throop, PA
Introduction: Spontaneous bacterial peritonitis (SBP) is a severe complication in cirrhotic patients. Nonselective beta-blockers (NSBB) have long been used to reduce portal pressure and variceal bleeding; however, the relationship between beta-blocker use and SBP outcomes is not well established. We aimed to determine whether NSBB confers a mortality benefit, decreases hepatorenal syndrome (HRS), influences mean arterial pressure (MAP) and variceal bleeding in SBP patients.
Methods: All adult admissions coded for SBP through no-decimal ICD codes were identified from the MIMIC-IV database. NSBB prescriptions were extracted by matching relevant drug names. Statistical analysis included chi-square tests for mortality, HRS, and variceal bleeding, as well as a Welch’s t-test for MAP. Logistic regressions (adjusted for age and gender) were performed to examine the independent association of beta-blockers with mortality, HRS, and variceal bleeding, and a linear regression addressed MAP.
Results: Out of 1597 SBP admissions, 654 (41%) had received at least one NSBB. Patients on NSBB had a slightly higher mean age (58.9 vs. 55.6 years) yet exhibited a lower in-hospital mortality (14.5% vs. 20.1%, p=0.0048) and reduced HRS incidence (13.8% vs. 18.2%, p=0.021). However, a higher proportion of patients using NSBB experienced variceal bleeding (17.9% vs. 7.1%, p< 0.0001). Mean MAP did not significantly differ between groups (90.96 vs. 90.73 mmHg, p=0.7631). In adjusted logistic regressions, NSBB use remained associated with reduced mortality (OR < 1) and showed a trend toward lower odds of HRS, but was strongly linked to an increased odds of variceal bleeding (OR > 1).
Discussion: Our findings suggest that in patients presenting with SBP, beta-blocker therapy may correlate with notable survival benefits and reduced HRS rates—even after accounting for age and gender. A higher incidence of variceal bleeding could be due to potential confounding and patient selection factors which are inherent to a retrospective database analysis. Although NSBB are traditionally prescribed to prevent variceal hemorrhage, our analysis highlights the complexity of managing advanced liver disease and the possibility that sicker patients or patients with previous history of variceal bleeding are more likely to receive these medications. The effect of NSBB on portal hemodynamics, and infection outcomes remains multifactorial, requiring further prospective validation to determine optimal therapeutic strategies for SBP management.
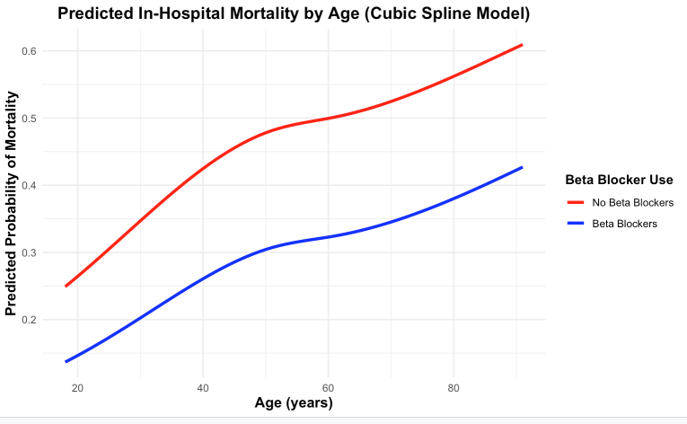
Figure: Predicted in-hospital mortality by age among patients with SBP using non-selective beta-blockers (NSBB) vs not using NSBB
Disclosures:
Tejas Nikumbh indicated no relevant financial relationships.
Talha Liaqat indicated no relevant financial relationships.
Himani Mongia indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Udit Asija indicated no relevant financial relationships.
Vikas Khurana indicated no relevant financial relationships.
Tejas Nikumbh, MD1, Talha Liaqat, MBBS1, Himani Mongia, MD2, Sunny Kumar, MD3, Udit Asija, MD4, Vikas Khurana, MD, MBA2. P5813 - Use of Beta Blockers in Spontaneous Bacterial Peritonitis Confers a Survival Benefit: A Retrospective Analysis of the MIMIC-IV Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Wright Center for Graduate Medical Education, Dunmore, PA; 2The Wright Center for Graduate Medical Education, Scranton, PA; 3Wright Center for Graduate Medical Education, Scranton, PA; 4The Wright Center for Graduate Medical Education, Throop, PA
Introduction: Spontaneous bacterial peritonitis (SBP) is a severe complication in cirrhotic patients. Nonselective beta-blockers (NSBB) have long been used to reduce portal pressure and variceal bleeding; however, the relationship between beta-blocker use and SBP outcomes is not well established. We aimed to determine whether NSBB confers a mortality benefit, decreases hepatorenal syndrome (HRS), influences mean arterial pressure (MAP) and variceal bleeding in SBP patients.
Methods: All adult admissions coded for SBP through no-decimal ICD codes were identified from the MIMIC-IV database. NSBB prescriptions were extracted by matching relevant drug names. Statistical analysis included chi-square tests for mortality, HRS, and variceal bleeding, as well as a Welch’s t-test for MAP. Logistic regressions (adjusted for age and gender) were performed to examine the independent association of beta-blockers with mortality, HRS, and variceal bleeding, and a linear regression addressed MAP.
Results: Out of 1597 SBP admissions, 654 (41%) had received at least one NSBB. Patients on NSBB had a slightly higher mean age (58.9 vs. 55.6 years) yet exhibited a lower in-hospital mortality (14.5% vs. 20.1%, p=0.0048) and reduced HRS incidence (13.8% vs. 18.2%, p=0.021). However, a higher proportion of patients using NSBB experienced variceal bleeding (17.9% vs. 7.1%, p< 0.0001). Mean MAP did not significantly differ between groups (90.96 vs. 90.73 mmHg, p=0.7631). In adjusted logistic regressions, NSBB use remained associated with reduced mortality (OR < 1) and showed a trend toward lower odds of HRS, but was strongly linked to an increased odds of variceal bleeding (OR > 1).
Discussion: Our findings suggest that in patients presenting with SBP, beta-blocker therapy may correlate with notable survival benefits and reduced HRS rates—even after accounting for age and gender. A higher incidence of variceal bleeding could be due to potential confounding and patient selection factors which are inherent to a retrospective database analysis. Although NSBB are traditionally prescribed to prevent variceal hemorrhage, our analysis highlights the complexity of managing advanced liver disease and the possibility that sicker patients or patients with previous history of variceal bleeding are more likely to receive these medications. The effect of NSBB on portal hemodynamics, and infection outcomes remains multifactorial, requiring further prospective validation to determine optimal therapeutic strategies for SBP management.
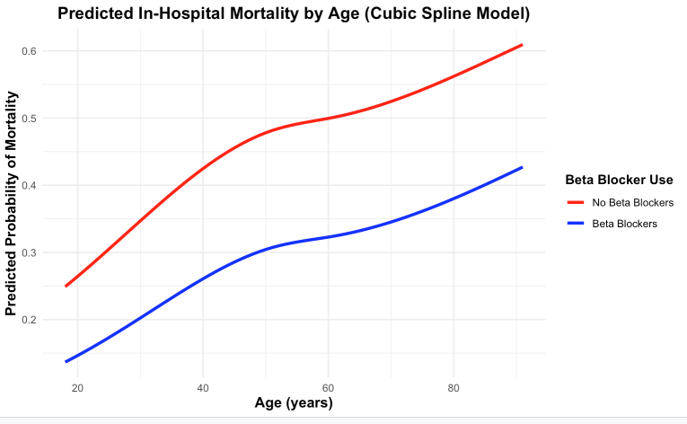
Figure: Predicted in-hospital mortality by age among patients with SBP using non-selective beta-blockers (NSBB) vs not using NSBB
Disclosures:
Tejas Nikumbh indicated no relevant financial relationships.
Talha Liaqat indicated no relevant financial relationships.
Himani Mongia indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Udit Asija indicated no relevant financial relationships.
Vikas Khurana indicated no relevant financial relationships.
Tejas Nikumbh, MD1, Talha Liaqat, MBBS1, Himani Mongia, MD2, Sunny Kumar, MD3, Udit Asija, MD4, Vikas Khurana, MD, MBA2. P5813 - Use of Beta Blockers in Spontaneous Bacterial Peritonitis Confers a Survival Benefit: A Retrospective Analysis of the MIMIC-IV Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
