Tuesday Poster Session
Category: Liver
P5812 - Association Between Metabolic Dysfunction Associated Steatotic Liver Disease and Cardiovascular Disease in Inflammatory Bowel Disease: A Retrospective Analysis from a Tertiary Care Centre
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Fariha Hasan, MD
Cooper University Hospital
Camden, NJ
Presenting Author(s)
Fariha Hasan, MD1, Christina Kanagawa, DO1, Daniel Guirguis, MD, MS2, Nikhil Kota, BS3, Subhadra Thampi, BS4, Zeina Issa, BS5, Harshini Suresh, MBA, BA, BS6, Shahryar Khan, MD7, Hareesha Rishab Bharadwaj, 8, Alexander Garcia, DO1, Avneet Singh, DO1, Krystal Hunter, PhD, MBA1, Satyajeet Roy, MD1
1Cooper University Hospital, Camden, NJ; 2St. Luke's University Hospital, Hatfield, PA; 3Cooper Medical School of Rowan University, Plainsboro, NJ; 4Cooper Medical School of Rowan University, Dayton, NJ; 5Cooper Medical School of Rowan University, Camden, NJ; 6Cooper Medical School of Rowan University, Jericho, NY; 7University of Kansas Medical Center, Kansas City, KS; 8The University of Manchester, Manchester, England, United Kingdom
Introduction: Cardiovascular disease (CVD) remains the leading cause of mortality worldwide. Emerging evidence suggests that both inflammatory bowel disease (IBD) and metabolic-dysfunction-associated-steatotic-liver-disease (MASLD) independently increase cardiovascular risk. However, the impact of MASLD on cardiovascular outcomes, specifically within the IBD population, is not well characterized. This study aimed to evaluate the prevalence of cardiovascular comorbidities in patients with IBD, with and without coexisting MASLD, to better understand additive risk and guide screening practices.
Methods: We conducted a retrospective electronic medical record review of all adult patients ( >18 years) with a diagnosis of IBD at a tertiary care center. Patients were divided into two groups: those with IBD alone and those with both IBD and imaging evidence of MASLD. Outcomes included cardiovascular associations between IBD and MASLD. Categorical variables were analyzed using chi-square or Fisher’s exact tests, and continuous variables with independent t-tests.
Results: A total of 317 patients with IBD were included, with 125 (39.4%) having coexisting metabolic MASLD. Patients in the IBD+MASLD group were significantly older (mean 58.5 vs. 53.0 years, p< 0.001).
The prevalence of coronary artery disease (CAD) was significantly higher in patients with IBD and MASLD compared to IBD alone (16.0% vs. 7.8%, p=0.023). Similarly, hypertension (54.4% vs. 39.6%, p=0.010) and hyperlipidemia (69.6% vs. 38.5%, p< 0.001) were more common in the IBD+MASLD group. Diabetes mellitus also showed a significant association (36.0% vs. 14.1%, p< 0.001), as did cirrhosis (5.6% vs. 1.6%, p=0.044) and history of hypothyroidism (18.4% vs. 9.9%, p=0.029). There were no significant differences in the prevalence of heart failure (4.8% vs. 3.1%, p=0.451) or CVA/TIA (5.6% vs. 2.6%, p=0.172). Medication analysis revealed that patients with IBD+MASLD were more likely to be on statins (73.4% vs. 26.6%, p< 0.001), ACE inhibitors/ARBs (87.5% vs. 12.5%, p< 0.001), beta blockers (25.6% vs. 14.6%, p=0.014), and insulin (16.8% vs. 4.2%, p< 0.001). Use of antiplatelets and anticoagulants did not differ significantly.
Discussion: We conclude that MASLD in IBD patients is associated with a significantly greater burden of cardiometabolic comorbidities and cardiovascular risk compared to those with IBD alone. These findings underscore the need for routine cardiovascular risk assessment and targeted interventions in this high-risk subgroup.
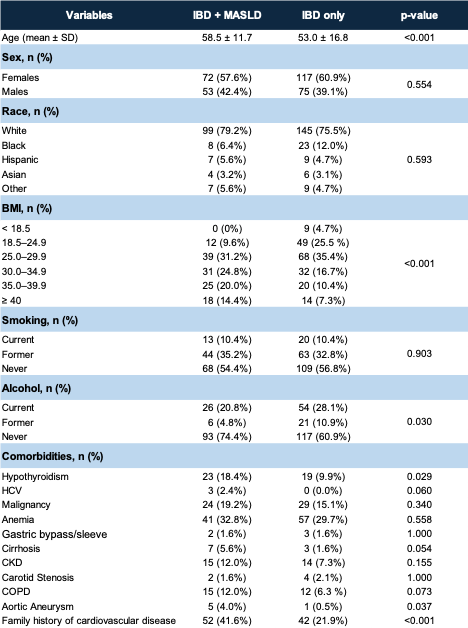
Figure: Table 1: Demographics between the two groups
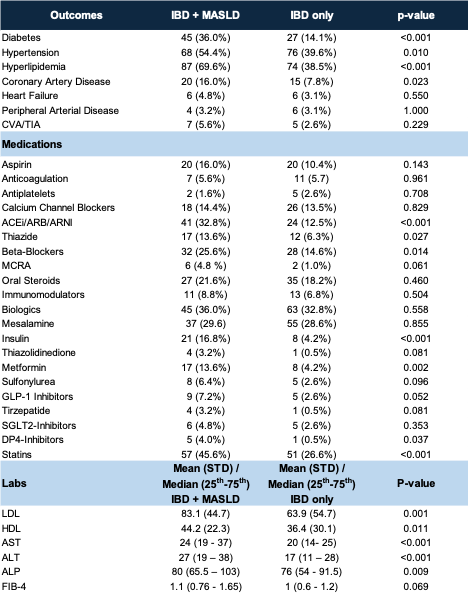
Figure: Table 2: Outcomes, medications and pertinent lab values between the two groups
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Christina Kanagawa indicated no relevant financial relationships.
Daniel Guirguis indicated no relevant financial relationships.
Nikhil Kota indicated no relevant financial relationships.
Subhadra Thampi indicated no relevant financial relationships.
Zeina Issa indicated no relevant financial relationships.
Harshini Suresh indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Satyajeet Roy indicated no relevant financial relationships.
Fariha Hasan, MD1, Christina Kanagawa, DO1, Daniel Guirguis, MD, MS2, Nikhil Kota, BS3, Subhadra Thampi, BS4, Zeina Issa, BS5, Harshini Suresh, MBA, BA, BS6, Shahryar Khan, MD7, Hareesha Rishab Bharadwaj, 8, Alexander Garcia, DO1, Avneet Singh, DO1, Krystal Hunter, PhD, MBA1, Satyajeet Roy, MD1. P5812 - Association Between Metabolic Dysfunction Associated Steatotic Liver Disease and Cardiovascular Disease in Inflammatory Bowel Disease: A Retrospective Analysis from a Tertiary Care Centre, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cooper University Hospital, Camden, NJ; 2St. Luke's University Hospital, Hatfield, PA; 3Cooper Medical School of Rowan University, Plainsboro, NJ; 4Cooper Medical School of Rowan University, Dayton, NJ; 5Cooper Medical School of Rowan University, Camden, NJ; 6Cooper Medical School of Rowan University, Jericho, NY; 7University of Kansas Medical Center, Kansas City, KS; 8The University of Manchester, Manchester, England, United Kingdom
Introduction: Cardiovascular disease (CVD) remains the leading cause of mortality worldwide. Emerging evidence suggests that both inflammatory bowel disease (IBD) and metabolic-dysfunction-associated-steatotic-liver-disease (MASLD) independently increase cardiovascular risk. However, the impact of MASLD on cardiovascular outcomes, specifically within the IBD population, is not well characterized. This study aimed to evaluate the prevalence of cardiovascular comorbidities in patients with IBD, with and without coexisting MASLD, to better understand additive risk and guide screening practices.
Methods: We conducted a retrospective electronic medical record review of all adult patients ( >18 years) with a diagnosis of IBD at a tertiary care center. Patients were divided into two groups: those with IBD alone and those with both IBD and imaging evidence of MASLD. Outcomes included cardiovascular associations between IBD and MASLD. Categorical variables were analyzed using chi-square or Fisher’s exact tests, and continuous variables with independent t-tests.
Results: A total of 317 patients with IBD were included, with 125 (39.4%) having coexisting metabolic MASLD. Patients in the IBD+MASLD group were significantly older (mean 58.5 vs. 53.0 years, p< 0.001).
The prevalence of coronary artery disease (CAD) was significantly higher in patients with IBD and MASLD compared to IBD alone (16.0% vs. 7.8%, p=0.023). Similarly, hypertension (54.4% vs. 39.6%, p=0.010) and hyperlipidemia (69.6% vs. 38.5%, p< 0.001) were more common in the IBD+MASLD group. Diabetes mellitus also showed a significant association (36.0% vs. 14.1%, p< 0.001), as did cirrhosis (5.6% vs. 1.6%, p=0.044) and history of hypothyroidism (18.4% vs. 9.9%, p=0.029). There were no significant differences in the prevalence of heart failure (4.8% vs. 3.1%, p=0.451) or CVA/TIA (5.6% vs. 2.6%, p=0.172). Medication analysis revealed that patients with IBD+MASLD were more likely to be on statins (73.4% vs. 26.6%, p< 0.001), ACE inhibitors/ARBs (87.5% vs. 12.5%, p< 0.001), beta blockers (25.6% vs. 14.6%, p=0.014), and insulin (16.8% vs. 4.2%, p< 0.001). Use of antiplatelets and anticoagulants did not differ significantly.
Discussion: We conclude that MASLD in IBD patients is associated with a significantly greater burden of cardiometabolic comorbidities and cardiovascular risk compared to those with IBD alone. These findings underscore the need for routine cardiovascular risk assessment and targeted interventions in this high-risk subgroup.
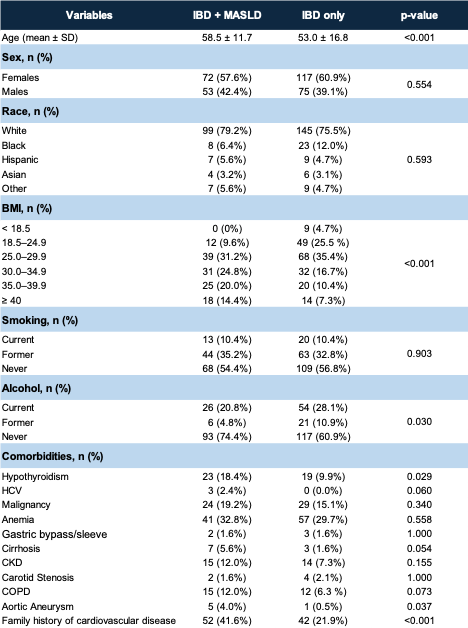
Figure: Table 1: Demographics between the two groups
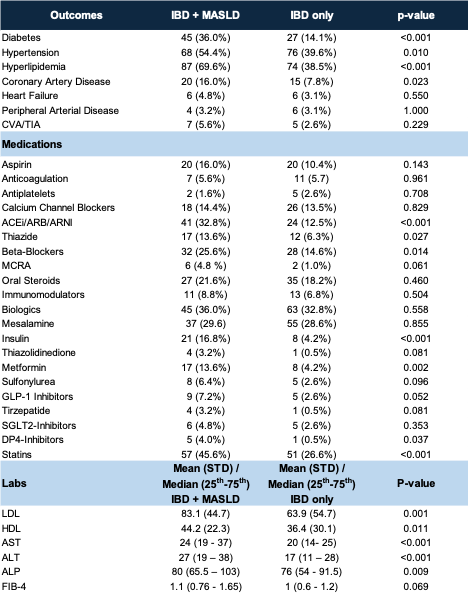
Figure: Table 2: Outcomes, medications and pertinent lab values between the two groups
Disclosures:
Fariha Hasan indicated no relevant financial relationships.
Christina Kanagawa indicated no relevant financial relationships.
Daniel Guirguis indicated no relevant financial relationships.
Nikhil Kota indicated no relevant financial relationships.
Subhadra Thampi indicated no relevant financial relationships.
Zeina Issa indicated no relevant financial relationships.
Harshini Suresh indicated no relevant financial relationships.
Shahryar Khan indicated no relevant financial relationships.
Hareesha Rishab Bharadwaj indicated no relevant financial relationships.
Alexander Garcia indicated no relevant financial relationships.
Avneet Singh indicated no relevant financial relationships.
Krystal Hunter indicated no relevant financial relationships.
Satyajeet Roy indicated no relevant financial relationships.
Fariha Hasan, MD1, Christina Kanagawa, DO1, Daniel Guirguis, MD, MS2, Nikhil Kota, BS3, Subhadra Thampi, BS4, Zeina Issa, BS5, Harshini Suresh, MBA, BA, BS6, Shahryar Khan, MD7, Hareesha Rishab Bharadwaj, 8, Alexander Garcia, DO1, Avneet Singh, DO1, Krystal Hunter, PhD, MBA1, Satyajeet Roy, MD1. P5812 - Association Between Metabolic Dysfunction Associated Steatotic Liver Disease and Cardiovascular Disease in Inflammatory Bowel Disease: A Retrospective Analysis from a Tertiary Care Centre, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

