Tuesday Poster Session
Category: Liver
P5807 - Association Between Chronic PPI Therapy and Hepatic Encephalopathy in Cirrhosis: A Retrospective Dose-Stratified Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nakul Mahajan, MBBS (he/him/his)
Maimonides Medical Center
Brooklyn, NY
Presenting Author(s)
Ahmed Salem, MD1, Sarah Meribout, MD1, Hazem Abosheaishaa, MD2, Mohammed Abusuliman, MD3, Neha Sharma, MD1, Omar Abdelhalim, MD4, Islam Mohamed, MD5, Fatima Khan, MD1, Syed Mujtaba Baqir, MD1, Samantha Ehrlich, MD1, Samar Pal S. Sandhu, MBBS1, Rajdeep Singh, MD6, Islam Rajab, MD7, Avleen Kaur, MD8, Nakul Mahajan, MBBS1, Carla Barberan Parraga, MD1, Abdallah Hussein, MD9, Tanuj Chokshi, MD1, Joseph Menand, MD1, MariaLisa Itzoe, DO, MPH1, Bani Roland, MD10, Yuriy Tsirlin, MD1, Gerard Mullin, MD11, Mohammad Alomari, MD12, Mauricio Garcia, MD13, Aaron Z. Tokayer, MD, MHS1
1Maimonides Medical Center, Brooklyn, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 3Henry Ford Hospital, Detroit, MI; 4Icahn School of Medicine at Mount Sinai, Queens, NY; 5University of Missouri Columbia, Columbia, MO; 6PEACEHEALTH, Longview, WA; 7St. Joseph's University Medical Center, Paterson, NJ; 8SUNY Upstate Medical University, Syracuse, NY; 9Virtua Our Lady of Lourdes Hospital, Camden, NJ; 10Brooklyn VA Medical Center, Brooklyn, NY; 11Johns Hopkins University School of Medicine, Baltimore, MD; 12University of Arkansas, Little Rock, AR; 13University of Arkansas for Medical Sciences, Little Rock, AR
Introduction:
Background:
Despite widespread use, proton pump inhibitors (PPIs) have been implicated as a potential modifiable risk factor for hepatic encephalopathy (HE) in patients with cirrhosis. However, real-world data delineating this relationship remain limited, especially regarding dose and duration effects.
Aim:
To investigate the association between PPI use and risk of incident hepatic encephalopathy among cirrhotic patients, accounting for exposure duration and dose intensity.
Methods: We conducted a retrospective multicenter cohort study using TriNetX, aggregating EHRs from 90+ U.S. health systems. Adults (≥18 years) with cirrhosis (ICD-10: K70.3, K74.6, K76.9) from Jan 1, 2015–Dec 31, 2023 were included. Exclusions: prior HE, HCC, TIPS, or recent sepsis.
Patients were stratified into:
Index date was first PPI prescription or matched pseudo-date. All had ≥12 months follow-up. Propensity score matching (1:1:1) used age, sex, MELD-lab equivalents (bilirubin, INR, albumin, creatinine), comorbidities (diabetes, CKD, alcohol use, varices, ascites), and medications (lactulose, rifaximin, diuretics, NSAIDs, beta-blockers).
The primary outcome was incident HE within 12 months, defined via ICD-10 codes and initiation of lactulose or rifaximin. Cox models provided adjusted hazard ratios (aHRs), with Kaplan-Meier curves illustrating incidence.
Results: 18,991 patients met criteria (6,423 per group). Baseline variables were balanced (SMD < 0.1). Median follow-up: 11.2 months.
HE incidence:
Risk comparisons:
Findings were consistent across subgroups (alcoholic vs non-alcoholic cirrhosis, sex, MELD strata). Sensitivity analyses controlling for lactulose, rifaximin, and diuretic use confirmed robustness. KM curves showed early divergence by month 3.
Discussion: In cirrhotic patients, chronic PPI use—especially high-dose—was independently linked to increased HE risk. These real-world data support cautious PPI use, favoring dose reduction or discontinuation when appropriate. Prospective studies are needed to validate causality and mechanisms.
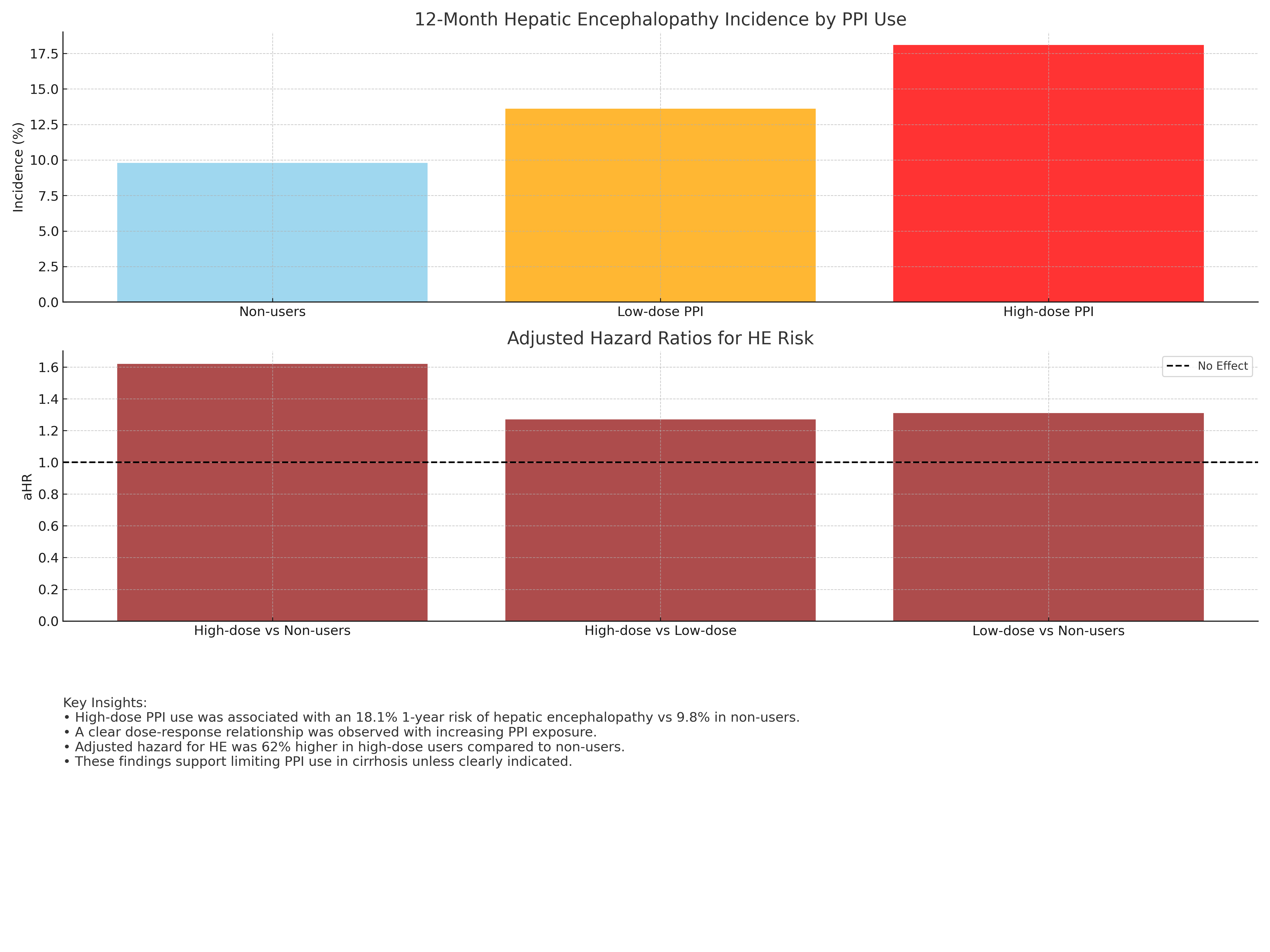
Figure: • High-dose PPl use was associated with an 18.1% 1-year risk of hepatic encephalopathy vs 9.8% in non-users.
• Adiested hazard or was 62% higher in niged we see as exposuresers.
• These findings support limiting PPI use in cirrhosis unless clearly indicated.
Disclosures:
Ahmed Salem indicated no relevant financial relationships.
Sarah Meribout indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Neha Sharma indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Fatima Khan indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Samantha Ehrlich indicated no relevant financial relationships.
Samar Pal Sandhu indicated no relevant financial relationships.
Rajdeep Singh indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Carla Barberan Parraga indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Joseph Menand indicated no relevant financial relationships.
MariaLisa Itzoe indicated no relevant financial relationships.
Bani Roland indicated no relevant financial relationships.
Yuriy Tsirlin indicated no relevant financial relationships.
Gerard Mullin indicated no relevant financial relationships.
Mohammad Alomari indicated no relevant financial relationships.
Mauricio Garcia indicated no relevant financial relationships.
Aaron Tokayer indicated no relevant financial relationships.
Ahmed Salem, MD1, Sarah Meribout, MD1, Hazem Abosheaishaa, MD2, Mohammed Abusuliman, MD3, Neha Sharma, MD1, Omar Abdelhalim, MD4, Islam Mohamed, MD5, Fatima Khan, MD1, Syed Mujtaba Baqir, MD1, Samantha Ehrlich, MD1, Samar Pal S. Sandhu, MBBS1, Rajdeep Singh, MD6, Islam Rajab, MD7, Avleen Kaur, MD8, Nakul Mahajan, MBBS1, Carla Barberan Parraga, MD1, Abdallah Hussein, MD9, Tanuj Chokshi, MD1, Joseph Menand, MD1, MariaLisa Itzoe, DO, MPH1, Bani Roland, MD10, Yuriy Tsirlin, MD1, Gerard Mullin, MD11, Mohammad Alomari, MD12, Mauricio Garcia, MD13, Aaron Z. Tokayer, MD, MHS1. P5807 - Association Between Chronic PPI Therapy and Hepatic Encephalopathy in Cirrhosis: A Retrospective Dose-Stratified Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Maimonides Medical Center, Brooklyn, NY; 2Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY; 3Henry Ford Hospital, Detroit, MI; 4Icahn School of Medicine at Mount Sinai, Queens, NY; 5University of Missouri Columbia, Columbia, MO; 6PEACEHEALTH, Longview, WA; 7St. Joseph's University Medical Center, Paterson, NJ; 8SUNY Upstate Medical University, Syracuse, NY; 9Virtua Our Lady of Lourdes Hospital, Camden, NJ; 10Brooklyn VA Medical Center, Brooklyn, NY; 11Johns Hopkins University School of Medicine, Baltimore, MD; 12University of Arkansas, Little Rock, AR; 13University of Arkansas for Medical Sciences, Little Rock, AR
Introduction:
Background:
Despite widespread use, proton pump inhibitors (PPIs) have been implicated as a potential modifiable risk factor for hepatic encephalopathy (HE) in patients with cirrhosis. However, real-world data delineating this relationship remain limited, especially regarding dose and duration effects.
Aim:
To investigate the association between PPI use and risk of incident hepatic encephalopathy among cirrhotic patients, accounting for exposure duration and dose intensity.
Methods: We conducted a retrospective multicenter cohort study using TriNetX, aggregating EHRs from 90+ U.S. health systems. Adults (≥18 years) with cirrhosis (ICD-10: K70.3, K74.6, K76.9) from Jan 1, 2015–Dec 31, 2023 were included. Exclusions: prior HE, HCC, TIPS, or recent sepsis.
Patients were stratified into:
Non-users (no PPI exposure)
Low-dose users (≤20 mg omeprazole-equivalent/day)
High-dose users (≥40 mg/day)
Index date was first PPI prescription or matched pseudo-date. All had ≥12 months follow-up. Propensity score matching (1:1:1) used age, sex, MELD-lab equivalents (bilirubin, INR, albumin, creatinine), comorbidities (diabetes, CKD, alcohol use, varices, ascites), and medications (lactulose, rifaximin, diuretics, NSAIDs, beta-blockers).
The primary outcome was incident HE within 12 months, defined via ICD-10 codes and initiation of lactulose or rifaximin. Cox models provided adjusted hazard ratios (aHRs), with Kaplan-Meier curves illustrating incidence.
Results: 18,991 patients met criteria (6,423 per group). Baseline variables were balanced (SMD < 0.1). Median follow-up: 11.2 months.
HE incidence:
High-dose: 18.1%
Low-dose: 13.6%
Non-users: 9.8% (log-rank p< 0.001)
Risk comparisons:
High-dose vs non-users: aHR 1.62 (95% CI: 1.39–1.87), p< 0.001
High-dose vs low-dose: aHR 1.27 (95% CI: 1.10–1.47), p=0.002
Low-dose vs non-users: aHR 1.31 (95% CI: 1.14–1.50), p< 0.001
Findings were consistent across subgroups (alcoholic vs non-alcoholic cirrhosis, sex, MELD strata). Sensitivity analyses controlling for lactulose, rifaximin, and diuretic use confirmed robustness. KM curves showed early divergence by month 3.
Discussion: In cirrhotic patients, chronic PPI use—especially high-dose—was independently linked to increased HE risk. These real-world data support cautious PPI use, favoring dose reduction or discontinuation when appropriate. Prospective studies are needed to validate causality and mechanisms.
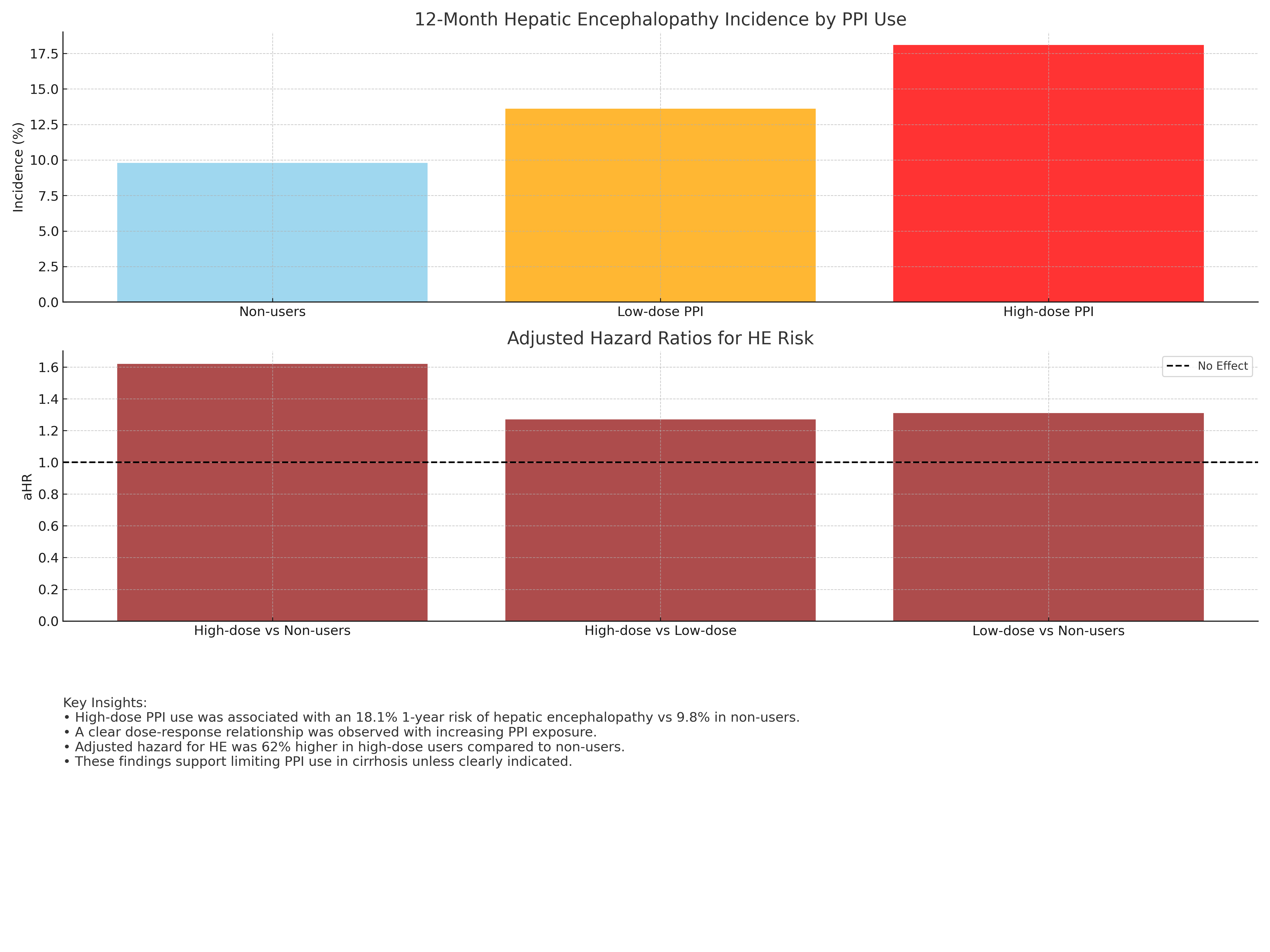
Figure: • High-dose PPl use was associated with an 18.1% 1-year risk of hepatic encephalopathy vs 9.8% in non-users.
• Adiested hazard or was 62% higher in niged we see as exposuresers.
• These findings support limiting PPI use in cirrhosis unless clearly indicated.
Disclosures:
Ahmed Salem indicated no relevant financial relationships.
Sarah Meribout indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohammed Abusuliman indicated no relevant financial relationships.
Neha Sharma indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Islam Mohamed indicated no relevant financial relationships.
Fatima Khan indicated no relevant financial relationships.
Syed Mujtaba Baqir indicated no relevant financial relationships.
Samantha Ehrlich indicated no relevant financial relationships.
Samar Pal Sandhu indicated no relevant financial relationships.
Rajdeep Singh indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Nakul Mahajan indicated no relevant financial relationships.
Carla Barberan Parraga indicated no relevant financial relationships.
Abdallah Hussein indicated no relevant financial relationships.
Tanuj Chokshi indicated no relevant financial relationships.
Joseph Menand indicated no relevant financial relationships.
MariaLisa Itzoe indicated no relevant financial relationships.
Bani Roland indicated no relevant financial relationships.
Yuriy Tsirlin indicated no relevant financial relationships.
Gerard Mullin indicated no relevant financial relationships.
Mohammad Alomari indicated no relevant financial relationships.
Mauricio Garcia indicated no relevant financial relationships.
Aaron Tokayer indicated no relevant financial relationships.
Ahmed Salem, MD1, Sarah Meribout, MD1, Hazem Abosheaishaa, MD2, Mohammed Abusuliman, MD3, Neha Sharma, MD1, Omar Abdelhalim, MD4, Islam Mohamed, MD5, Fatima Khan, MD1, Syed Mujtaba Baqir, MD1, Samantha Ehrlich, MD1, Samar Pal S. Sandhu, MBBS1, Rajdeep Singh, MD6, Islam Rajab, MD7, Avleen Kaur, MD8, Nakul Mahajan, MBBS1, Carla Barberan Parraga, MD1, Abdallah Hussein, MD9, Tanuj Chokshi, MD1, Joseph Menand, MD1, MariaLisa Itzoe, DO, MPH1, Bani Roland, MD10, Yuriy Tsirlin, MD1, Gerard Mullin, MD11, Mohammad Alomari, MD12, Mauricio Garcia, MD13, Aaron Z. Tokayer, MD, MHS1. P5807 - Association Between Chronic PPI Therapy and Hepatic Encephalopathy in Cirrhosis: A Retrospective Dose-Stratified Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

