Tuesday Poster Session
Category: Liver
P5876 - Analyzing the Trends in Admissions Related to Autoimmune Hepatitis and the Growing Burden on Healthcare: A Decade-Long National Study From the USA
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RV
Renuka Verma, MD (she/her/hers)
Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas
Las Vegas, NV
Presenting Author(s)
Renuka Verma, MD1, Tejas Joshi, MD2, Hafiz Zarsham Ali Ikram, MBBS3, Kamleshun Ramphul, MD4, Wesam Frandah, MD2
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Marshall University School of Medicine, Huntington, WV; 4Independent researcher, Las Vegas, NV
Introduction: Although some studies have suggested a rise in the incidence of
autoimmune hepatitis (AIH), data regarding hospitalization trends and healthcare burden is sparse. In this retrospective study, we aimed to describe the trends in AIH among all-cause admissions in
the United States over a decade and their growing healthcare burden.
Methods: We analyzed the 2012-2021 NIS. The presence of autoimmune hepatitis
was identified using (ICD)-9/ICD-10 codes “K754”. We estimated the year-by-year trends in hospitalizations of AIH relative to all-cause admissions, stratified by sex, age, and race, using Cochran–Armitage tests. The inflation-adjusted total hospital
costs(USD) were also compared over the ten years. A logistic regression model estimated
how age, sex, race, and year impacted the odds of having a higher than median cost of hospitalization.
Results: From 2012 to 2021, AIH-related hospitalizations increased from 55.2 cases per 100,000
admissions to 80.1 per 100,000 (ptrend < 0.01). Similar overall rising trends were noted based on sex, race,
and age groups, as described in Figures 1a, 1b, and 1c. Total costs rose from 290.5 million in 2012 to 477.2 million in
2021(Figure 1d)(ptrend< 0.01). Overall increments in cost were also observed in our stratified groups, as
demonstrated in Figures 1f, 1g, 1h, 1i, 1j, 1k, and 1l(ptrend< 0.01 throughout). A multivariable regression
model showed that the odds of reporting a hospital cost higher than median were higher among patients
ages 46-59 years (aOR 1.317, 95% CI 1.283- 1.352, p< 0.01) and ages ≥60 years(aOR 1.407, 95% CI
1.376-1.439, p< 0.01) (vs. Ages 18-45). Racial disparities were also seen as Blacks (aOR 1.173, 95% CI
1.143-1.204, p< 0.01), Hispanics(aOR 1.346, 95% CI 1.311-1.382, p< 0.01), and Asian Americans/Pacific-
islanders(AAPI)(aOR 1.827, 95% CI 1.724-1.937, p< 0.01) tended to be more likely to report higher than
median costs than Whites. The burden also followed an annual pattern (aOR 1.045, 95% CI 1.041-1.048,
p< 0.01). AIH admissions was higher among females than
males, they were less likely to report a hospital cost higher than the overall median(aOR 0.880, 95% CI
0.861-0.900, p< 0.01).
Discussion: This study confirmed that AIH is a growing healthcare concern and burden. In addition, racial,
sex-based, and age-based discrepancies in hospital costs were found. This calls for additional studies to
first identify at-risk groups for AIH and provide adequate screening and follow-ups to mitigate the risks of
severe hospitalizations.
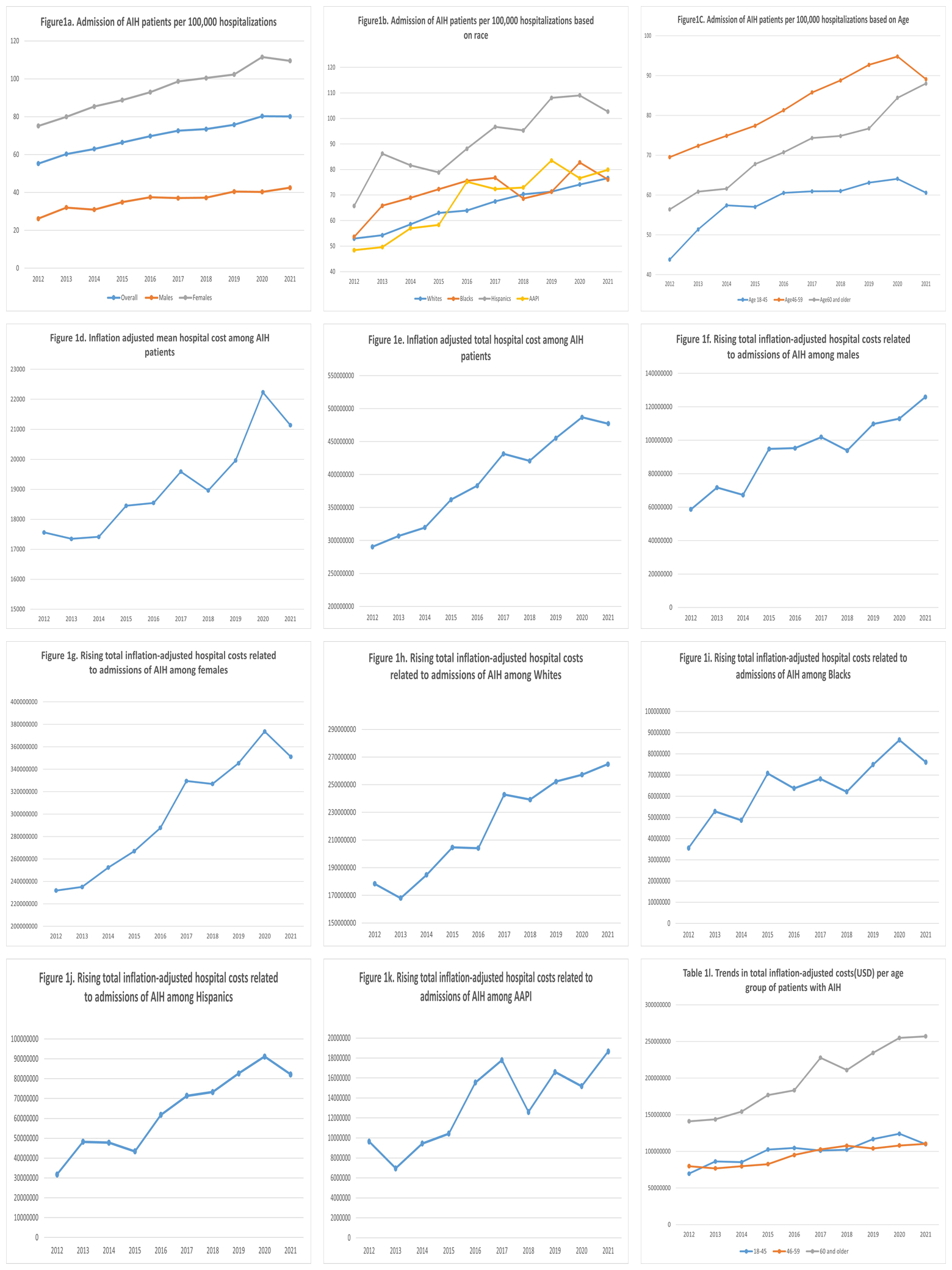
Figure: Statistical Analysis of Rising Trends and Cost Burden
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Tejas Joshi: Salix, Gilead, Echosens – Advisor or Review Panel Member, Consultant, Grant/Research Support.
Hafiz Zarsham Ali Ikram indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Renuka Verma, MD1, Tejas Joshi, MD2, Hafiz Zarsham Ali Ikram, MBBS3, Kamleshun Ramphul, MD4, Wesam Frandah, MD2. P5876 - Analyzing the Trends in Admissions Related to Autoimmune Hepatitis and the Growing Burden on Healthcare: A Decade-Long National Study From the USA, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada, Las Vegas, Las Vegas, NV; 2Marshall University Joan C. Edwards School of Medicine, Huntington, WV; 3Marshall University School of Medicine, Huntington, WV; 4Independent researcher, Las Vegas, NV
Introduction: Although some studies have suggested a rise in the incidence of
autoimmune hepatitis (AIH), data regarding hospitalization trends and healthcare burden is sparse. In this retrospective study, we aimed to describe the trends in AIH among all-cause admissions in
the United States over a decade and their growing healthcare burden.
Methods: We analyzed the 2012-2021 NIS. The presence of autoimmune hepatitis
was identified using (ICD)-9/ICD-10 codes “K754”. We estimated the year-by-year trends in hospitalizations of AIH relative to all-cause admissions, stratified by sex, age, and race, using Cochran–Armitage tests. The inflation-adjusted total hospital
costs(USD) were also compared over the ten years. A logistic regression model estimated
how age, sex, race, and year impacted the odds of having a higher than median cost of hospitalization.
Results: From 2012 to 2021, AIH-related hospitalizations increased from 55.2 cases per 100,000
admissions to 80.1 per 100,000 (ptrend < 0.01). Similar overall rising trends were noted based on sex, race,
and age groups, as described in Figures 1a, 1b, and 1c. Total costs rose from 290.5 million in 2012 to 477.2 million in
2021(Figure 1d)(ptrend< 0.01). Overall increments in cost were also observed in our stratified groups, as
demonstrated in Figures 1f, 1g, 1h, 1i, 1j, 1k, and 1l(ptrend< 0.01 throughout). A multivariable regression
model showed that the odds of reporting a hospital cost higher than median were higher among patients
ages 46-59 years (aOR 1.317, 95% CI 1.283- 1.352, p< 0.01) and ages ≥60 years(aOR 1.407, 95% CI
1.376-1.439, p< 0.01) (vs. Ages 18-45). Racial disparities were also seen as Blacks (aOR 1.173, 95% CI
1.143-1.204, p< 0.01), Hispanics(aOR 1.346, 95% CI 1.311-1.382, p< 0.01), and Asian Americans/Pacific-
islanders(AAPI)(aOR 1.827, 95% CI 1.724-1.937, p< 0.01) tended to be more likely to report higher than
median costs than Whites. The burden also followed an annual pattern (aOR 1.045, 95% CI 1.041-1.048,
p< 0.01). AIH admissions was higher among females than
males, they were less likely to report a hospital cost higher than the overall median(aOR 0.880, 95% CI
0.861-0.900, p< 0.01).
Discussion: This study confirmed that AIH is a growing healthcare concern and burden. In addition, racial,
sex-based, and age-based discrepancies in hospital costs were found. This calls for additional studies to
first identify at-risk groups for AIH and provide adequate screening and follow-ups to mitigate the risks of
severe hospitalizations.
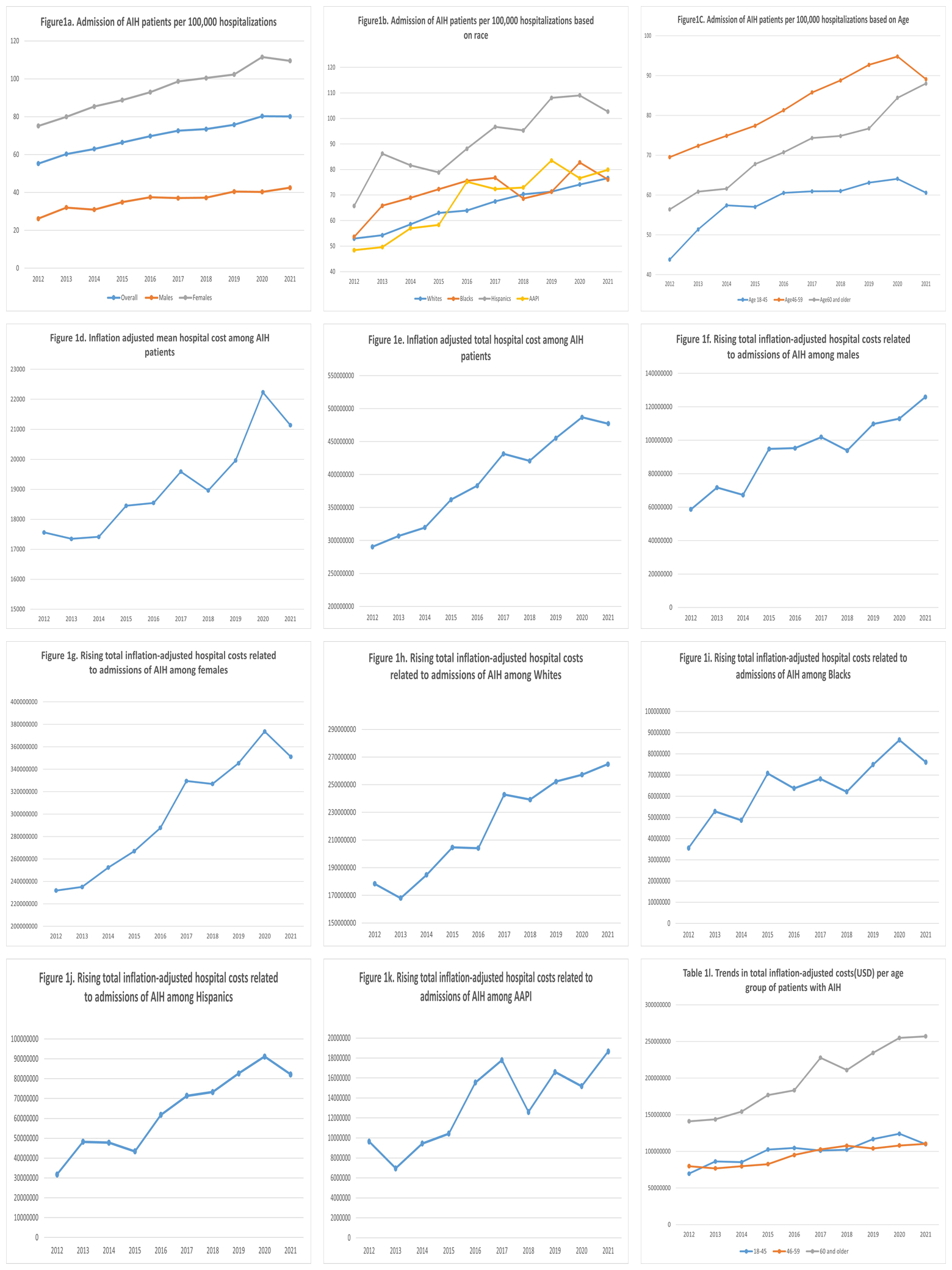
Figure: Statistical Analysis of Rising Trends and Cost Burden
Disclosures:
Renuka Verma indicated no relevant financial relationships.
Tejas Joshi: Salix, Gilead, Echosens – Advisor or Review Panel Member, Consultant, Grant/Research Support.
Hafiz Zarsham Ali Ikram indicated no relevant financial relationships.
Kamleshun Ramphul indicated no relevant financial relationships.
Wesam Frandah: Boston Scientific – Advisor or Review Panel Member, Consultant. Merritt – Consultant. Olympus corporation of America – Consultant.
Renuka Verma, MD1, Tejas Joshi, MD2, Hafiz Zarsham Ali Ikram, MBBS3, Kamleshun Ramphul, MD4, Wesam Frandah, MD2. P5876 - Analyzing the Trends in Admissions Related to Autoimmune Hepatitis and the Growing Burden on Healthcare: A Decade-Long National Study From the USA, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
