Tuesday Poster Session
Category: Liver
P5946 - The Role of Ammonia Testing in Hepatic Encephalopathy: A Quality Improvement Project
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Manasa Ginjupalli, MD
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Camelia Ciobanu, MD1, Manasa Ginjupalli, MD1, Amr Dokmak, MD1, Ali Wakil, MD1, Jeeva Jaganathan, MD2, Arnold Forlemu, MD1, Chaula Desai, MD1, Madhavi Reddy, MD2
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Serum ammonia is frequently used to diagnose hepatic encephalopathy (HE) in patients with cirrhosis and altered mental status. However, HE is a clinical diagnosis, and routine ammonia testing has limited utility in guiding its management. Ammonia elevations may result from various non-hepatic conditions, such as malignancy, rhabdomyolysis, and gastrointestinal bleeding. Despite evidence showing minimal clinical utility from routine ammonia testing, it remains commonly ordered in the inpatient setting. We implemented an educational initiative for internal medicine residents to enhance their knowledge and understanding of the appropriate use of ammonia testing in HE, promoting evidence-based clinical practice.
Methods: An educational session was conducted for internal medicine residents on the role of serum ammonia in the diagnosis, staging, treatment, and prognosis of HE. The session reviewed the latest American Association for the Study of Liver Diseases (AASLD) and European Association for the Study of Liver (EASL) guidelines, highlighting the pathophysiological role of ammonia and current recommendations regarding its use in HE management. Pre- and post-session questionnaires assessed participants’ knowledge and their willingness to incorporate evidence-based practices in future HE management.
Results: The educational session significantly improved participants’ understanding of the limited role of serum ammonia in the management of HE. Participants gained clarity on the lack of correlation between isolated serum ammonia levels and HE grade in patients with cirrhosis, limited role of trending ammonia levels or titrating the lactulose dose based on serum ammonia levels in cirrhotic patients [Image 1]. By the end of the session, 87% of participants recognized HE as a clinical diagnosis guided by the patient’s mental status, rather than laboratory ammonia values, compared to 65% prior to the session. Furthermore, the understanding of the prognostic value of ammonia testing in cirrhosis and acute liver failure showed significant improvement [Image 2].
Discussion: Our quality improvement initiative enhanced internal medicine residents' knowledge regarding the limited role of serum ammonia testing in the diagnosis, staging, treatment, and prognosis of hepatic encephalopathy in patients with known diagnosis of cirrhosis.
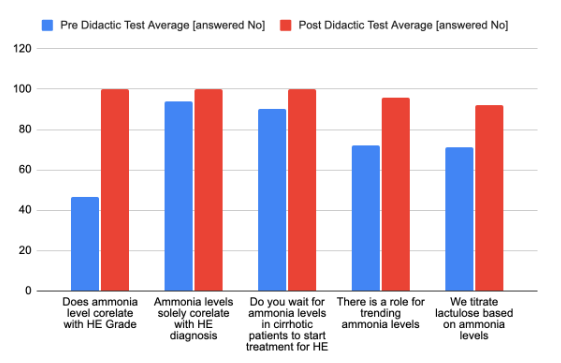
Figure: Image 1 - Improvement in the Knowledge pre and post Didactic session regarding the role of serum ammonia testing in Hepatic Encephalopathy
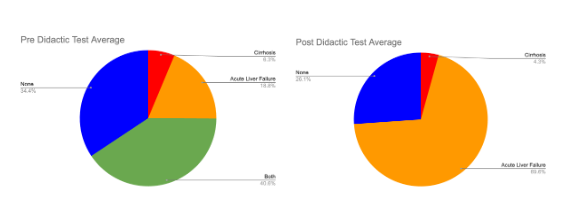
Figure: Image 2 - Improvement of knowledge regarding Prognostic utility of serum ammonium level among patients with cirrhosis and acute liver failure
Disclosures:
Camelia Ciobanu indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Jeeva Jaganathan indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Camelia Ciobanu, MD1, Manasa Ginjupalli, MD1, Amr Dokmak, MD1, Ali Wakil, MD1, Jeeva Jaganathan, MD2, Arnold Forlemu, MD1, Chaula Desai, MD1, Madhavi Reddy, MD2. P5946 - The Role of Ammonia Testing in Hepatic Encephalopathy: A Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2The Brooklyn Hospital Center, Brooklyn, NY
Introduction: Serum ammonia is frequently used to diagnose hepatic encephalopathy (HE) in patients with cirrhosis and altered mental status. However, HE is a clinical diagnosis, and routine ammonia testing has limited utility in guiding its management. Ammonia elevations may result from various non-hepatic conditions, such as malignancy, rhabdomyolysis, and gastrointestinal bleeding. Despite evidence showing minimal clinical utility from routine ammonia testing, it remains commonly ordered in the inpatient setting. We implemented an educational initiative for internal medicine residents to enhance their knowledge and understanding of the appropriate use of ammonia testing in HE, promoting evidence-based clinical practice.
Methods: An educational session was conducted for internal medicine residents on the role of serum ammonia in the diagnosis, staging, treatment, and prognosis of HE. The session reviewed the latest American Association for the Study of Liver Diseases (AASLD) and European Association for the Study of Liver (EASL) guidelines, highlighting the pathophysiological role of ammonia and current recommendations regarding its use in HE management. Pre- and post-session questionnaires assessed participants’ knowledge and their willingness to incorporate evidence-based practices in future HE management.
Results: The educational session significantly improved participants’ understanding of the limited role of serum ammonia in the management of HE. Participants gained clarity on the lack of correlation between isolated serum ammonia levels and HE grade in patients with cirrhosis, limited role of trending ammonia levels or titrating the lactulose dose based on serum ammonia levels in cirrhotic patients [Image 1]. By the end of the session, 87% of participants recognized HE as a clinical diagnosis guided by the patient’s mental status, rather than laboratory ammonia values, compared to 65% prior to the session. Furthermore, the understanding of the prognostic value of ammonia testing in cirrhosis and acute liver failure showed significant improvement [Image 2].
Discussion: Our quality improvement initiative enhanced internal medicine residents' knowledge regarding the limited role of serum ammonia testing in the diagnosis, staging, treatment, and prognosis of hepatic encephalopathy in patients with known diagnosis of cirrhosis.
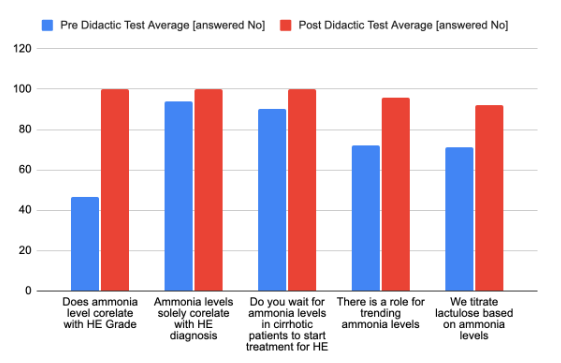
Figure: Image 1 - Improvement in the Knowledge pre and post Didactic session regarding the role of serum ammonia testing in Hepatic Encephalopathy
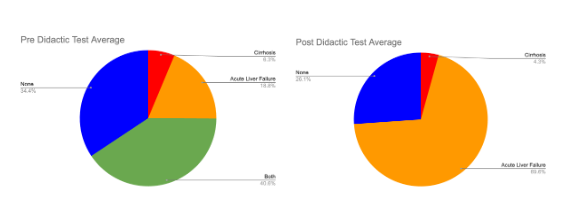
Figure: Image 2 - Improvement of knowledge regarding Prognostic utility of serum ammonium level among patients with cirrhosis and acute liver failure
Disclosures:
Camelia Ciobanu indicated no relevant financial relationships.
Manasa Ginjupalli indicated no relevant financial relationships.
Amr Dokmak indicated no relevant financial relationships.
Ali Wakil indicated no relevant financial relationships.
Jeeva Jaganathan indicated no relevant financial relationships.
Arnold Forlemu indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Madhavi Reddy indicated no relevant financial relationships.
Camelia Ciobanu, MD1, Manasa Ginjupalli, MD1, Amr Dokmak, MD1, Ali Wakil, MD1, Jeeva Jaganathan, MD2, Arnold Forlemu, MD1, Chaula Desai, MD1, Madhavi Reddy, MD2. P5946 - The Role of Ammonia Testing in Hepatic Encephalopathy: A Quality Improvement Project, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
