Tuesday Poster Session
Category: Liver
P5942 - External Validation of Machine Learning Models to Assess Portal Hypertension Severity in Patients With Compensated Chronic Liver Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FM
Fahad S. Mohammed, BS (he/him/his)
UNC School of Medicine
Chapel Hill, NC
Presenting Author(s)
Fahad Mohammed, BS, Minzhi Xing, PhD, Michael Mohnasky, BS, Andrew Caddell, BS, Jack Felkner, BS, Thomas Turner, BS, Arjun Juneja, BS, Nima Kokabi, MD, Hyeon Yu, MD, Chelsea Anderson, PhD, MPH, Andrew Moon, MD, MPH
UNC School of Medicine, Chapel Hill, NC
Introduction: Portal hypertension is a critical determinant of compensated advanced chronic liver disease (cACLD) progression. While multiple predictive models exist, external validation is necessary to ensure generalizability across populations. This study aims to externally validate two models that predict portal hypertension severity using laboratory and clinical parameters, with thresholds of hepatic venous pressure gradient (HVPG) ≥10 mmHg and ≥16 mmHg. Both models were developed using a European population, warranting the need for an external validation using a US cohort.
Methods: This study included a retrospective cohort of 152 patients with cACLD who underwent HVPG measurement at UNC Health from May 2014 to April 2024. Exclusion criteria were: 1. Current hepatic decompensation (ascites, variceal bleed, encephalopathy) 2. Current/prior hepatic malignancy 3. History of transjugular intrahepatic portosystemic shunt (TIPS). Two models were evaluated: a machine learning model (M1) which incorporates platelet count, bilirubin, and international normalized ratio (INR); and a Fib4+ Model (M2), which utilizes the Fib-4 score (age, AST, ALT, platelet count) and albumin. Model performance was assessed by calculating the area under the receiver operating characteristic curve (AUROC) for HVPG thresholds ≥10 mmHg and ≥16 mmHg. To further assess the model's robustness and generalizability, calibration plots and Brier scores were used to evaluate each model's predictive performance.
Results: M1 achieved an AUROC of 0.728 for predicting HVPG ≥10 mmHg and 0.745 for HVPG ≥16 mmHg, while M2 demonstrated AUROCs of 0.655 for predicting HVPG ≥10 mmHg and 0.721 for HVPG ≥16 mmHg. M1 demonstrated 10.0% and 3.2% higher predictive performance compared to M2 for HVPG ≥10 mmHg and HVPG ≥16 mmHg, respectively. Brier scores for predicting HVPG ≥10 mmHg were 0.101 and 0.117 (M1 vs. M2), while those for predicting HVPG ≥16 mmHg were 0.065 and 0.084 (M1 vs. M2). Both models showed good predictive accuracy across different subgroups.
Discussion: The external validation results indicate that both models exhibited good performance in predicting portal hypertension severity in patients with compensated chronic liver disease. Model M1 demonstrated better predictive performance for both HVPG thresholds. These models may serve as valuable tools for clinical decision-making and identifying patients at increased risk for adverse outcomes.
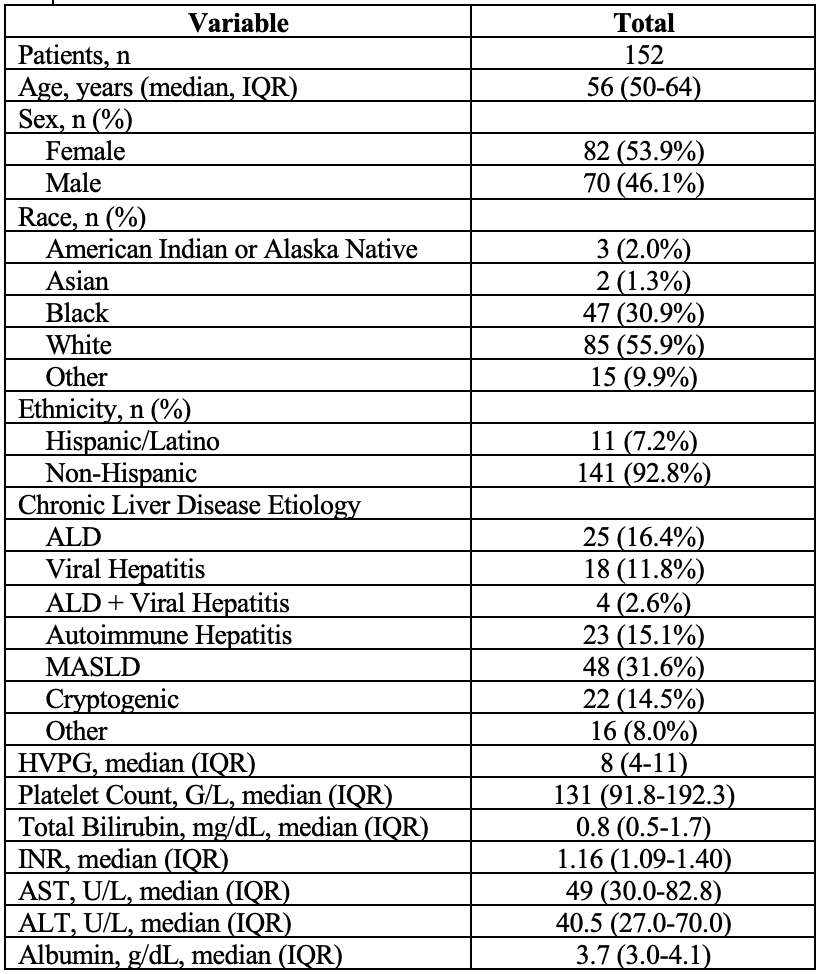
Figure: Patient Characteristics
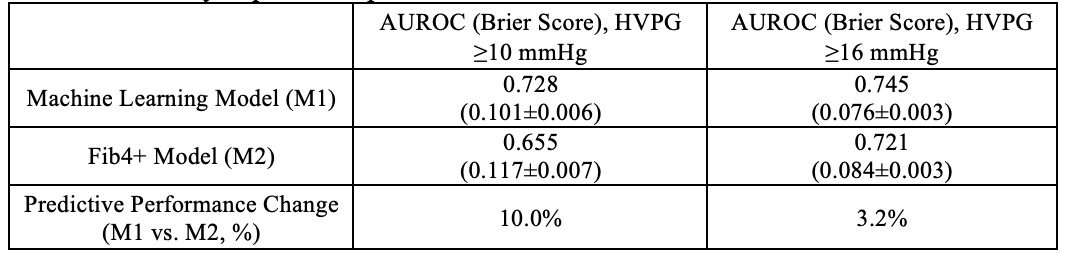
Figure: Summary of predictive performance for Models M1 vs. M2.
Disclosures:
Fahad Mohammed indicated no relevant financial relationships.
Minzhi Xing indicated no relevant financial relationships.
Michael Mohnasky indicated no relevant financial relationships.
Andrew Caddell indicated no relevant financial relationships.
Jack Felkner indicated no relevant financial relationships.
Thomas Turner indicated no relevant financial relationships.
Arjun Juneja indicated no relevant financial relationships.
Nima Kokabi indicated no relevant financial relationships.
Hyeon Yu indicated no relevant financial relationships.
Chelsea Anderson indicated no relevant financial relationships.
Andrew Moon indicated no relevant financial relationships.
Fahad Mohammed, BS, Minzhi Xing, PhD, Michael Mohnasky, BS, Andrew Caddell, BS, Jack Felkner, BS, Thomas Turner, BS, Arjun Juneja, BS, Nima Kokabi, MD, Hyeon Yu, MD, Chelsea Anderson, PhD, MPH, Andrew Moon, MD, MPH. P5942 - External Validation of Machine Learning Models to Assess Portal Hypertension Severity in Patients With Compensated Chronic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
UNC School of Medicine, Chapel Hill, NC
Introduction: Portal hypertension is a critical determinant of compensated advanced chronic liver disease (cACLD) progression. While multiple predictive models exist, external validation is necessary to ensure generalizability across populations. This study aims to externally validate two models that predict portal hypertension severity using laboratory and clinical parameters, with thresholds of hepatic venous pressure gradient (HVPG) ≥10 mmHg and ≥16 mmHg. Both models were developed using a European population, warranting the need for an external validation using a US cohort.
Methods: This study included a retrospective cohort of 152 patients with cACLD who underwent HVPG measurement at UNC Health from May 2014 to April 2024. Exclusion criteria were: 1. Current hepatic decompensation (ascites, variceal bleed, encephalopathy) 2. Current/prior hepatic malignancy 3. History of transjugular intrahepatic portosystemic shunt (TIPS). Two models were evaluated: a machine learning model (M1) which incorporates platelet count, bilirubin, and international normalized ratio (INR); and a Fib4+ Model (M2), which utilizes the Fib-4 score (age, AST, ALT, platelet count) and albumin. Model performance was assessed by calculating the area under the receiver operating characteristic curve (AUROC) for HVPG thresholds ≥10 mmHg and ≥16 mmHg. To further assess the model's robustness and generalizability, calibration plots and Brier scores were used to evaluate each model's predictive performance.
Results: M1 achieved an AUROC of 0.728 for predicting HVPG ≥10 mmHg and 0.745 for HVPG ≥16 mmHg, while M2 demonstrated AUROCs of 0.655 for predicting HVPG ≥10 mmHg and 0.721 for HVPG ≥16 mmHg. M1 demonstrated 10.0% and 3.2% higher predictive performance compared to M2 for HVPG ≥10 mmHg and HVPG ≥16 mmHg, respectively. Brier scores for predicting HVPG ≥10 mmHg were 0.101 and 0.117 (M1 vs. M2), while those for predicting HVPG ≥16 mmHg were 0.065 and 0.084 (M1 vs. M2). Both models showed good predictive accuracy across different subgroups.
Discussion: The external validation results indicate that both models exhibited good performance in predicting portal hypertension severity in patients with compensated chronic liver disease. Model M1 demonstrated better predictive performance for both HVPG thresholds. These models may serve as valuable tools for clinical decision-making and identifying patients at increased risk for adverse outcomes.
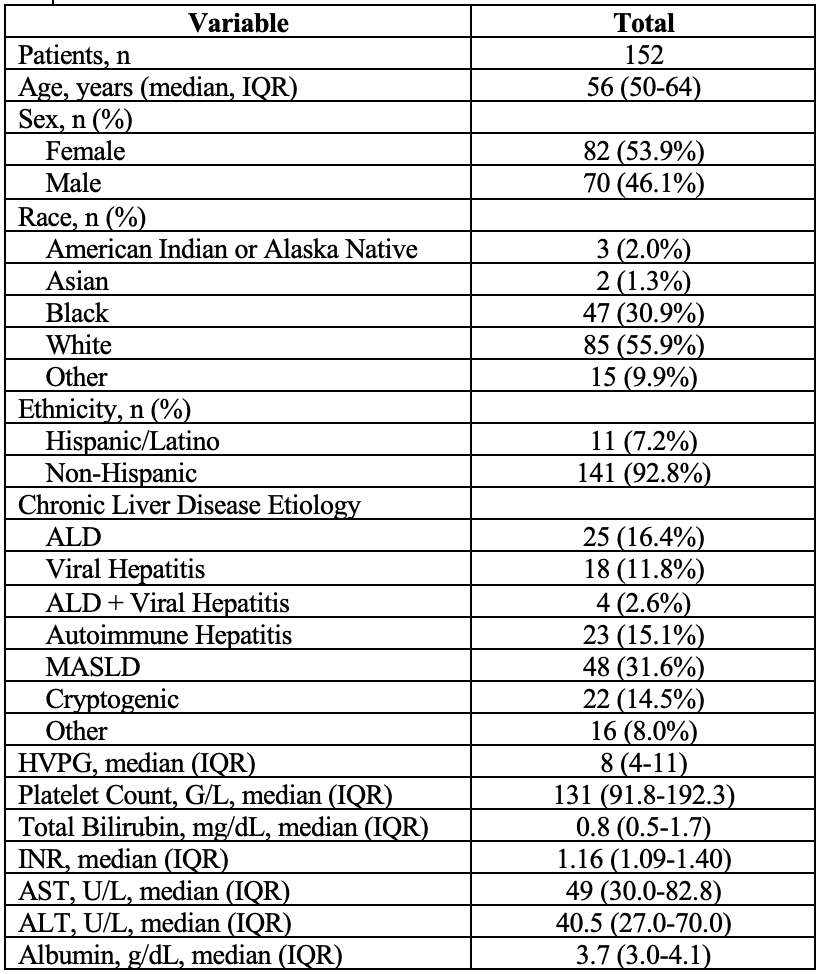
Figure: Patient Characteristics
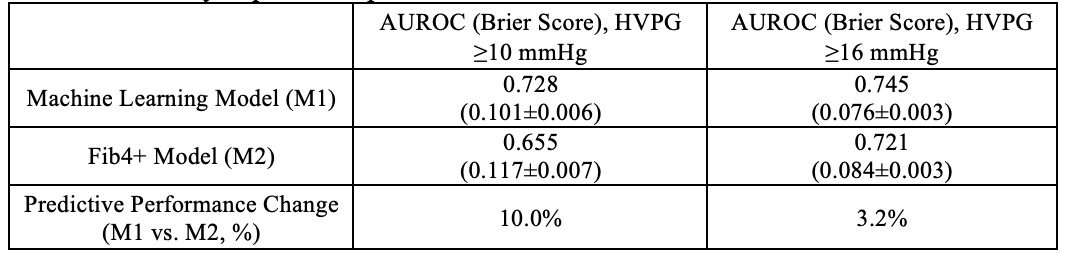
Figure: Summary of predictive performance for Models M1 vs. M2.
Disclosures:
Fahad Mohammed indicated no relevant financial relationships.
Minzhi Xing indicated no relevant financial relationships.
Michael Mohnasky indicated no relevant financial relationships.
Andrew Caddell indicated no relevant financial relationships.
Jack Felkner indicated no relevant financial relationships.
Thomas Turner indicated no relevant financial relationships.
Arjun Juneja indicated no relevant financial relationships.
Nima Kokabi indicated no relevant financial relationships.
Hyeon Yu indicated no relevant financial relationships.
Chelsea Anderson indicated no relevant financial relationships.
Andrew Moon indicated no relevant financial relationships.
Fahad Mohammed, BS, Minzhi Xing, PhD, Michael Mohnasky, BS, Andrew Caddell, BS, Jack Felkner, BS, Thomas Turner, BS, Arjun Juneja, BS, Nima Kokabi, MD, Hyeon Yu, MD, Chelsea Anderson, PhD, MPH, Andrew Moon, MD, MPH. P5942 - External Validation of Machine Learning Models to Assess Portal Hypertension Severity in Patients With Compensated Chronic Liver Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
