Tuesday Poster Session
Category: Liver
P5935 - Sweet Burden: Comparing Dietary Sugar Intake in Metabolic vs Alcoholic Fatty Liver Disease by Demographics
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammed Dheyaa Marsool
Mayo Clinic
Phoenix, AZ
Presenting Author(s)
Ali Dheyaa Marsool, 1, Mohammed Dheyaa Marsool, 2, Thai Hau Koo, MD3, Muhammad Abdul Rehman, MBBS4, Xue Leong, 3, Adrian Lindsey, MD5, Sara Shihab, MD2
1Al-Kindy College of Medicine, Baghdad, Baghdad, Iraq; 2Mayo Clinic, Phoenix, AZ; 3University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 4Mayo Clinic, Byron, MN; 5MetroHealth Medical Center, Cleveland, OH
Introduction: Dietary composition is a key modifiable factor in the progression of liver disease. However, few studies have directly compared the nutritional patterns of alcoholic liver disease (ALD) and metabolic-associated fatty liver disease (MAFLD). This study investigated how dietary quality and nutrient intake differ between individuals with presumed ALD and MAFLD, and whether these differences vary by sex and race/ethnicity.
Methods: We analyzed data from 9,254 adults in the 2017–2018 National Health and Nutrition Examination Survey (NHANES) with complete data on liver enzymes, alcohol use, dietary intake, and demographics. MAFLD was defined based on elevated liver enzyme levels in the absence of heavy alcohol use, whereas ALD was identified among heavy drinkers. Dietary intake was assessed using 24-hour recalls and included total sugar, fat, protein, and caloric intake. Survey-weighted multivariate regressions adjusted for BMI, sex, race/ethnicity, and calorie intake were used to examine the associations between MAFLD and nutrient consumption.
Results: Adults with MAFLD had a significantly higher mean BMI than those without MAFLD (31.15 vs. 29.12 kg/m², p = 0.005). Although calorie intake was marginally higher in the MAFLD group (2,295 vs. 2,171 kcal/day), this difference was not statistically significant (p = 0.27). Sugar intake showed a non-significant trend toward elevation in the MAFLD group (mean 89.76 vs. 85.34 g/day, p = 0.11). In multivariate models, MAFLD was associated with 17 g/day higher sugar intake, although this did not reach statistical significance (p = 0.11). Female sex and Non-Hispanic Black race were significantly associated with greater sugar consumption (p < 0.001 and p = 0.015, respectively), whereas higher BMI was inversely related to sugar intake (p = 0.055). Total caloric intake was the strongest predictor of sugar consumption (p < 0.001). Visualization supported a trend toward higher sugar intake in MAFLD than in ALD.
Discussion: In this nationally representative sample, individuals with MAFLD tended to consume more sugar than those with ALD or no fatty liver disease, although the differences were not statistically significant. Sex and racial/ethnic disparities in sugar consumption were evident, with implications for personalized dietary counseling. These findings underscore the need for targeted nutritional interventions for metabolic liver disease, particularly among women and minority populations.
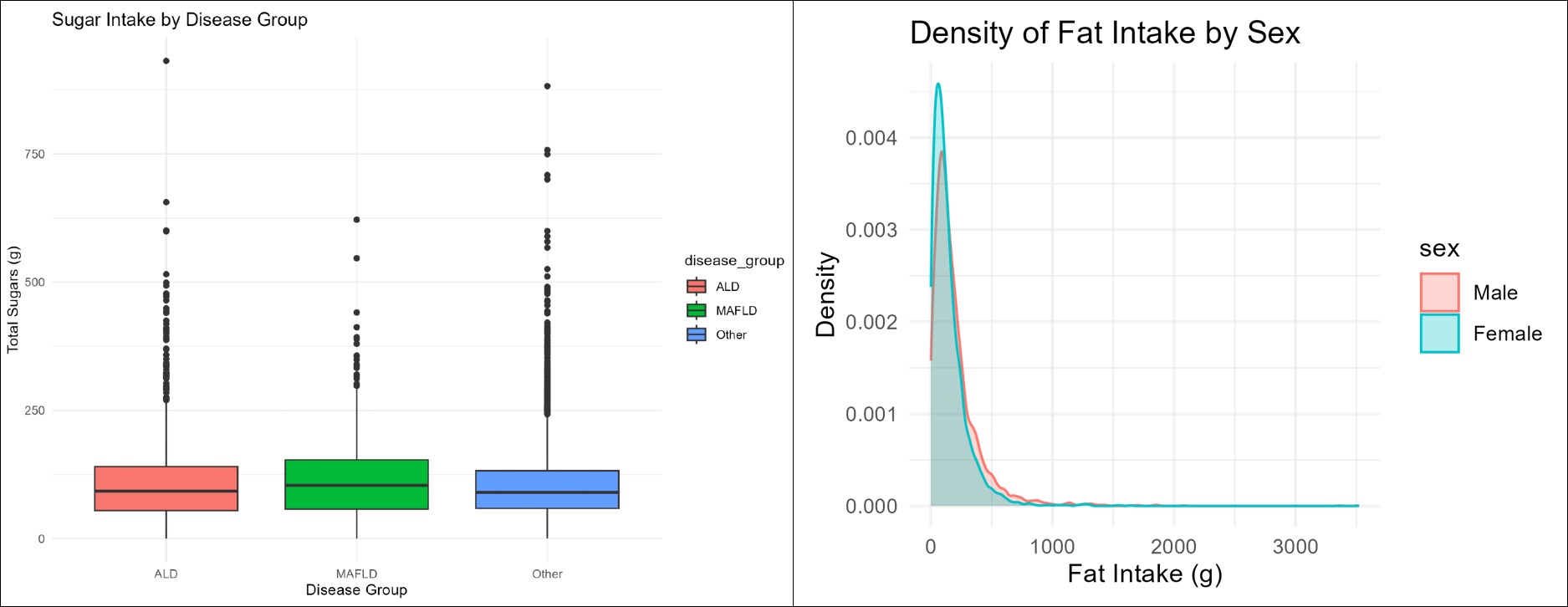
Figure: Left: Boxplots of total sugar intake by disease group highlights generally higher median sugar consumption among those with MAFLD compared to ALD and other participants. Right: Density distribution of fat intake by sex demonstrates that females have slightly higher fat consumption density than males.
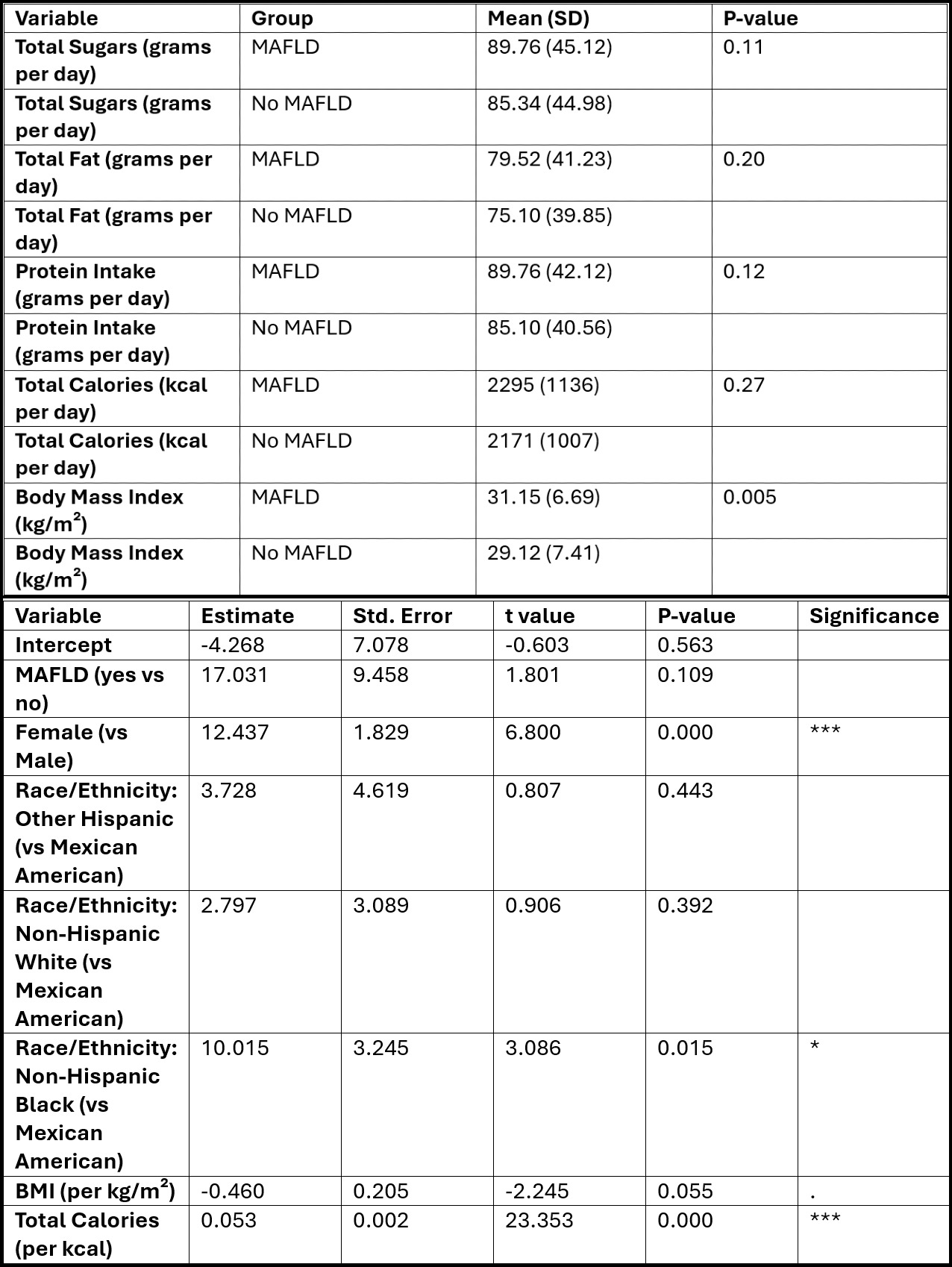
Figure: Top: Descriptive characteristics and dietary intake by MAFLD status in NHANES 2017-2018. Bottom: Survey-weighted linear regression of sugar intake predicted by MAFLD status and covariates.
Disclosures:
Ali Dheyaa Marsool indicated no relevant financial relationships.
Mohammed Dheyaa Marsool indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Muhammad Abdul Rehman indicated no relevant financial relationships.
Xue Leong indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Sara Shihab indicated no relevant financial relationships.
Ali Dheyaa Marsool, 1, Mohammed Dheyaa Marsool, 2, Thai Hau Koo, MD3, Muhammad Abdul Rehman, MBBS4, Xue Leong, 3, Adrian Lindsey, MD5, Sara Shihab, MD2. P5935 - Sweet Burden: Comparing Dietary Sugar Intake in Metabolic vs Alcoholic Fatty Liver Disease by Demographics, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Al-Kindy College of Medicine, Baghdad, Baghdad, Iraq; 2Mayo Clinic, Phoenix, AZ; 3University of Sciences Malaysia Specialist Hospital, Kelantan, Kelantan, Malaysia; 4Mayo Clinic, Byron, MN; 5MetroHealth Medical Center, Cleveland, OH
Introduction: Dietary composition is a key modifiable factor in the progression of liver disease. However, few studies have directly compared the nutritional patterns of alcoholic liver disease (ALD) and metabolic-associated fatty liver disease (MAFLD). This study investigated how dietary quality and nutrient intake differ between individuals with presumed ALD and MAFLD, and whether these differences vary by sex and race/ethnicity.
Methods: We analyzed data from 9,254 adults in the 2017–2018 National Health and Nutrition Examination Survey (NHANES) with complete data on liver enzymes, alcohol use, dietary intake, and demographics. MAFLD was defined based on elevated liver enzyme levels in the absence of heavy alcohol use, whereas ALD was identified among heavy drinkers. Dietary intake was assessed using 24-hour recalls and included total sugar, fat, protein, and caloric intake. Survey-weighted multivariate regressions adjusted for BMI, sex, race/ethnicity, and calorie intake were used to examine the associations between MAFLD and nutrient consumption.
Results: Adults with MAFLD had a significantly higher mean BMI than those without MAFLD (31.15 vs. 29.12 kg/m², p = 0.005). Although calorie intake was marginally higher in the MAFLD group (2,295 vs. 2,171 kcal/day), this difference was not statistically significant (p = 0.27). Sugar intake showed a non-significant trend toward elevation in the MAFLD group (mean 89.76 vs. 85.34 g/day, p = 0.11). In multivariate models, MAFLD was associated with 17 g/day higher sugar intake, although this did not reach statistical significance (p = 0.11). Female sex and Non-Hispanic Black race were significantly associated with greater sugar consumption (p < 0.001 and p = 0.015, respectively), whereas higher BMI was inversely related to sugar intake (p = 0.055). Total caloric intake was the strongest predictor of sugar consumption (p < 0.001). Visualization supported a trend toward higher sugar intake in MAFLD than in ALD.
Discussion: In this nationally representative sample, individuals with MAFLD tended to consume more sugar than those with ALD or no fatty liver disease, although the differences were not statistically significant. Sex and racial/ethnic disparities in sugar consumption were evident, with implications for personalized dietary counseling. These findings underscore the need for targeted nutritional interventions for metabolic liver disease, particularly among women and minority populations.
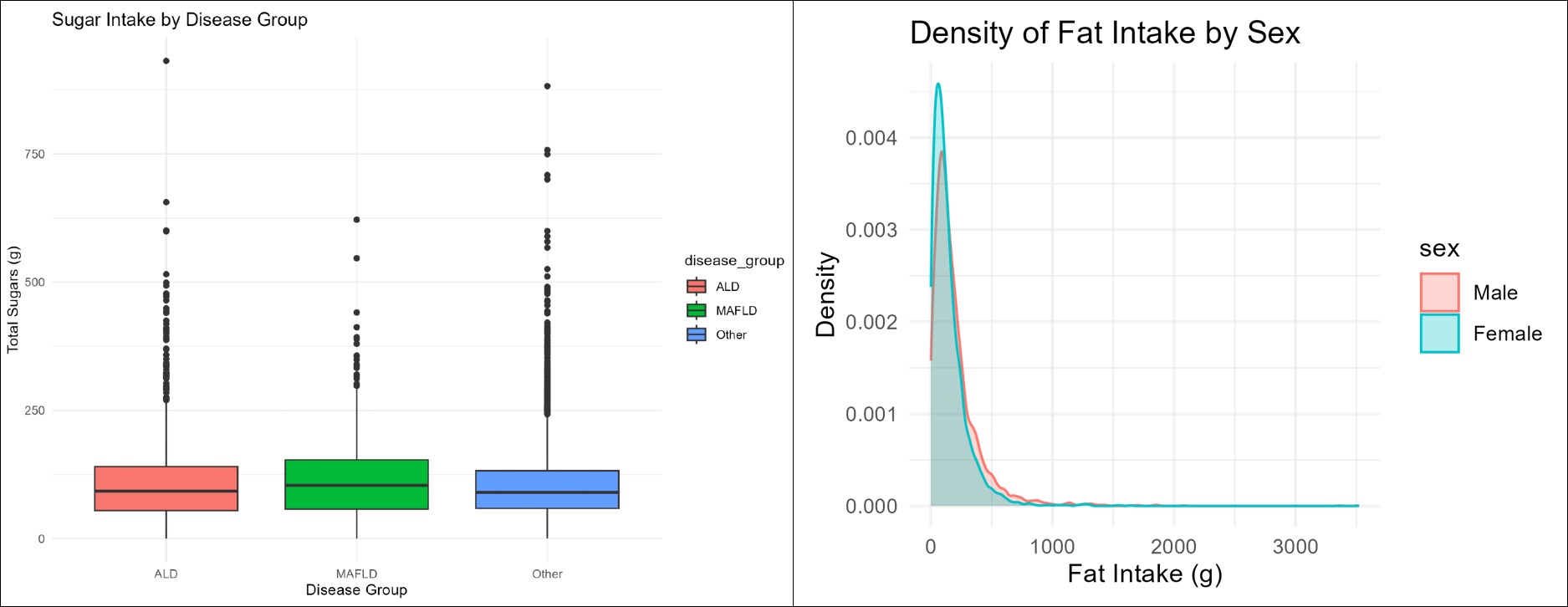
Figure: Left: Boxplots of total sugar intake by disease group highlights generally higher median sugar consumption among those with MAFLD compared to ALD and other participants. Right: Density distribution of fat intake by sex demonstrates that females have slightly higher fat consumption density than males.
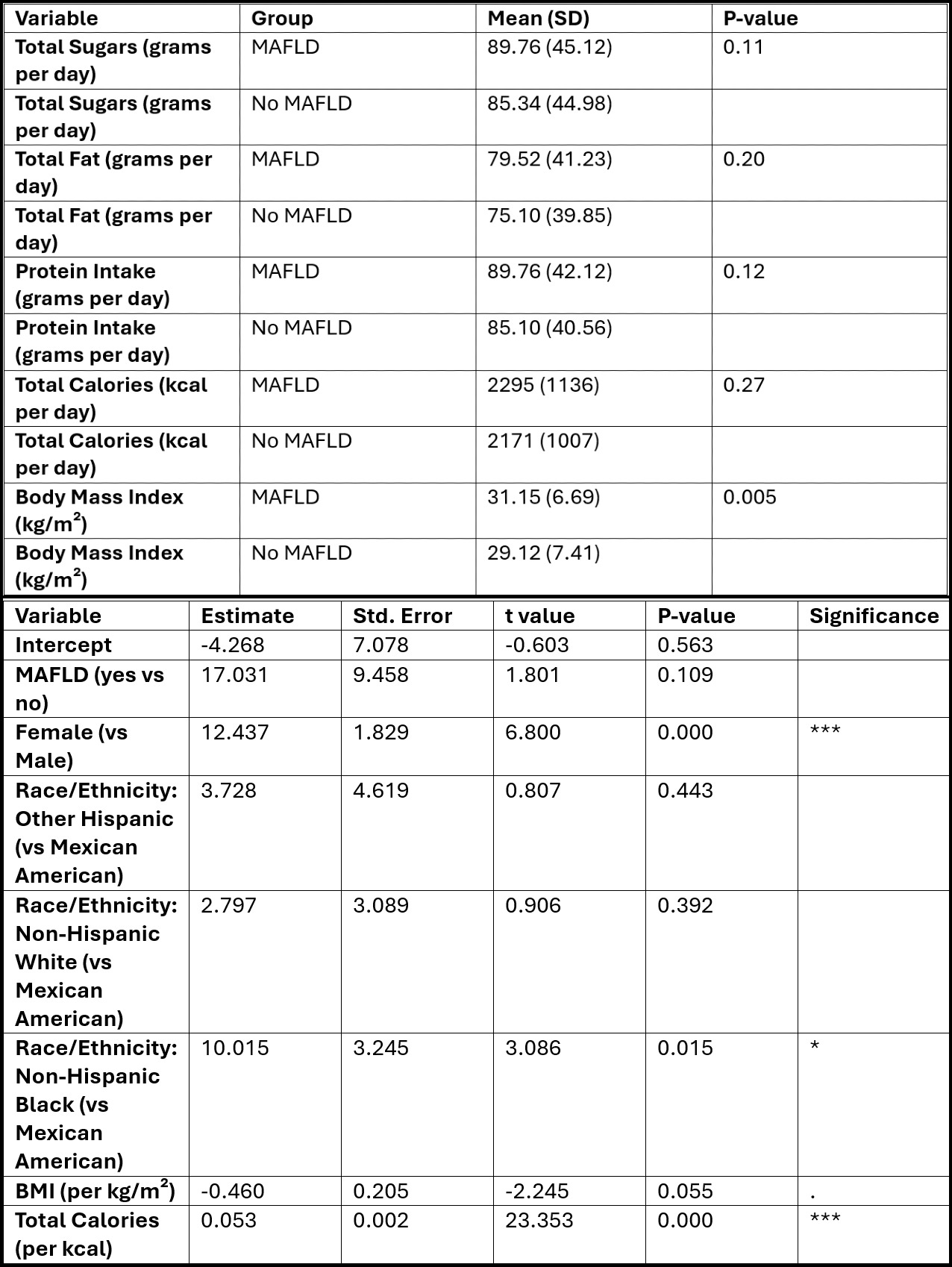
Figure: Top: Descriptive characteristics and dietary intake by MAFLD status in NHANES 2017-2018. Bottom: Survey-weighted linear regression of sugar intake predicted by MAFLD status and covariates.
Disclosures:
Ali Dheyaa Marsool indicated no relevant financial relationships.
Mohammed Dheyaa Marsool indicated no relevant financial relationships.
Thai Hau Koo indicated no relevant financial relationships.
Muhammad Abdul Rehman indicated no relevant financial relationships.
Xue Leong indicated no relevant financial relationships.
Adrian Lindsey indicated no relevant financial relationships.
Sara Shihab indicated no relevant financial relationships.
Ali Dheyaa Marsool, 1, Mohammed Dheyaa Marsool, 2, Thai Hau Koo, MD3, Muhammad Abdul Rehman, MBBS4, Xue Leong, 3, Adrian Lindsey, MD5, Sara Shihab, MD2. P5935 - Sweet Burden: Comparing Dietary Sugar Intake in Metabolic vs Alcoholic Fatty Liver Disease by Demographics, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
