Tuesday Poster Session
Category: Liver
P5970 - Caught in the Hepatic Web: Weaving Through a Tangled Tale
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

William Jones, MD
Prisma Health Greenville Memorial Hospital, SC
Presenting Author(s)
William Jones, MD, Emma Smith, MD, Anjani Jammula, MD, Chauncy Handran, MD
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Budd-Chiari syndrome (BCS) is characterized by hepatic venous outflow obstruction at the level of hepatic veins or IVC leading to portal HTN. Congenital or acquired membranous webs within the hepatic veins can present as chronic BCS, are challenging to diagnose and complicate intravascular hepatic procedures.
Case Description/
Methods: 27-year-old obese, Hispanic male presents with a history of EV and ascites who carried a diagnosis of portal HTN and decompensated cirrhosis, but with a low MELD of 11. His initial presentation was hematemesis related to variceal hemorrhage requiring EVL 4 years ago at another facility. All serological testing for genetic, infectious, metabolic etiologies of cirrhosis were unrevealing. History negative for heavy alcohol use. Cardiac causes, hypercoagulable states, and veno-occlusive disease were all ruled out. A percutaneous liver biopsy at his initial diagnosis showed congestive hepatopathy with bridging fibrosis, but no cirrhosis, hepatitis, or steatosis. He had ongoing decompensation with refractory ascites requiring frequent large volume paracenteses, SBP, HE, and recurrent variceal hemorrhage needing multiple rounds of EVL. Given the discrepancy in his clinical deterioration and the prior minimal liver biopsy findings, a repeat transjugular liver biopsy was performed where the hepatic veins were unable to be cannulated, and intrahepatic IVC was noted to be markedly narrowed. Pathology again revealed bridging fibrosis without cirrhosis, sinusoidal dilation, and < 5% steatosis, consistent with venous outflow obstruction. He ultimately required TIPS for refractory ascites, and a traditional TIPS insertion was unsuccessful deemed likely to be related to the hepatic venous webs. Ultrasound was used to gain percutaneous access to the right hepatic vein. A wire was advanced via transjugular access and snared via the percutaneous access. This area was dilated and allowed hepatic vein access for portal vein cannulation. Hepatic venous portal gradient decreased from 26 mmHg to 9mmHg after TIPS. His diuretics have since been discontinued, varices were absent on subsequent endoscopies, and encephalopathy well managed on Lactulose.
Discussion: BCS is rare with an incidence below 1 case per million-person years, and non-thrombotic causes being even more uncommon. Not only did this case of intrahepatic venous webs in a young male presenting as decompensated cirrhosis with no identifiable etiology provide for a challenging diagnosis but also a complicated TIPS.
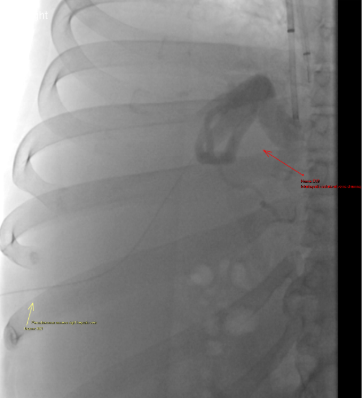
Figure: Percuatenous access into right hepatic vein (yellow arrow). Venogram with intrahepatic venous collaterals draining directly to IVC (red arrow).

Figure: Direct ‘Gun-site” access and snaring into right hepatic vein across the hepatic venous web for access into the right hepatic vein from the native right hepatic vein origin.
Disclosures:
William Jones indicated no relevant financial relationships.
Emma Smith indicated no relevant financial relationships.
Anjani Jammula indicated no relevant financial relationships.
Chauncy Handran indicated no relevant financial relationships.
William Jones, MD, Emma Smith, MD, Anjani Jammula, MD, Chauncy Handran, MD. P5970 - Caught in the Hepatic Web: Weaving Through a Tangled Tale, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Prisma Health Greenville Memorial Hospital, Greenville, SC
Introduction: Budd-Chiari syndrome (BCS) is characterized by hepatic venous outflow obstruction at the level of hepatic veins or IVC leading to portal HTN. Congenital or acquired membranous webs within the hepatic veins can present as chronic BCS, are challenging to diagnose and complicate intravascular hepatic procedures.
Case Description/
Methods: 27-year-old obese, Hispanic male presents with a history of EV and ascites who carried a diagnosis of portal HTN and decompensated cirrhosis, but with a low MELD of 11. His initial presentation was hematemesis related to variceal hemorrhage requiring EVL 4 years ago at another facility. All serological testing for genetic, infectious, metabolic etiologies of cirrhosis were unrevealing. History negative for heavy alcohol use. Cardiac causes, hypercoagulable states, and veno-occlusive disease were all ruled out. A percutaneous liver biopsy at his initial diagnosis showed congestive hepatopathy with bridging fibrosis, but no cirrhosis, hepatitis, or steatosis. He had ongoing decompensation with refractory ascites requiring frequent large volume paracenteses, SBP, HE, and recurrent variceal hemorrhage needing multiple rounds of EVL. Given the discrepancy in his clinical deterioration and the prior minimal liver biopsy findings, a repeat transjugular liver biopsy was performed where the hepatic veins were unable to be cannulated, and intrahepatic IVC was noted to be markedly narrowed. Pathology again revealed bridging fibrosis without cirrhosis, sinusoidal dilation, and < 5% steatosis, consistent with venous outflow obstruction. He ultimately required TIPS for refractory ascites, and a traditional TIPS insertion was unsuccessful deemed likely to be related to the hepatic venous webs. Ultrasound was used to gain percutaneous access to the right hepatic vein. A wire was advanced via transjugular access and snared via the percutaneous access. This area was dilated and allowed hepatic vein access for portal vein cannulation. Hepatic venous portal gradient decreased from 26 mmHg to 9mmHg after TIPS. His diuretics have since been discontinued, varices were absent on subsequent endoscopies, and encephalopathy well managed on Lactulose.
Discussion: BCS is rare with an incidence below 1 case per million-person years, and non-thrombotic causes being even more uncommon. Not only did this case of intrahepatic venous webs in a young male presenting as decompensated cirrhosis with no identifiable etiology provide for a challenging diagnosis but also a complicated TIPS.
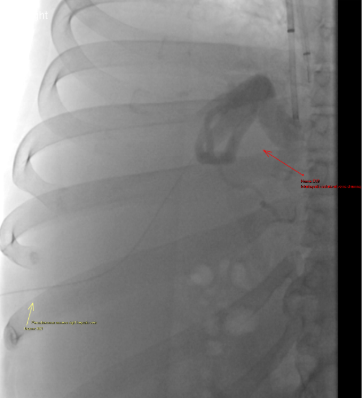
Figure: Percuatenous access into right hepatic vein (yellow arrow). Venogram with intrahepatic venous collaterals draining directly to IVC (red arrow).

Figure: Direct ‘Gun-site” access and snaring into right hepatic vein across the hepatic venous web for access into the right hepatic vein from the native right hepatic vein origin.
Disclosures:
William Jones indicated no relevant financial relationships.
Emma Smith indicated no relevant financial relationships.
Anjani Jammula indicated no relevant financial relationships.
Chauncy Handran indicated no relevant financial relationships.
William Jones, MD, Emma Smith, MD, Anjani Jammula, MD, Chauncy Handran, MD. P5970 - Caught in the Hepatic Web: Weaving Through a Tangled Tale, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

