Tuesday Poster Session
Category: Liver
P5958 - Sociodemographic Disparities in Liver Fibrosis and Steatosis in US Adults
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Razan Aburumman, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Razan Aburumman, MD1, Sarine Tahmazian, MD1, Saif Nabeel, MD2, Saqr Alsakarneh, MD, MSc3, Tala Al Saleh, MD1, Syed-Mohammed Jafri, MD1
1Henry Ford Health, Detroit, MI; 2School of Medicine, The University of Jordan, Amman, 'Amman, Jordan; 3Mayo Clinic, Rochester, MN
Introduction: Liver stiffness and steatosis, assessed via transient elastography, are non-invasive markers used to evaluate hepatic fibrosis and fat accumulation. This study aims to examine differences in liver stiffness and steatosis across sociodemographic groups.
Methods: Data were drawn from the NHANES 2017–2020 cycles, a nationally representative survey of the U.S. population conducted by the Centers for Disease Control and Prevention. Participants aged 18 and older who underwent transient elastography using FibroScan were included. Liver stiffness measurements (LSM, kPa) and controlled attenuation parameters (CAP, dB/m) were used as indicators of fibrosis and steatosis, respectively. Statistical analyses included Pearson correlation for continuous variables and ANOVA tests with post hoc Tukey HSD for group comparisons.
Results: A total of 8,317 participants were included (50.3% female, 34.2% non-Hispanic white, and the mean age was 49 years). Males had higher median liver stiffness (6.45 kPa) and CAP (270.99 dB/m) than females (5.58 kPa and 256.56 dB/m, respectively), with both differences statistically significant (P < 0.001). Age was significantly associated with liver stiffness (r = 0.079, P < 0.001) and CAP (r = 0.183, P < 0.001). Post hoc HSD tests showed that non-Hispanic Asians had significantly lower mean liver stiffness compared to other racial groups (P < 0.05), except for Mexican Americans. Additionally, Mexican Americans had significantly higher steatosis scores (280.21 dB/m) than all other racial groups (P < 0.05).
Participants with health insurance had slightly higher median liver stiffness compared to those without insurance (6.06 vs. 5.79 kPa, P = 0.049). Although median CAP values were also higher among insured individuals (264.25 vs. 261.08 dB/m), the difference was not statistically significant (P = 0.09). Post hoc HSD tests showed that participants with full food security had significantly lower liver stiffness than those with very low food security (5.89 vs. 6.46 kPa, P = 0.037), with no significant differences between other food security levels. Steatosis scores did not differ significantly across food security groups (P = 0.098). The family monthly poverty index was not significantly associated with liver stiffness (r = –0.022, P = 0.07) or CAP scores (r = 0.003, P = 0.787).
Discussion: Liver stiffness and steatosis differed by gender, race, and food security status. These findings suggest sociodemographic factors may influence liver health outcomes in U.S. adults.
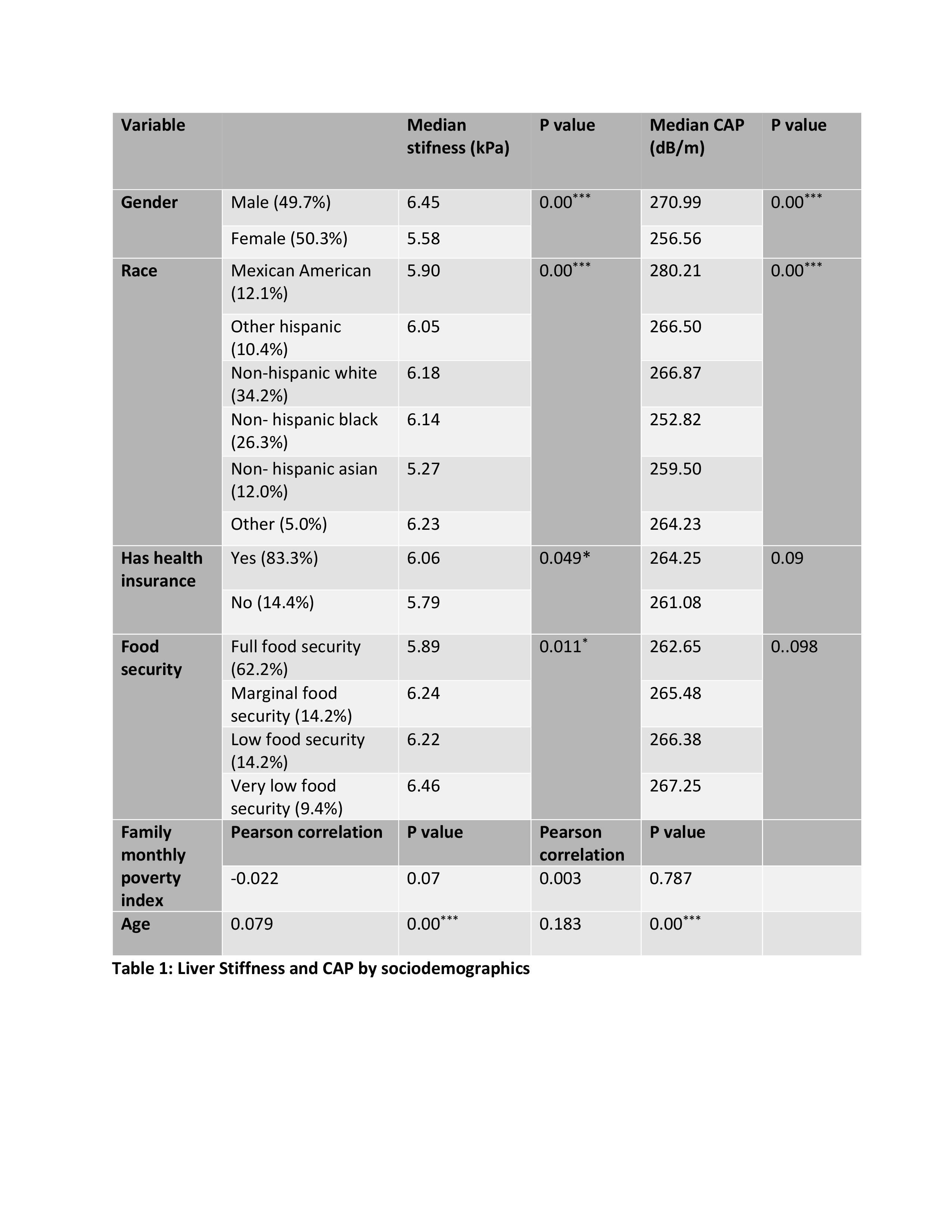
Figure: Table 1: Liver Stiffness and CAP by sociodemographics
Disclosures:
Razan Aburumman indicated no relevant financial relationships.
Sarine Tahmazian indicated no relevant financial relationships.
Saif Nabeel indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Tala Al Saleh indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Razan Aburumman, MD1, Sarine Tahmazian, MD1, Saif Nabeel, MD2, Saqr Alsakarneh, MD, MSc3, Tala Al Saleh, MD1, Syed-Mohammed Jafri, MD1. P5958 - Sociodemographic Disparities in Liver Fibrosis and Steatosis in US Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Health, Detroit, MI; 2School of Medicine, The University of Jordan, Amman, 'Amman, Jordan; 3Mayo Clinic, Rochester, MN
Introduction: Liver stiffness and steatosis, assessed via transient elastography, are non-invasive markers used to evaluate hepatic fibrosis and fat accumulation. This study aims to examine differences in liver stiffness and steatosis across sociodemographic groups.
Methods: Data were drawn from the NHANES 2017–2020 cycles, a nationally representative survey of the U.S. population conducted by the Centers for Disease Control and Prevention. Participants aged 18 and older who underwent transient elastography using FibroScan were included. Liver stiffness measurements (LSM, kPa) and controlled attenuation parameters (CAP, dB/m) were used as indicators of fibrosis and steatosis, respectively. Statistical analyses included Pearson correlation for continuous variables and ANOVA tests with post hoc Tukey HSD for group comparisons.
Results: A total of 8,317 participants were included (50.3% female, 34.2% non-Hispanic white, and the mean age was 49 years). Males had higher median liver stiffness (6.45 kPa) and CAP (270.99 dB/m) than females (5.58 kPa and 256.56 dB/m, respectively), with both differences statistically significant (P < 0.001). Age was significantly associated with liver stiffness (r = 0.079, P < 0.001) and CAP (r = 0.183, P < 0.001). Post hoc HSD tests showed that non-Hispanic Asians had significantly lower mean liver stiffness compared to other racial groups (P < 0.05), except for Mexican Americans. Additionally, Mexican Americans had significantly higher steatosis scores (280.21 dB/m) than all other racial groups (P < 0.05).
Participants with health insurance had slightly higher median liver stiffness compared to those without insurance (6.06 vs. 5.79 kPa, P = 0.049). Although median CAP values were also higher among insured individuals (264.25 vs. 261.08 dB/m), the difference was not statistically significant (P = 0.09). Post hoc HSD tests showed that participants with full food security had significantly lower liver stiffness than those with very low food security (5.89 vs. 6.46 kPa, P = 0.037), with no significant differences between other food security levels. Steatosis scores did not differ significantly across food security groups (P = 0.098). The family monthly poverty index was not significantly associated with liver stiffness (r = –0.022, P = 0.07) or CAP scores (r = 0.003, P = 0.787).
Discussion: Liver stiffness and steatosis differed by gender, race, and food security status. These findings suggest sociodemographic factors may influence liver health outcomes in U.S. adults.
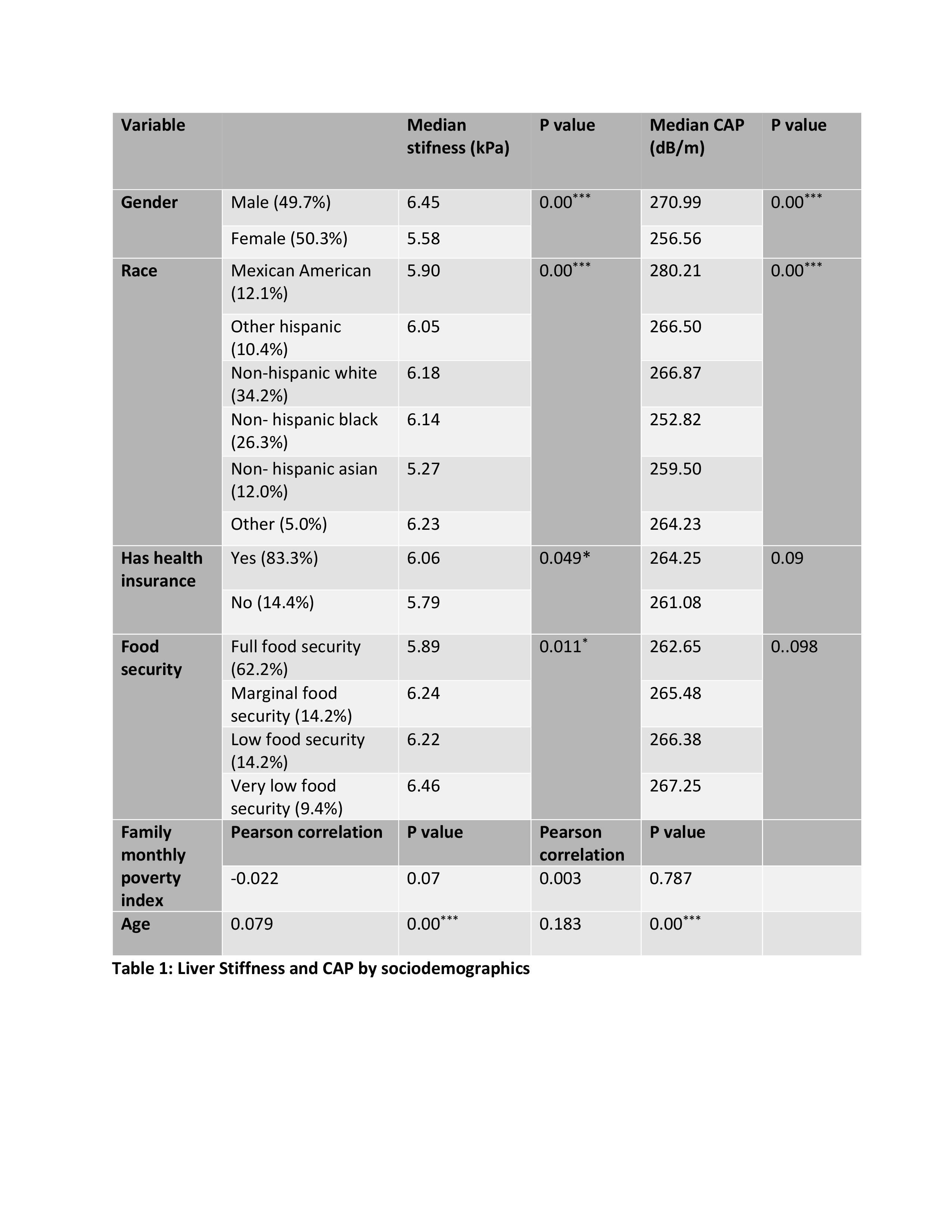
Figure: Table 1: Liver Stiffness and CAP by sociodemographics
Disclosures:
Razan Aburumman indicated no relevant financial relationships.
Sarine Tahmazian indicated no relevant financial relationships.
Saif Nabeel indicated no relevant financial relationships.
Saqr Alsakarneh indicated no relevant financial relationships.
Tala Al Saleh indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Razan Aburumman, MD1, Sarine Tahmazian, MD1, Saif Nabeel, MD2, Saqr Alsakarneh, MD, MSc3, Tala Al Saleh, MD1, Syed-Mohammed Jafri, MD1. P5958 - Sociodemographic Disparities in Liver Fibrosis and Steatosis in US Adults, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
