Tuesday Poster Session
Category: Liver
P5931 - Racial Differences in Clinical Outcomes Among Cirrhotic Patients on SGLT2 Inhibitors: A Propensity-Matched Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohamad Mahdi Osman, DO
Cleveland Clinic
Cleveland, OH
Presenting Author(s)
Mohamad Mahdi Osman, DO1, Mohamad-Noor Abu-Hammour, MD1, Varun Aitharaju, MD2, Leandro Sierra, MD3, Omar Sims, PhD4, Ali Syed, MD5, Dian Jung Chiang, MD1
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Hoover, AL; 5University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Sodium-glucose co-transporter 2 inhibitors (SGLT2-i) have demonstrated cardio-renal benefits in patients with type 2 diabetes mellitus and are increasingly prescribed in populations with advanced liver disease. However, recent data from meta-analysis of clinical trials suggest clinical outcome discrepancy between black and white patients. The real-world clinical outcomes of SGLT2-i across racial groups—particularly among patients with cirrhosis—remains to be determined This study aimed to compare clinical outcomes between Black and White patients with cirrhosis on SGLT2-i in a large research database.
Methods: Using the TriNetX research network, we identified adult Black and White patients with cirrhosis who were prescribed SGLT2-i. A total of 6,255 Black and 33,215 White patients were identified. After 1:1 propensity score matching based on demographics, liver function, MELD components, and cardiometabolic comorbidities, 6,238 matched pairs were analyzed. Outcomes were assessed over a three-year follow-up period using time-to-event analysis. The primary outcome was all-cause mortality. Secondary outcomes included all-cause hospitalizations, ascites, spontaneous bacterial peritonitis (SBP), hepatic encephalopathy (HE), and variceal bleeding.
Results: Compared to White patients, Black patients with cirrhosis on SGLT2-i experienced significantly lower rates of all-cause mortality (11.9% vs. 15.8%; p < 0.001) and all-cause hospitalizations (43.0% vs. 46.4%; p < 0.001). Rates of ascites (14.5% vs. 19.3%; p < 0.001), SBP (0.9% vs. 1.5%; p = 0.005), HE (3.4% vs. 6.5%; p < 0.001), and variceal bleeding (0.6% vs. 1.2%; p < 0.001) were also significantly lower among Black patients (Table 1). These findings persisted despite matching for relevant clinical and biochemical covariates.
Discussion: In this large real-world analysis of patients with cirrhosis on SGLT2-i, Black patients demonstrated significantly better outcomes compared to White patients across all measured domains, including mortality, hospitalizations, and decompensated cirrhosis events. In contrast to meta-analysis of clinical trial data, the findings from large real world retrospective studies indicate SGLT2-i is associated with improved liver related outcomes. The discrepancy underscores the need for further investigation into genetic, socioeconomic, and access-related factors contributing to these disparities.
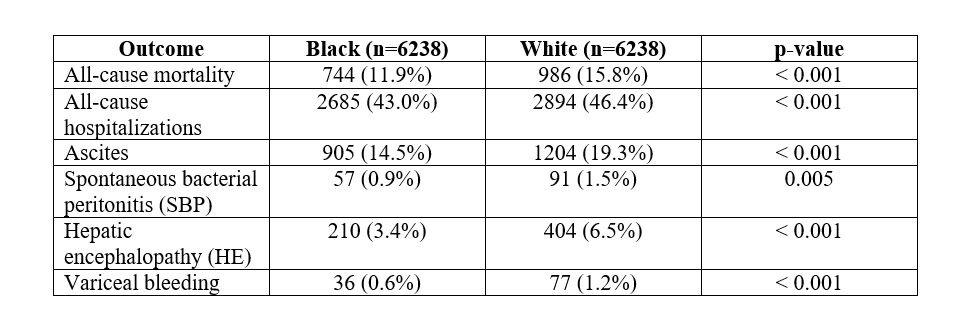
Figure: Table 1
Disclosures:
Mohamad Mahdi Osman indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Varun Aitharaju indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Ali Syed indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Mohamad Mahdi Osman, DO1, Mohamad-Noor Abu-Hammour, MD1, Varun Aitharaju, MD2, Leandro Sierra, MD3, Omar Sims, PhD4, Ali Syed, MD5, Dian Jung Chiang, MD1. P5931 - Racial Differences in Clinical Outcomes Among Cirrhotic Patients on SGLT2 Inhibitors: A Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Cleveland Clinic, Cleveland, OH; 2Cleveland Clinic Foundation, Cleveland, OH; 3Department of Internal Medicine, Cleveland Clinic, Cleveland, OH; 4Cleveland Clinic Foundation, Hoover, AL; 5University Hospitals Cleveland Medical Center, Cleveland, OH
Introduction: Sodium-glucose co-transporter 2 inhibitors (SGLT2-i) have demonstrated cardio-renal benefits in patients with type 2 diabetes mellitus and are increasingly prescribed in populations with advanced liver disease. However, recent data from meta-analysis of clinical trials suggest clinical outcome discrepancy between black and white patients. The real-world clinical outcomes of SGLT2-i across racial groups—particularly among patients with cirrhosis—remains to be determined This study aimed to compare clinical outcomes between Black and White patients with cirrhosis on SGLT2-i in a large research database.
Methods: Using the TriNetX research network, we identified adult Black and White patients with cirrhosis who were prescribed SGLT2-i. A total of 6,255 Black and 33,215 White patients were identified. After 1:1 propensity score matching based on demographics, liver function, MELD components, and cardiometabolic comorbidities, 6,238 matched pairs were analyzed. Outcomes were assessed over a three-year follow-up period using time-to-event analysis. The primary outcome was all-cause mortality. Secondary outcomes included all-cause hospitalizations, ascites, spontaneous bacterial peritonitis (SBP), hepatic encephalopathy (HE), and variceal bleeding.
Results: Compared to White patients, Black patients with cirrhosis on SGLT2-i experienced significantly lower rates of all-cause mortality (11.9% vs. 15.8%; p < 0.001) and all-cause hospitalizations (43.0% vs. 46.4%; p < 0.001). Rates of ascites (14.5% vs. 19.3%; p < 0.001), SBP (0.9% vs. 1.5%; p = 0.005), HE (3.4% vs. 6.5%; p < 0.001), and variceal bleeding (0.6% vs. 1.2%; p < 0.001) were also significantly lower among Black patients (Table 1). These findings persisted despite matching for relevant clinical and biochemical covariates.
Discussion: In this large real-world analysis of patients with cirrhosis on SGLT2-i, Black patients demonstrated significantly better outcomes compared to White patients across all measured domains, including mortality, hospitalizations, and decompensated cirrhosis events. In contrast to meta-analysis of clinical trial data, the findings from large real world retrospective studies indicate SGLT2-i is associated with improved liver related outcomes. The discrepancy underscores the need for further investigation into genetic, socioeconomic, and access-related factors contributing to these disparities.
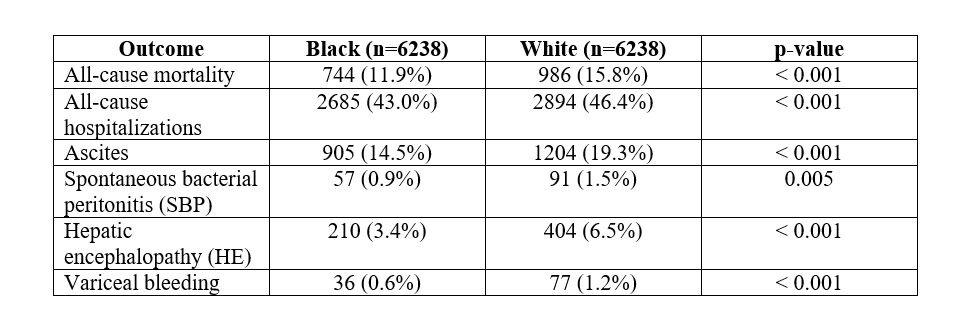
Figure: Table 1
Disclosures:
Mohamad Mahdi Osman indicated no relevant financial relationships.
Mohamad-Noor Abu-Hammour indicated no relevant financial relationships.
Varun Aitharaju indicated no relevant financial relationships.
Leandro Sierra indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Ali Syed indicated no relevant financial relationships.
Dian Jung Chiang: Ipsen – Advisory Committee/Board Member.
Mohamad Mahdi Osman, DO1, Mohamad-Noor Abu-Hammour, MD1, Varun Aitharaju, MD2, Leandro Sierra, MD3, Omar Sims, PhD4, Ali Syed, MD5, Dian Jung Chiang, MD1. P5931 - Racial Differences in Clinical Outcomes Among Cirrhotic Patients on SGLT2 Inhibitors: A Propensity-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
