Tuesday Poster Session
Category: Liver
P5926 - Comparative Outcomes of GLP-1 Receptor Agonists vs SGLT2 Inhibitors in Patients With Cirrhosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HA
Hatem Ahmed, MD
Phoenixville Hospital - Tower Health
Phoenixville, PA
Presenting Author(s)
Hatem Ahmed, MD1, Imad Alabdul Razzak, MD1, Eyad Abdulrazzak, MBBS2, Sameh Gomaa, MD1
1Phoenixville Hospital - Tower Health, Phoenixville, PA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Needham, MA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose cotransporter-2 inhibitors (SGLT2i) are widely used antidiabetic agents that are associated with cardiovascular and renal benefits in patients with type 2 diabetes. Growing evidence demonstrates benefits of GLP-1 RAs in patients with metabolic dysfunction-associated steatotic liver disease (MASLD). SGLT2 inhibitors are also linked to improvements in liver-related metrics in MASLD, including among patients with cirrhosis. However, direct comparisons in cirrhosis are limited. This study compared 1-year outcomes between GLP-1RA and SGLT2i users with cirrhosis.
Methods: We conducted a retrospective multicenter cohort study using TriNetX to identify adults with cirrhosis prescribed GLP-1RA or SGLT2i. Propensity score matching was used to balance baseline characteristics. Primary outcomes were 1-year mortality and hospitalization rates. Secondary outcomes included hepatic decompensation events: ascites, spontaneous bacterial peritonitis (SBP), variceal bleeding, hepatic encephalopathy, jaundice, hepatocellular carcinoma (HCC), and paracentesis rates. Tertiary outcomes included liver and renal biomarkers. Adverse events were also assessed.
Results: After matching, 8,847 patients remained per cohort. At 1 year, GLP-1RA use was associated with lower all-cause mortality (4.3% vs. 5.3%; OR 0.801; 95% CI: 0.693–0.927; p=0.003) and fewer hepatic decompensation events (5.7% vs. 7.1%; OR 0.788; p=0.001), including ascites (OR 0.691; p< 0.0001), need for paracentesis (OR 0.583; p< 0.0001), and SBP (OR 0.620; p=0.023). No significant differences were observed in variceal bleeding, HCC, or hepatic encephalopathy. GLP-1RA users also had lower rates of acute kidney injury (4.8% vs. 6.2%; OR 0.763; p=0.001). Adverse event rates, including hypoglycemia and pancreatitis, were similar (Table 1).
Tertiary outcomes showed modest but statistically significant improvements in AST, ALT, albumin, and INR levels in the GLP-1RA group. No significant differences were found in bilirubin, creatinine, or sodium levels (Table 2).
Discussion: Among adults with cirrhosis, GLP-1 receptor agonists were linked to lower 1-year all-cause mortality and reduced rates of ascites, spontaneous bacterial peritonitis, and paracentesis compared with SGLT2 inhibitors. They also produced modest improvements in AST, ALT, albumin, and INR. These real-world data suggest GLP-1RAs may offer broader hepatic benefits than SGLT2 inhibitors in this high-risk population.
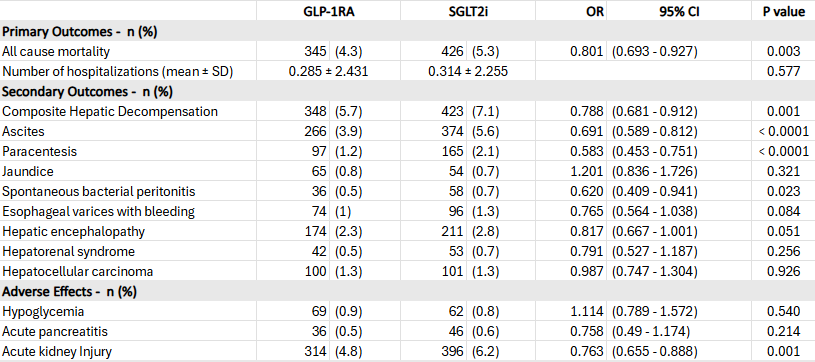
Figure: Table 1. One-year clinical outcomes in patients with cirrhosis treated with GLP-1 receptor agonists versus SGLT2 inhibitors
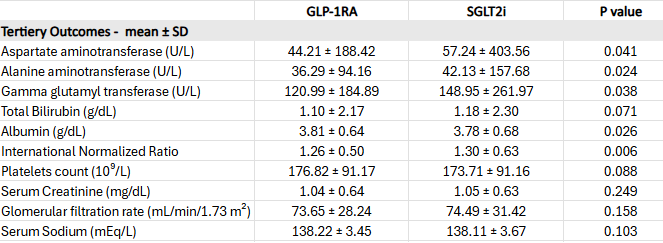
Figure: Table 2. Differences in Laboratory Parameters Between GLP-1RA and SGLT2i Cohorts in Patients With Cirrhosis
Disclosures:
Hatem Ahmed indicated no relevant financial relationships.
Imad Alabdul Razzak indicated no relevant financial relationships.
Eyad Abdulrazzak indicated no relevant financial relationships.
Sameh Gomaa indicated no relevant financial relationships.
Hatem Ahmed, MD1, Imad Alabdul Razzak, MD1, Eyad Abdulrazzak, MBBS2, Sameh Gomaa, MD1. P5926 - Comparative Outcomes of GLP-1 Receptor Agonists vs SGLT2 Inhibitors in Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Phoenixville Hospital - Tower Health, Phoenixville, PA; 2Beth Israel Deaconess Medical Center, Harvard Medical School, Needham, MA
Introduction: Glucagon-like peptide-1 receptor agonists (GLP-1RAs) and sodium-glucose cotransporter-2 inhibitors (SGLT2i) are widely used antidiabetic agents that are associated with cardiovascular and renal benefits in patients with type 2 diabetes. Growing evidence demonstrates benefits of GLP-1 RAs in patients with metabolic dysfunction-associated steatotic liver disease (MASLD). SGLT2 inhibitors are also linked to improvements in liver-related metrics in MASLD, including among patients with cirrhosis. However, direct comparisons in cirrhosis are limited. This study compared 1-year outcomes between GLP-1RA and SGLT2i users with cirrhosis.
Methods: We conducted a retrospective multicenter cohort study using TriNetX to identify adults with cirrhosis prescribed GLP-1RA or SGLT2i. Propensity score matching was used to balance baseline characteristics. Primary outcomes were 1-year mortality and hospitalization rates. Secondary outcomes included hepatic decompensation events: ascites, spontaneous bacterial peritonitis (SBP), variceal bleeding, hepatic encephalopathy, jaundice, hepatocellular carcinoma (HCC), and paracentesis rates. Tertiary outcomes included liver and renal biomarkers. Adverse events were also assessed.
Results: After matching, 8,847 patients remained per cohort. At 1 year, GLP-1RA use was associated with lower all-cause mortality (4.3% vs. 5.3%; OR 0.801; 95% CI: 0.693–0.927; p=0.003) and fewer hepatic decompensation events (5.7% vs. 7.1%; OR 0.788; p=0.001), including ascites (OR 0.691; p< 0.0001), need for paracentesis (OR 0.583; p< 0.0001), and SBP (OR 0.620; p=0.023). No significant differences were observed in variceal bleeding, HCC, or hepatic encephalopathy. GLP-1RA users also had lower rates of acute kidney injury (4.8% vs. 6.2%; OR 0.763; p=0.001). Adverse event rates, including hypoglycemia and pancreatitis, were similar (Table 1).
Tertiary outcomes showed modest but statistically significant improvements in AST, ALT, albumin, and INR levels in the GLP-1RA group. No significant differences were found in bilirubin, creatinine, or sodium levels (Table 2).
Discussion: Among adults with cirrhosis, GLP-1 receptor agonists were linked to lower 1-year all-cause mortality and reduced rates of ascites, spontaneous bacterial peritonitis, and paracentesis compared with SGLT2 inhibitors. They also produced modest improvements in AST, ALT, albumin, and INR. These real-world data suggest GLP-1RAs may offer broader hepatic benefits than SGLT2 inhibitors in this high-risk population.
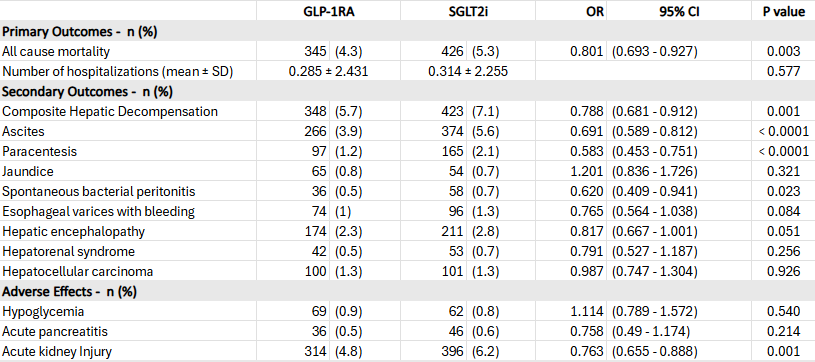
Figure: Table 1. One-year clinical outcomes in patients with cirrhosis treated with GLP-1 receptor agonists versus SGLT2 inhibitors
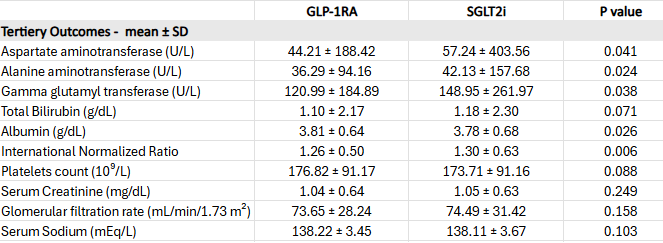
Figure: Table 2. Differences in Laboratory Parameters Between GLP-1RA and SGLT2i Cohorts in Patients With Cirrhosis
Disclosures:
Hatem Ahmed indicated no relevant financial relationships.
Imad Alabdul Razzak indicated no relevant financial relationships.
Eyad Abdulrazzak indicated no relevant financial relationships.
Sameh Gomaa indicated no relevant financial relationships.
Hatem Ahmed, MD1, Imad Alabdul Razzak, MD1, Eyad Abdulrazzak, MBBS2, Sameh Gomaa, MD1. P5926 - Comparative Outcomes of GLP-1 Receptor Agonists vs SGLT2 Inhibitors in Patients With Cirrhosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

