Tuesday Poster Session
Category: Liver
P5924 - Sodium-Glucose Cotransporter-2 Inhibitors in Cirrhosis: Impact on Mortality, Hepatic Decompensation, and Prognostic Biomarkers
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- HA
Hatem Ahmed, MD
Phoenixville Hospital - Tower Health
Phoenixville, PA
Presenting Author(s)
Hatem Ahmed, MD, Sameh Gomaa, MD, Mohammad Alazzeh, MD
Phoenixville Hospital - Tower Health, Phoenixville, PA
Introduction: Liver cirrhosis is a major cause of morbidity and mortality, with limited pharmacologic options to alter its progression. Sodium-glucose cotransporter 2 inhibitors (SGLT2i), widely used for diabetes and cardiorenal protection, have shown potential hepatoprotective effects. However, their impact on clinical outcomes in cirrhosis remains unclear. This study evaluates the association between SGLT2i use and mortality, hepatic decompensation, and prognostic markers in patients with cirrhosis.
Methods: We conducted a retrospective cohort study using the TriNetX database, comparing patients with liver cirrhosis who were prescribed SGLT2 inhibitors after their diagnosis to those who were not. Propensity score matching was used to balance baseline characteristics between groups. Outcomes were assessed at 5- and 10-year intervals and included all-cause mortality, hospitalization rates, hepatic decompensation events, prognostic laboratory markers, and adverse effects. Results are reported as percentages and odds ratios (OR) with 95% confidence intervals (CI).
Results: After propensity score matching (n = 24,559 per group), SGLT2i use was associated with significantly lower 5-year all-cause mortality (OR 0.381; 95% CI: 0.363–0.399; p < 0.0001). Hepatic decompensation was also significantly reduced in the SGLT2i group (OR 0.617; 95% CI: 0.580–0.656; p < 0.0001), including lower rates of ascites, spontaneous bacterial peritonitis, hepatorenal syndrome, and the need for paracentesis. There was no significant difference in the incidence of hepatic encephalopathy between groups (Table 1).
Additionally, SGLT2i use was associated with lower rates of acute kidney injury and urinary tract infections, without an increased incidence of diabetic ketoacidosis. These benefits persisted through the 10-year follow-up period.
SGLT2i users also demonstrated improved hepatic function, with higher serum albumin and lower total bilirubin levels, along with better renal function, evidenced by lower serum creatinine and higher estimated glomerular filtration rates (Table 2). These findings remained consistent across the 10-year follow-up.
Discussion: SGLT2i use in patients with cirrhosis was associated with improved survival, fewer hepatic decompensation events, and better renal function, without an increased risk of hepatic encephalopathy or major adverse effects. These findings support the potential role of SGLT2 inhibitors as adjunctive therapy in the management of cirrhosis.
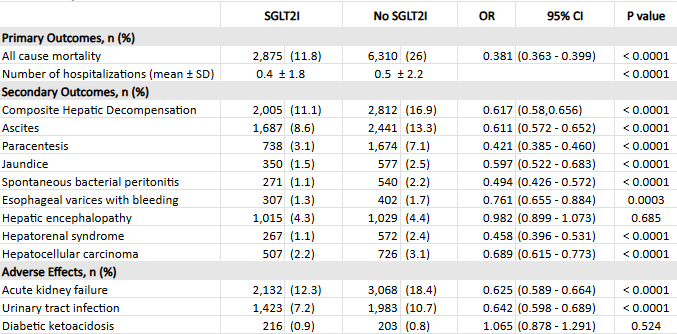
Figure: Table 1. Five-Year Outcomes in SGLT2i-Cirrhosis and Non-SGLT2i-Cirrhosis Cohorts
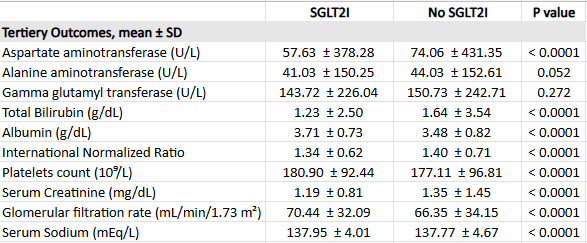
Figure: Table 2. Differences in Prognostic Markers Between SGLT2i-Cirrhosis and Non-SGLT2i-Cirrhosis Cohorts
Disclosures:
Hatem Ahmed indicated no relevant financial relationships.
Sameh Gomaa indicated no relevant financial relationships.
Mohammad Alazzeh indicated no relevant financial relationships.
Hatem Ahmed, MD, Sameh Gomaa, MD, Mohammad Alazzeh, MD. P5924 - Sodium-Glucose Cotransporter-2 Inhibitors in Cirrhosis: Impact on Mortality, Hepatic Decompensation, and Prognostic Biomarkers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Phoenixville Hospital - Tower Health, Phoenixville, PA
Introduction: Liver cirrhosis is a major cause of morbidity and mortality, with limited pharmacologic options to alter its progression. Sodium-glucose cotransporter 2 inhibitors (SGLT2i), widely used for diabetes and cardiorenal protection, have shown potential hepatoprotective effects. However, their impact on clinical outcomes in cirrhosis remains unclear. This study evaluates the association between SGLT2i use and mortality, hepatic decompensation, and prognostic markers in patients with cirrhosis.
Methods: We conducted a retrospective cohort study using the TriNetX database, comparing patients with liver cirrhosis who were prescribed SGLT2 inhibitors after their diagnosis to those who were not. Propensity score matching was used to balance baseline characteristics between groups. Outcomes were assessed at 5- and 10-year intervals and included all-cause mortality, hospitalization rates, hepatic decompensation events, prognostic laboratory markers, and adverse effects. Results are reported as percentages and odds ratios (OR) with 95% confidence intervals (CI).
Results: After propensity score matching (n = 24,559 per group), SGLT2i use was associated with significantly lower 5-year all-cause mortality (OR 0.381; 95% CI: 0.363–0.399; p < 0.0001). Hepatic decompensation was also significantly reduced in the SGLT2i group (OR 0.617; 95% CI: 0.580–0.656; p < 0.0001), including lower rates of ascites, spontaneous bacterial peritonitis, hepatorenal syndrome, and the need for paracentesis. There was no significant difference in the incidence of hepatic encephalopathy between groups (Table 1).
Additionally, SGLT2i use was associated with lower rates of acute kidney injury and urinary tract infections, without an increased incidence of diabetic ketoacidosis. These benefits persisted through the 10-year follow-up period.
SGLT2i users also demonstrated improved hepatic function, with higher serum albumin and lower total bilirubin levels, along with better renal function, evidenced by lower serum creatinine and higher estimated glomerular filtration rates (Table 2). These findings remained consistent across the 10-year follow-up.
Discussion: SGLT2i use in patients with cirrhosis was associated with improved survival, fewer hepatic decompensation events, and better renal function, without an increased risk of hepatic encephalopathy or major adverse effects. These findings support the potential role of SGLT2 inhibitors as adjunctive therapy in the management of cirrhosis.
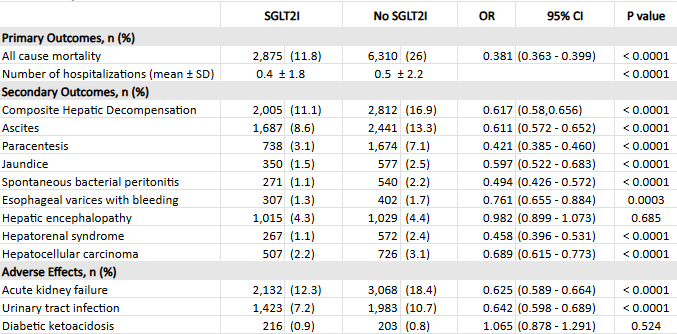
Figure: Table 1. Five-Year Outcomes in SGLT2i-Cirrhosis and Non-SGLT2i-Cirrhosis Cohorts
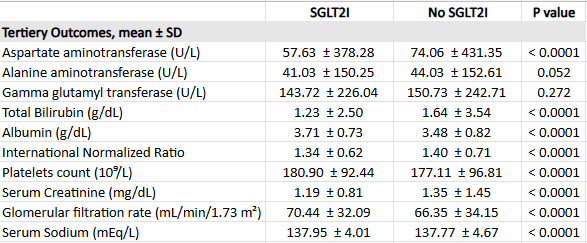
Figure: Table 2. Differences in Prognostic Markers Between SGLT2i-Cirrhosis and Non-SGLT2i-Cirrhosis Cohorts
Disclosures:
Hatem Ahmed indicated no relevant financial relationships.
Sameh Gomaa indicated no relevant financial relationships.
Mohammad Alazzeh indicated no relevant financial relationships.
Hatem Ahmed, MD, Sameh Gomaa, MD, Mohammad Alazzeh, MD. P5924 - Sodium-Glucose Cotransporter-2 Inhibitors in Cirrhosis: Impact on Mortality, Hepatic Decompensation, and Prognostic Biomarkers, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

