Tuesday Poster Session
Category: Liver
P5905 - Racial Disparities in Liver Transplantation Among Patients With Primary Sclerosing Cholangitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Alexander Worix, MD (he/him/his)
University of California San Francisco
San Francisco, CA
Presenting Author(s)
Alexander Worix, MD, Isaac Benque, MD, Jennifer Lai, MD, MBA, Sharad Wadhwani, MD, Michael Li, MD
University of California San Francisco, San Francisco, CA
Introduction: Primary sclerosing cholangitis (PSC) is a progressive hepatobiliary disease without effective medical therapies other than liver transplantation (LT). However, disparities in LT access and outcomes for minority patients with PSC remain poorly defined.
Methods: We conducted a retrospective cohort analysis using the United Network for Organ Sharing database from 2010-2024. PSC patients listed for LT were stratified by race (non-white vs white). Multivariable competing risks regression was used to investigate the primary outcome of time to waitlist dropout (due to being too sick) or mortality, accounting for LT as a competing risk. Secondary outcomes were time to post-LT graft failure, living donor LT, and listing for cholangiocarcinoma.
Results: Among 7,636 PSC patients evaluated, 5733 were white and 1903 were non-white; most non-white patients were black (62%). Over time, the proportion of non-white patients with PSC listed for LT has risen (Fig A). Non-white patients had higher MELD scores at listing (20 vs 17, p< 0.001) and were less likely to have concurrent inflammatory bowel disease (61% vs 73%, p< 0.001). Only 28 [1.5%] non-white patients with cholangiocarcinoma were listed for LT compared to 253 [4.4%] white patients (p< 0.001). Donation after circulatory death graft utilization was similar between the two groups; however, non-white patients were half as likely to undergo living donor LT (6% vs 12%, RR 0.5, p< 0.001). There was no difference in risk of waitlist dropout/mortality between white and non-white patients on competing risks regression (aHR 1.1, 95% CI 0.8-1.5, p=0.7; Fig B), though measures of socioeconomic status like education level (HR 0.8, 95% CI 0.7-0.9, p< 0.001) and public insurance (HR 1.4, 95% CI 1.1-1.7, p< 0.001) were associated with waitlist dropout/mortality. Race, education status, and insurance type were not associated with time to graft failure on Cox regression.
Discussion: Racial disparities persist in access to liver transplantation for PSC, as non-white patients are less likely to receive living donor LT and less likely to be listed with concurrent cholangiocarcinoma. Despite these disparities, clinical outcomes were largely similar, suggesting resilience in care once access is achieved, though measures of socioeconomic status remained associated with waitlist outcomes. Interventions are needed to address barriers to early diagnosis, subspecialty referral, and living donor education in minority communities.
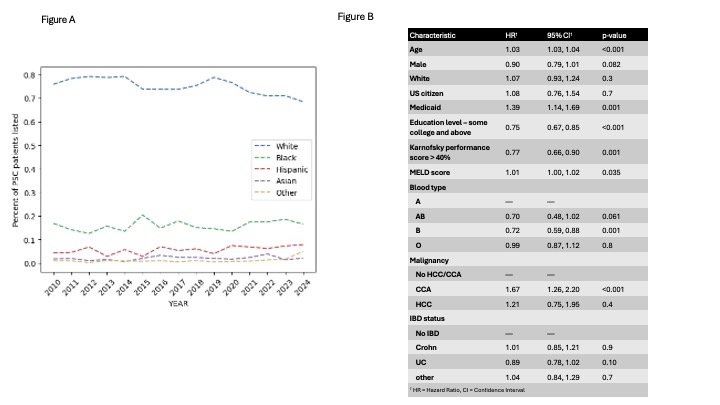
Figure: Figure A - Proportion of PSC Patients Listed by Ethnicity; Figure B - Competing Risks Regression Model, Time to Waitlist Dropout or Mortality
Disclosures:
Alexander Worix indicated no relevant financial relationships.
Isaac Benque indicated no relevant financial relationships.
Jennifer Lai: Boehringer Ingelheim – Consultant. Genfit – Consultant. Lipocene – Grant/Research Support. Nestle Nutrition Services – Grant/Research Support. Novo Nordisk – Advisory Committee/Board Member. Third Rock Ventures – Consultant. Vir Biotechnologies – Grant/Research Support.
Sharad Wadhwani indicated no relevant financial relationships.
Michael Li indicated no relevant financial relationships.
Alexander Worix, MD, Isaac Benque, MD, Jennifer Lai, MD, MBA, Sharad Wadhwani, MD, Michael Li, MD. P5905 - Racial Disparities in Liver Transplantation Among Patients With Primary Sclerosing Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of California San Francisco, San Francisco, CA
Introduction: Primary sclerosing cholangitis (PSC) is a progressive hepatobiliary disease without effective medical therapies other than liver transplantation (LT). However, disparities in LT access and outcomes for minority patients with PSC remain poorly defined.
Methods: We conducted a retrospective cohort analysis using the United Network for Organ Sharing database from 2010-2024. PSC patients listed for LT were stratified by race (non-white vs white). Multivariable competing risks regression was used to investigate the primary outcome of time to waitlist dropout (due to being too sick) or mortality, accounting for LT as a competing risk. Secondary outcomes were time to post-LT graft failure, living donor LT, and listing for cholangiocarcinoma.
Results: Among 7,636 PSC patients evaluated, 5733 were white and 1903 were non-white; most non-white patients were black (62%). Over time, the proportion of non-white patients with PSC listed for LT has risen (Fig A). Non-white patients had higher MELD scores at listing (20 vs 17, p< 0.001) and were less likely to have concurrent inflammatory bowel disease (61% vs 73%, p< 0.001). Only 28 [1.5%] non-white patients with cholangiocarcinoma were listed for LT compared to 253 [4.4%] white patients (p< 0.001). Donation after circulatory death graft utilization was similar between the two groups; however, non-white patients were half as likely to undergo living donor LT (6% vs 12%, RR 0.5, p< 0.001). There was no difference in risk of waitlist dropout/mortality between white and non-white patients on competing risks regression (aHR 1.1, 95% CI 0.8-1.5, p=0.7; Fig B), though measures of socioeconomic status like education level (HR 0.8, 95% CI 0.7-0.9, p< 0.001) and public insurance (HR 1.4, 95% CI 1.1-1.7, p< 0.001) were associated with waitlist dropout/mortality. Race, education status, and insurance type were not associated with time to graft failure on Cox regression.
Discussion: Racial disparities persist in access to liver transplantation for PSC, as non-white patients are less likely to receive living donor LT and less likely to be listed with concurrent cholangiocarcinoma. Despite these disparities, clinical outcomes were largely similar, suggesting resilience in care once access is achieved, though measures of socioeconomic status remained associated with waitlist outcomes. Interventions are needed to address barriers to early diagnosis, subspecialty referral, and living donor education in minority communities.
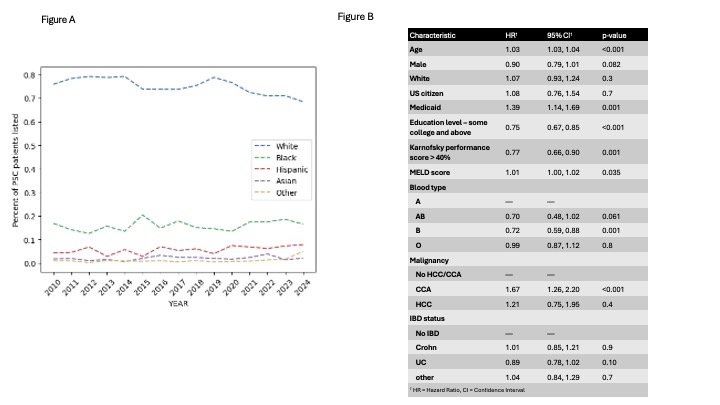
Figure: Figure A - Proportion of PSC Patients Listed by Ethnicity; Figure B - Competing Risks Regression Model, Time to Waitlist Dropout or Mortality
Disclosures:
Alexander Worix indicated no relevant financial relationships.
Isaac Benque indicated no relevant financial relationships.
Jennifer Lai: Boehringer Ingelheim – Consultant. Genfit – Consultant. Lipocene – Grant/Research Support. Nestle Nutrition Services – Grant/Research Support. Novo Nordisk – Advisory Committee/Board Member. Third Rock Ventures – Consultant. Vir Biotechnologies – Grant/Research Support.
Sharad Wadhwani indicated no relevant financial relationships.
Michael Li indicated no relevant financial relationships.
Alexander Worix, MD, Isaac Benque, MD, Jennifer Lai, MD, MBA, Sharad Wadhwani, MD, Michael Li, MD. P5905 - Racial Disparities in Liver Transplantation Among Patients With Primary Sclerosing Cholangitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
