Tuesday Poster Session
Category: Liver
P5895 - Process Measures of Care and Their Impact on Mortality in Hospitalized Patients With Alcohol-Associated Hepatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CF
Conrad J. Fernandes, MD
Baylor College of Medicine
Houston, TX
Presenting Author(s)
Conrad J. Fernandes, MD1, Lauren Shaffer, MD1, Nagasri Shankar, MD1, George Cholankeril, MD1, Ruben Hernaez, MD, MPH, PhD1, Kavish Patidar, DO2
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Alcohol-associated hepatitis (AH) is a severe form of alcohol-associated liver disease with high mortality. While process measures (PMs) have been proposed to standardize and improve AH management, their implementation and impact on patient outcomes remain poorly understood.
Methods: We conducted a retrospective study of adult patients diagnosed with AH who were admitted to an academic tertiary care center between 1/1/2023 and 12/31/2023. We included patients with probable or definite AH per the National Institute on Alcohol Abuse and Alcoholism Alcoholic Hepatitis Consortia criteria. We evaluated four key PMs: timely (within 48hrs of admission) nutritional assessment, timely (within 48hrs of admission) infection screening, receipt of alcohol rehabilitation resources, and non-selective beta-blocker (NSBB) prescription at discharge. To determine the impact of these PMs on patient outcomes, we used multivariate Cox-regression models to assess the independent association between each PM and 90-day mortality.
Results: A total of 101 patients with AH were included for analysis (median age 48yrs, 42% female, and median admission phosphatidylethanol 212 ng/mL). Severe AH (sAH), defined as Model for End-stage Liver Disease (MELD) score >20, was present in 76%, and the overall median MELD score was 25 (Table 1). Implementation of PMs varied, with only 12% of patients receiving at least 3 out of 4 PMs. Timely infection screening was the most frequently implemented PM (54%), followed by receipt of alcohol rehabilitation resources and timely nutritional assessment (both at 41%), while NSBB prescription at discharge was the least common (9%). The 90-day mortality rate was 21%. After adjusting for age, sex, and MELD score, only receipt of alcohol rehabilitation resources was independently associated with decreased mortality risk (HR 0.38, 95%CI 0.11-0.91, p=0.03) (Table 2). Subgroup analysis of patients with sAH showed consistent results, with receipt of alcohol rehabilitation resources remaining the only PM independently associated with decreased mortality risk (HR 0.21, 95%CI 0.06-0.69, p=0.01).
Discussion: This study reveals significant gaps in implementing key PMs for AH care, with receipt of alcohol rehabilitation resources having the greatest benefit for survival. These findings underscore the importance of integrating alcohol use disorder treatment into in-hospital AH management and highlight opportunities for quality improvement initiatives.
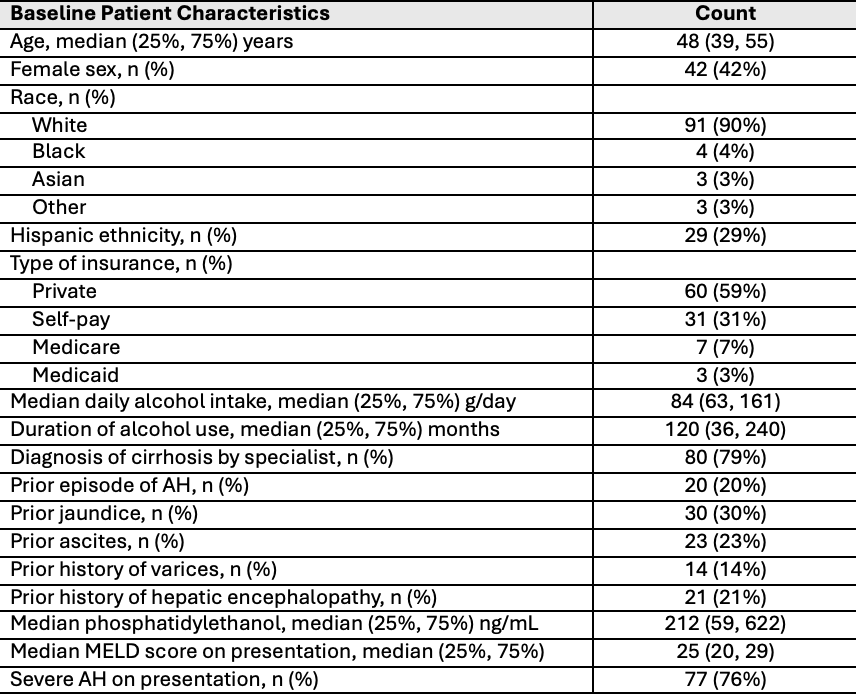
Figure: Table 1: Baseline patient demographics and clinical characteristics
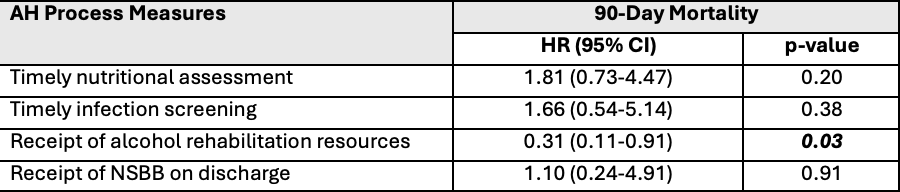
Figure: Table 2: Alcohol-associated hepatitis process measures and 90-day-mortality adjusted for age, sex, and MELD score
Disclosures:
Conrad Fernandes indicated no relevant financial relationships.
Lauren Shaffer indicated no relevant financial relationships.
Nagasri Shankar indicated no relevant financial relationships.
George Cholankeril indicated no relevant financial relationships.
Ruben Hernaez indicated no relevant financial relationships.
Kavish Patidar: Madrigal Pharmaceuticals – Advisor or Review Panel Member. Mallinckrodt Pharmaceuticals – Consultant.
Conrad J. Fernandes, MD1, Lauren Shaffer, MD1, Nagasri Shankar, MD1, George Cholankeril, MD1, Ruben Hernaez, MD, MPH, PhD1, Kavish Patidar, DO2. P5895 - Process Measures of Care and Their Impact on Mortality in Hospitalized Patients With Alcohol-Associated Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Baylor College of Medicine, Houston, TX; 2Baylor College of Medicine / Michael E. DeBakey Veterans Affairs Medical Center, Houston, TX
Introduction: Alcohol-associated hepatitis (AH) is a severe form of alcohol-associated liver disease with high mortality. While process measures (PMs) have been proposed to standardize and improve AH management, their implementation and impact on patient outcomes remain poorly understood.
Methods: We conducted a retrospective study of adult patients diagnosed with AH who were admitted to an academic tertiary care center between 1/1/2023 and 12/31/2023. We included patients with probable or definite AH per the National Institute on Alcohol Abuse and Alcoholism Alcoholic Hepatitis Consortia criteria. We evaluated four key PMs: timely (within 48hrs of admission) nutritional assessment, timely (within 48hrs of admission) infection screening, receipt of alcohol rehabilitation resources, and non-selective beta-blocker (NSBB) prescription at discharge. To determine the impact of these PMs on patient outcomes, we used multivariate Cox-regression models to assess the independent association between each PM and 90-day mortality.
Results: A total of 101 patients with AH were included for analysis (median age 48yrs, 42% female, and median admission phosphatidylethanol 212 ng/mL). Severe AH (sAH), defined as Model for End-stage Liver Disease (MELD) score >20, was present in 76%, and the overall median MELD score was 25 (Table 1). Implementation of PMs varied, with only 12% of patients receiving at least 3 out of 4 PMs. Timely infection screening was the most frequently implemented PM (54%), followed by receipt of alcohol rehabilitation resources and timely nutritional assessment (both at 41%), while NSBB prescription at discharge was the least common (9%). The 90-day mortality rate was 21%. After adjusting for age, sex, and MELD score, only receipt of alcohol rehabilitation resources was independently associated with decreased mortality risk (HR 0.38, 95%CI 0.11-0.91, p=0.03) (Table 2). Subgroup analysis of patients with sAH showed consistent results, with receipt of alcohol rehabilitation resources remaining the only PM independently associated with decreased mortality risk (HR 0.21, 95%CI 0.06-0.69, p=0.01).
Discussion: This study reveals significant gaps in implementing key PMs for AH care, with receipt of alcohol rehabilitation resources having the greatest benefit for survival. These findings underscore the importance of integrating alcohol use disorder treatment into in-hospital AH management and highlight opportunities for quality improvement initiatives.
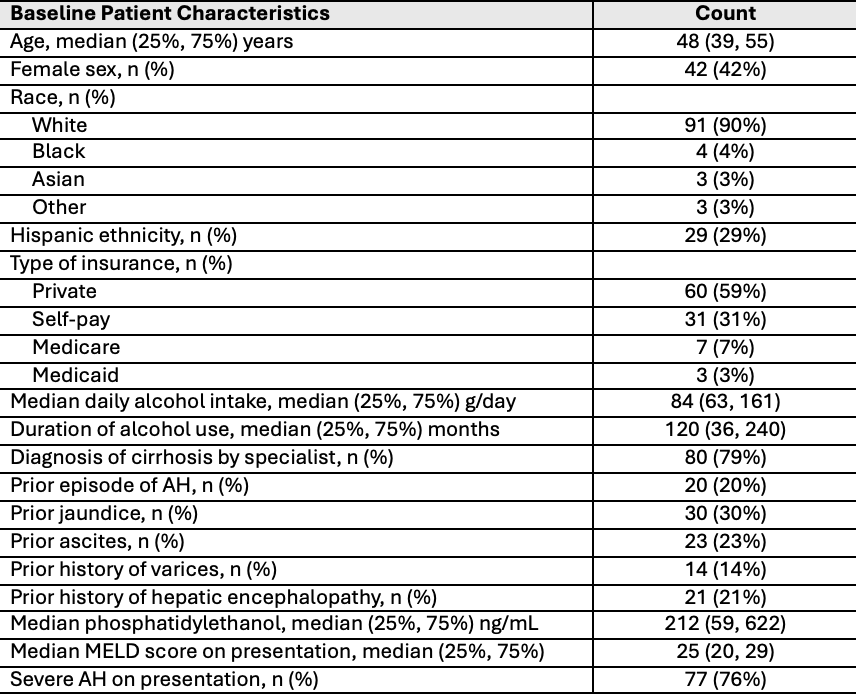
Figure: Table 1: Baseline patient demographics and clinical characteristics
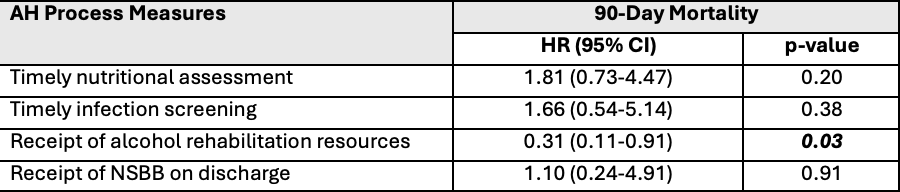
Figure: Table 2: Alcohol-associated hepatitis process measures and 90-day-mortality adjusted for age, sex, and MELD score
Disclosures:
Conrad Fernandes indicated no relevant financial relationships.
Lauren Shaffer indicated no relevant financial relationships.
Nagasri Shankar indicated no relevant financial relationships.
George Cholankeril indicated no relevant financial relationships.
Ruben Hernaez indicated no relevant financial relationships.
Kavish Patidar: Madrigal Pharmaceuticals – Advisor or Review Panel Member. Mallinckrodt Pharmaceuticals – Consultant.
Conrad J. Fernandes, MD1, Lauren Shaffer, MD1, Nagasri Shankar, MD1, George Cholankeril, MD1, Ruben Hernaez, MD, MPH, PhD1, Kavish Patidar, DO2. P5895 - Process Measures of Care and Their Impact on Mortality in Hospitalized Patients With Alcohol-Associated Hepatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
