Tuesday Poster Session
Category: Liver
P5870 - Lifestyle Medicine RPM Program for Metabolic Dysfunction-Associated Liver Disease (MASLD)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Erin Hendriks, MD (she/her/hers)
Salvo Health, MI
Presenting Author(s)
Award: ACG Presidential Poster Award
Sheena Batura, MS, RDN, CSOWM, LD1, Naresh Gunaratnam, MD2, Partha Nandi, MD3, Sejal Gunaratnam, MS4, Alyssa Guberman, BS5, Erin Hendriks, MD6
1Salvo Health, Leander, TX; 2MNGI Digestive Health, Minneapolis, MN; 3Pinnacle GI Partners, Troy, MI; 4University of Toledo College Medicine and Life Sciences, Perrysburg, OH; 5Salvo Health, New York, NY; 6Salvo Health, Bloomfield Township, MI
Introduction: MASLD affects ~30% of the U.S. population, with prevalence rising.¹ MASH, a subtype, can progress to cirrhosis, hepatocellular carcinoma, and death.² Studies show ~5% weight loss can reduce steatosis, with up to 10% reversing steatohepatitis and fibrosis. About 650 million adults worldwide have obesity (BMI ≥30), a key indicator for MASH and MASLD.³ Lifestyle interventions are key to treatment for both, yet clinical implementation remains inconsistent.
Develop a lifestyle medicine-focused remote patient monitoring (RPM) program to treat and reverse MASLD and obesity by systematically integrating evidence-based interventions.
Methods: Patients with MASLD or obesity were enrolled in an RPM program featuring a connected scale and mobile app for education, habit tracking, and self-monitoring. Monthly phone or video visits with a licensed practical nurse and registered dietitian followed a structured lifestyle medicine protocol—to optimize nutrition, physical activity, stress, sleep, or social connection at each visit—paired with personalized goals and coaching. Over three months, outcomes including weight loss, engagement, and adherence were tracked. Patient-reported outcomes were assessed using the PROMIS Global Health Scale 1.2. Pearson correlations evaluated the relationship between engagement (monthly weight readings and app logins) and weight loss.
Results: Among 161 patients enrolled (82 with MASLD; 84 with obesity), 80% were women and the mean age was 63 years. Sixty-nine percent (n = 115) lost weight after ≥90 days in the program. Clinically meaningful weight loss—defined as a ≥3% reduction in body weight—was achieved by 32% (n = 53). Digital engagement was directionally positively associated with weight loss. Average monthly weight readings showed a weak but statistically significant correlation (r = 0.181, p = 0.019), as did monthly app logins (r = 0.164, p = 0.035).
Patient‑reported outcomes improved by 56% (n = 93), indicating benefit beyond weight loss. Among those reporting improvement, 46% had MASLD and 54% had obesity.
Discussion: A structured, diagnosis-specific remote care model integrating lifestyle medicine can drive meaningful weight loss and improvements in well-being. Digital engagement—through self-monitoring and app use—was modestly associated with better outcomes, highlighting the role of behavior change as a key tool in remote care. Future iterations of the program will explore group-based support to further enhance clinical impact and patient-reported outcomes.
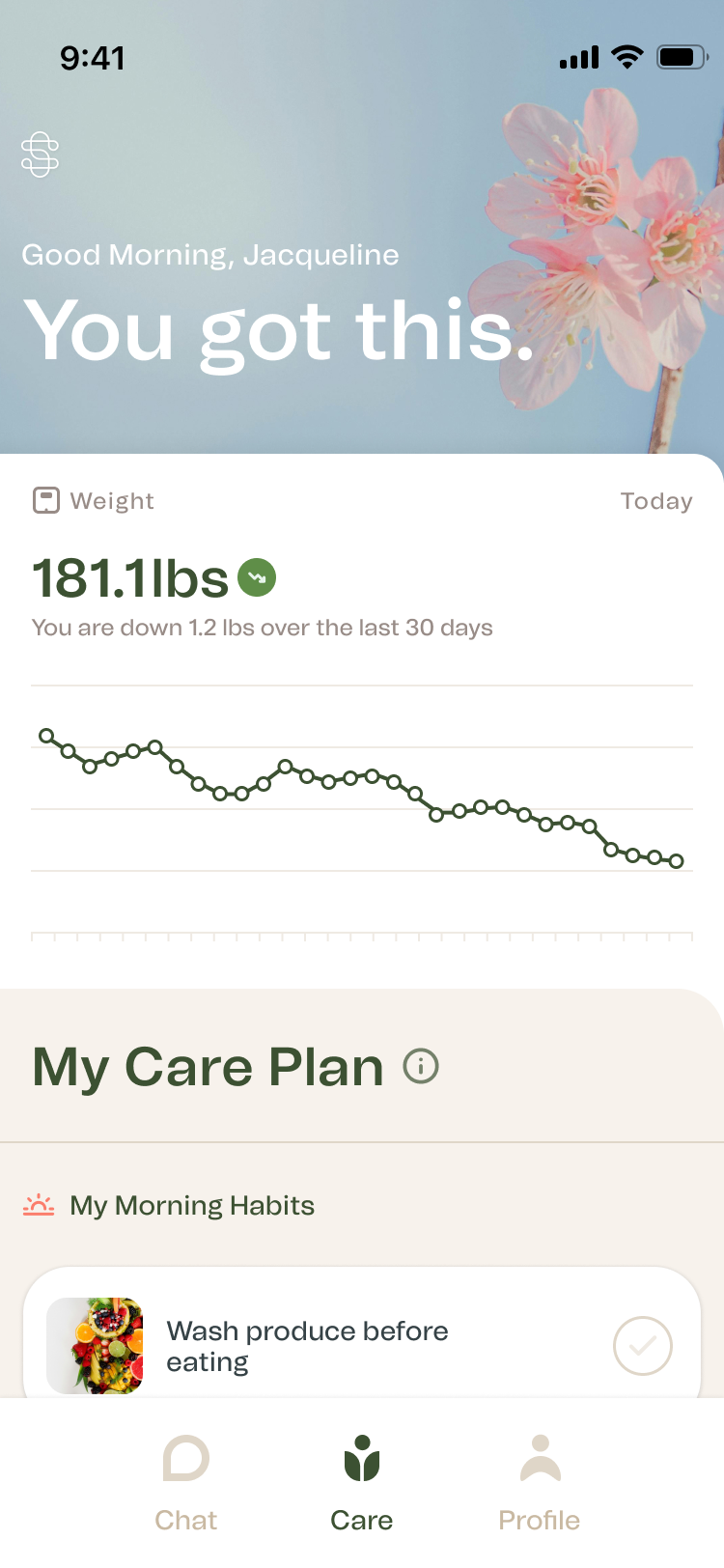
Figure: Reading Visualization in App
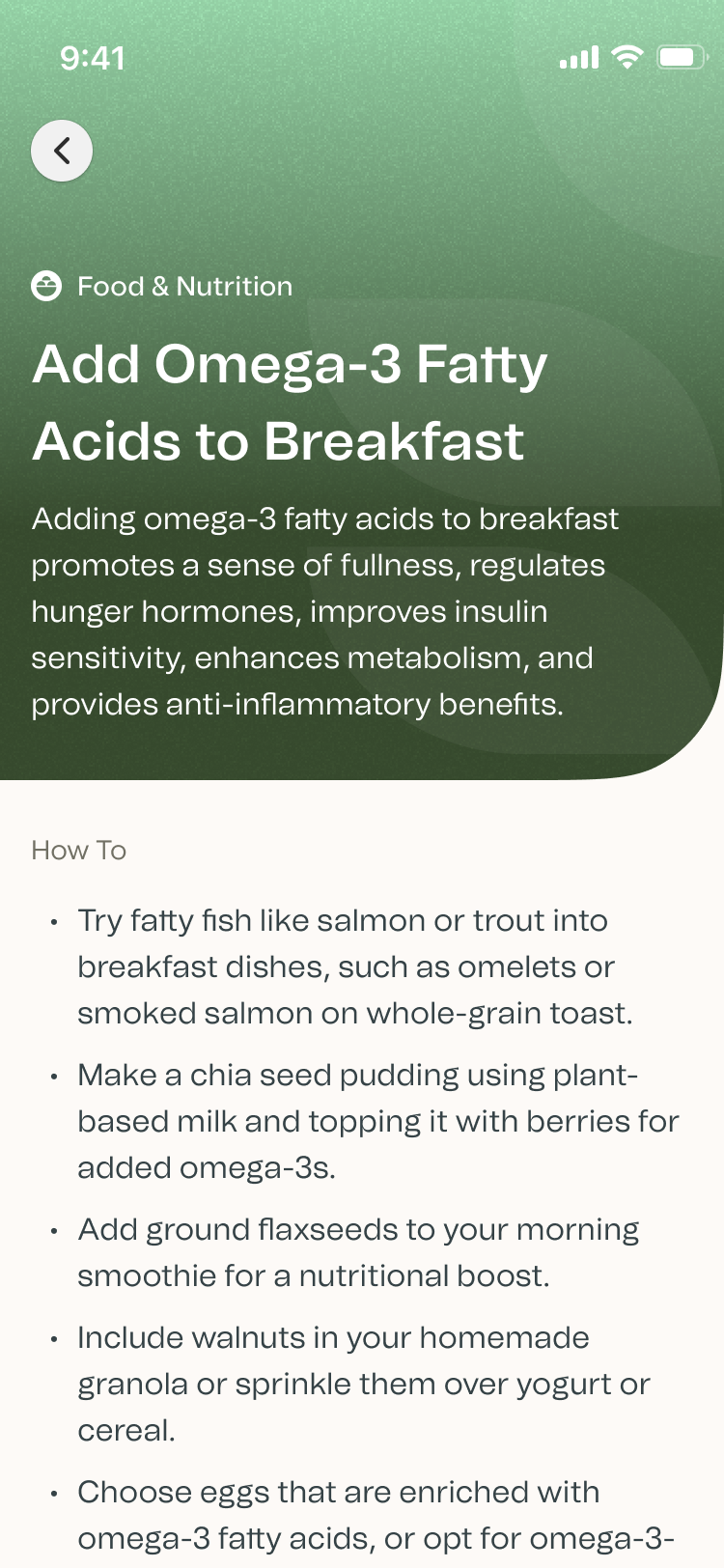
Figure: Detailed View of Content in App
Disclosures:
Sheena Batura indicated no relevant financial relationships.
Naresh Gunaratnam indicated no relevant financial relationships.
Partha Nandi indicated no relevant financial relationships.
Sejal Gunaratnam indicated no relevant financial relationships.
Alyssa Guberman indicated no relevant financial relationships.
Erin Hendriks indicated no relevant financial relationships.
Sheena Batura, MS, RDN, CSOWM, LD1, Naresh Gunaratnam, MD2, Partha Nandi, MD3, Sejal Gunaratnam, MS4, Alyssa Guberman, BS5, Erin Hendriks, MD6. P5870 - Lifestyle Medicine RPM Program for Metabolic Dysfunction-Associated Liver Disease (MASLD), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Sheena Batura, MS, RDN, CSOWM, LD1, Naresh Gunaratnam, MD2, Partha Nandi, MD3, Sejal Gunaratnam, MS4, Alyssa Guberman, BS5, Erin Hendriks, MD6
1Salvo Health, Leander, TX; 2MNGI Digestive Health, Minneapolis, MN; 3Pinnacle GI Partners, Troy, MI; 4University of Toledo College Medicine and Life Sciences, Perrysburg, OH; 5Salvo Health, New York, NY; 6Salvo Health, Bloomfield Township, MI
Introduction: MASLD affects ~30% of the U.S. population, with prevalence rising.¹ MASH, a subtype, can progress to cirrhosis, hepatocellular carcinoma, and death.² Studies show ~5% weight loss can reduce steatosis, with up to 10% reversing steatohepatitis and fibrosis. About 650 million adults worldwide have obesity (BMI ≥30), a key indicator for MASH and MASLD.³ Lifestyle interventions are key to treatment for both, yet clinical implementation remains inconsistent.
Develop a lifestyle medicine-focused remote patient monitoring (RPM) program to treat and reverse MASLD and obesity by systematically integrating evidence-based interventions.
Methods: Patients with MASLD or obesity were enrolled in an RPM program featuring a connected scale and mobile app for education, habit tracking, and self-monitoring. Monthly phone or video visits with a licensed practical nurse and registered dietitian followed a structured lifestyle medicine protocol—to optimize nutrition, physical activity, stress, sleep, or social connection at each visit—paired with personalized goals and coaching. Over three months, outcomes including weight loss, engagement, and adherence were tracked. Patient-reported outcomes were assessed using the PROMIS Global Health Scale 1.2. Pearson correlations evaluated the relationship between engagement (monthly weight readings and app logins) and weight loss.
Results: Among 161 patients enrolled (82 with MASLD; 84 with obesity), 80% were women and the mean age was 63 years. Sixty-nine percent (n = 115) lost weight after ≥90 days in the program. Clinically meaningful weight loss—defined as a ≥3% reduction in body weight—was achieved by 32% (n = 53). Digital engagement was directionally positively associated with weight loss. Average monthly weight readings showed a weak but statistically significant correlation (r = 0.181, p = 0.019), as did monthly app logins (r = 0.164, p = 0.035).
Patient‑reported outcomes improved by 56% (n = 93), indicating benefit beyond weight loss. Among those reporting improvement, 46% had MASLD and 54% had obesity.
Discussion: A structured, diagnosis-specific remote care model integrating lifestyle medicine can drive meaningful weight loss and improvements in well-being. Digital engagement—through self-monitoring and app use—was modestly associated with better outcomes, highlighting the role of behavior change as a key tool in remote care. Future iterations of the program will explore group-based support to further enhance clinical impact and patient-reported outcomes.
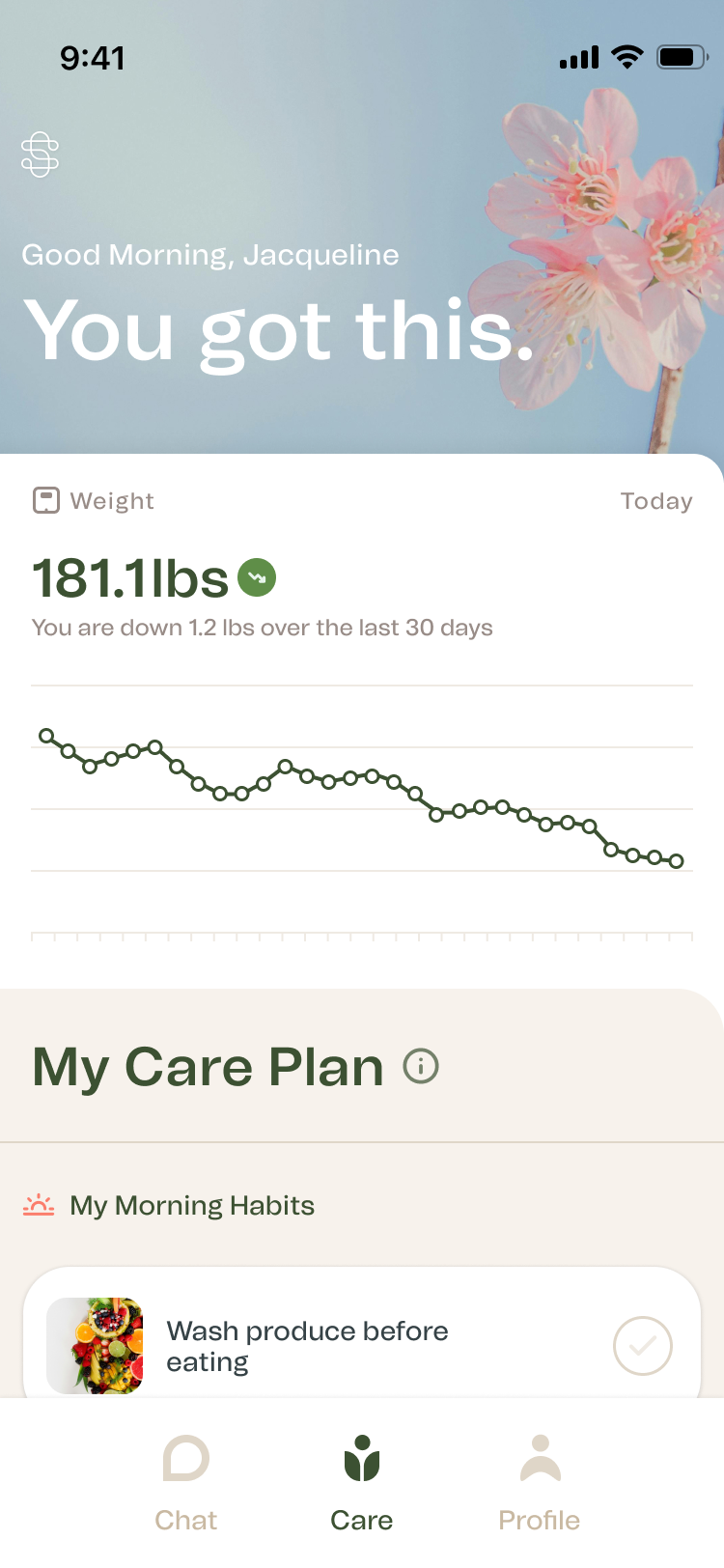
Figure: Reading Visualization in App
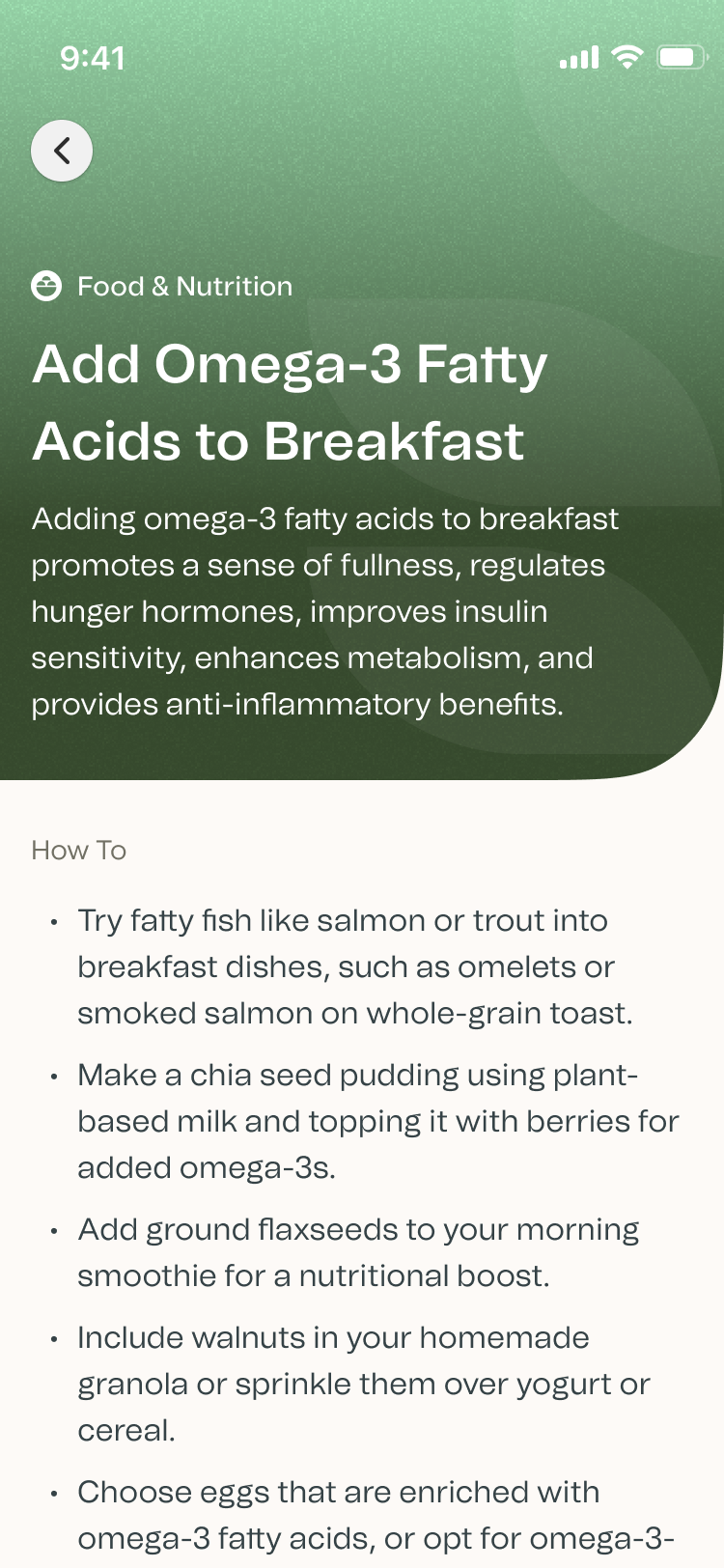
Figure: Detailed View of Content in App
Disclosures:
Sheena Batura indicated no relevant financial relationships.
Naresh Gunaratnam indicated no relevant financial relationships.
Partha Nandi indicated no relevant financial relationships.
Sejal Gunaratnam indicated no relevant financial relationships.
Alyssa Guberman indicated no relevant financial relationships.
Erin Hendriks indicated no relevant financial relationships.
Sheena Batura, MS, RDN, CSOWM, LD1, Naresh Gunaratnam, MD2, Partha Nandi, MD3, Sejal Gunaratnam, MS4, Alyssa Guberman, BS5, Erin Hendriks, MD6. P5870 - Lifestyle Medicine RPM Program for Metabolic Dysfunction-Associated Liver Disease (MASLD), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

