Tuesday Poster Session
Category: Liver
P5858 - Drug-Induced Liver Injury in Hospitalized Adults: US National Trends, Outcomes and Mortality Predictors
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Charmy Parikh, MD
Mercy Catholic Medical Center
Darby, PA
Presenting Author(s)
Charmy Parikh, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Karan J.. Yagnik, MD4, Yash Shah, MD5, Pranav Patel, MD6, Yash Shah, MD1, Umang Patel, DO2, Steven Russell, MD1
1Mercy Catholic Medical Center, Darby, PA; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6Geisinger Health System, Danville, PA
Introduction: Drug-induced liver Injury (DILI) accounts for approximately 10% of all acute hepatitis cases, and has an annual global incidence of 14 to 19.1 cases per 100,000 individuals exposed. In this study, we aim to analyze inpatient hospital outcomes of patients admitted with DILI using data from one of the largest inpatient archives in the US.
Methods: A retrospective cohort study was conducted to identify and analyze hospitalized cases of DILI in adult patients ( > 18 years) using ICD-10 codes from the National Inpatient Sample (NIS) database 2016-2020. We focused on in-hospital outcomes like trends in mortality, length of stay, hospital costs, and complications of DILI using cochran armitage test. We also conducted multivariate regression analysis to find predictors of mortality. Results are presented as adjusted odds ratios with 95% CI using a significant threshold of p< 0.05.
Results: A total of 70,705 hospitalizations were analyzed between 2016 and 2020 (mean age 54.57 years, 52.60% female). Mortality declined significantly from 6.32% in 2016 to 5.75% in 2020 (p < 0.05), though the association was weak (Cramer’s V = 0.017). DILI was linked to an average hospital stay of 7.89 days, with no significant change from 7.35 days in 2016 to 8.72 days in 2020 (p > 0.05). Inflation-adjusted mean hospital charges increased significantly from $19,955 in 2016 to $27,919 in 2020 (p < 0.05).
Predictors of mortality included age > 60 (OR: 1.334, 95% CI: 1.18–1.57, p < 0.05), self-pay as the primary payer (OR: 1.957, 95% CI: 1.67–2.28, p < 0.05), and hospitals in the Northeast (OR: 1.16, 95% CI: 1.05–1.27, p < 0.05). Patient-level predictors included ascites (OR: 1.79, 95% CI: 1.63–1.97, p < 0.05), coagulopathy (OR: 1.25, 95% CI: 1.05–1.49, p < 0.05), SBP (OR: 1.89, 95% CI: 1.56–2.29), jaundice (OR: 1.462, 95% CI: 1.08–1.97), hepatic encephalopathy (OR: 1.42, 95% CI: 1.27–1.60), and HRS (OR: 3.89, 95% CI: 3.47–4.36). Conversely, conditions like CKD (OR: 0.96, 95% CI: 0.88–1.05) and hypoalbuminemia (OR: 0.97, 95% CI: 0.83–1.15) were not significantly associated with increased mortality.
Discussion: We noted a significant decline in mortality rates and increased hospital charges for DILI patients from 2016 to 2020. Mortality was strongly associated with factors such as age > 60, AKI, ascites, and HRS. These findings reveal the burden of DILI on healthcare systems and the importance of early risk stratification and focused intervention in high-risk populations.
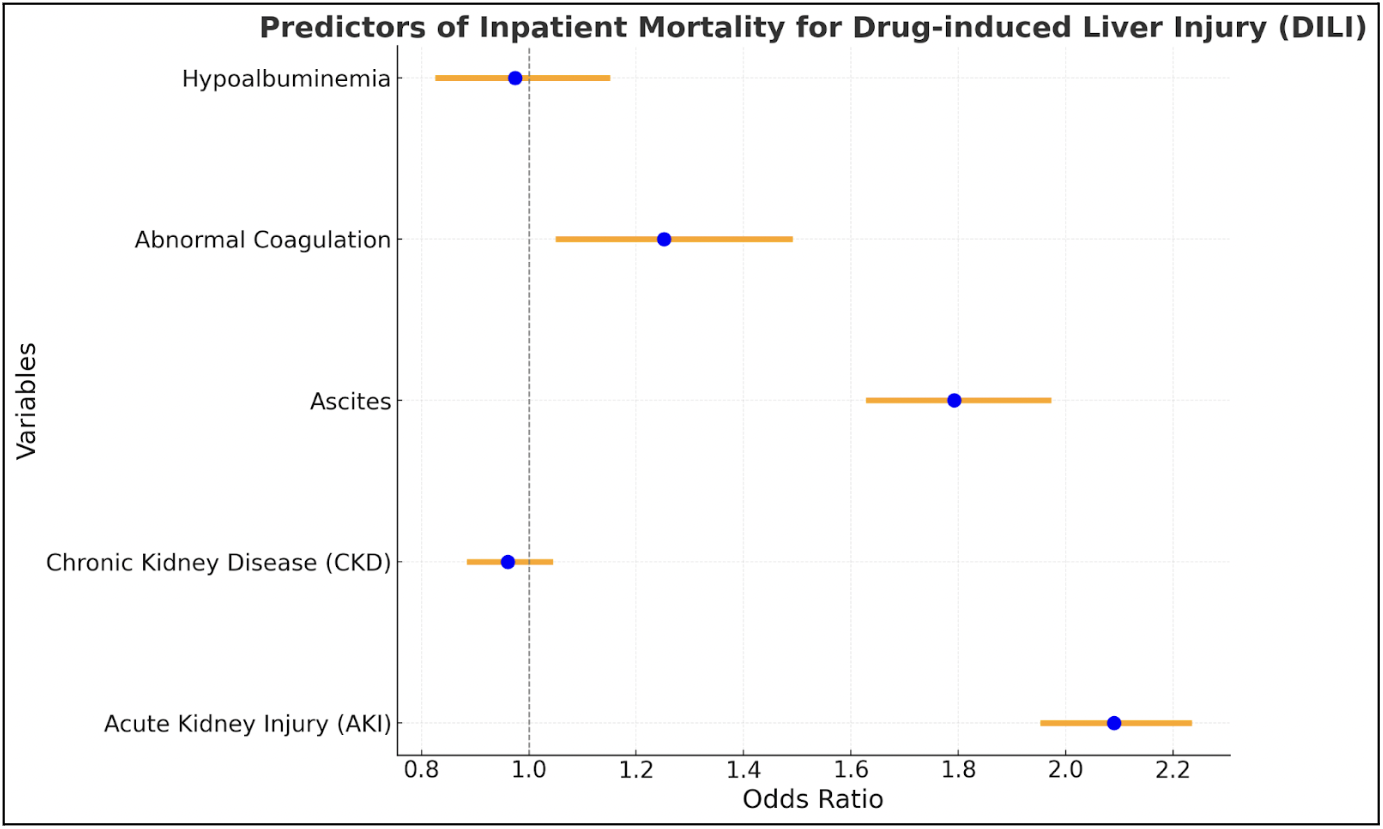
Figure: Yearwise Inpatient Mortality Trends from Drug Induced Liver Injury (DILI)
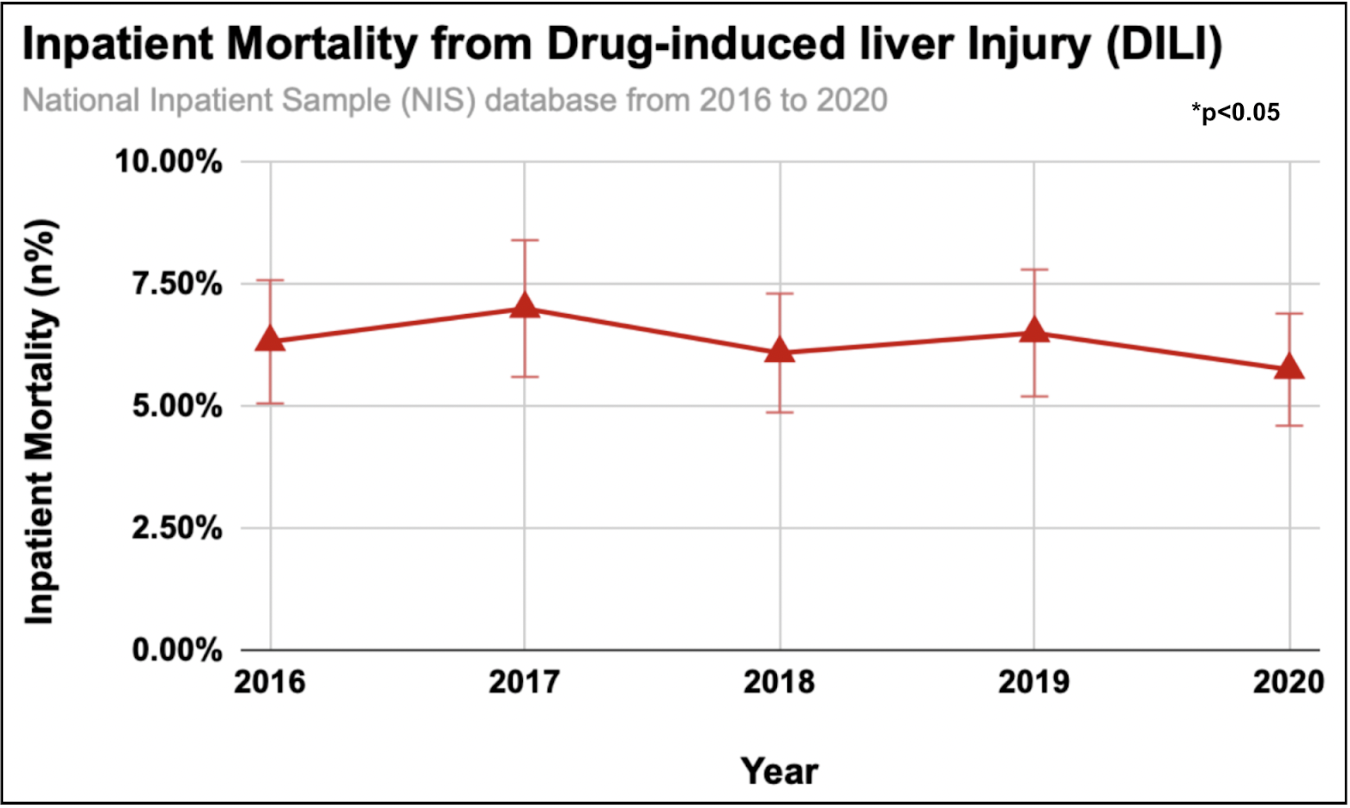
Figure: Predictors of Inpatient Mortality in Drug Induced Liver Injury (DILI)
Disclosures:
Charmy Parikh indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Umang Patel indicated no relevant financial relationships.
Steven Russell indicated no relevant financial relationships.
Charmy Parikh, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Karan J.. Yagnik, MD4, Yash Shah, MD5, Pranav Patel, MD6, Yash Shah, MD1, Umang Patel, DO2, Steven Russell, MD1. P5858 - Drug-Induced Liver Injury in Hospitalized Adults: US National Trends, Outcomes and Mortality Predictors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mercy Catholic Medical Center, Darby, PA; 2St. Mary Medical Center, Langhorne, PA; 3Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 4Monmouth Medical Center, Robert Wood Johnson Medical School of Rutgers University, Long Branch, NJ; 5Trinity Health Oakland / Wayne State University School of Medicine, Pontiac, MI; 6Geisinger Health System, Danville, PA
Introduction: Drug-induced liver Injury (DILI) accounts for approximately 10% of all acute hepatitis cases, and has an annual global incidence of 14 to 19.1 cases per 100,000 individuals exposed. In this study, we aim to analyze inpatient hospital outcomes of patients admitted with DILI using data from one of the largest inpatient archives in the US.
Methods: A retrospective cohort study was conducted to identify and analyze hospitalized cases of DILI in adult patients ( > 18 years) using ICD-10 codes from the National Inpatient Sample (NIS) database 2016-2020. We focused on in-hospital outcomes like trends in mortality, length of stay, hospital costs, and complications of DILI using cochran armitage test. We also conducted multivariate regression analysis to find predictors of mortality. Results are presented as adjusted odds ratios with 95% CI using a significant threshold of p< 0.05.
Results: A total of 70,705 hospitalizations were analyzed between 2016 and 2020 (mean age 54.57 years, 52.60% female). Mortality declined significantly from 6.32% in 2016 to 5.75% in 2020 (p < 0.05), though the association was weak (Cramer’s V = 0.017). DILI was linked to an average hospital stay of 7.89 days, with no significant change from 7.35 days in 2016 to 8.72 days in 2020 (p > 0.05). Inflation-adjusted mean hospital charges increased significantly from $19,955 in 2016 to $27,919 in 2020 (p < 0.05).
Predictors of mortality included age > 60 (OR: 1.334, 95% CI: 1.18–1.57, p < 0.05), self-pay as the primary payer (OR: 1.957, 95% CI: 1.67–2.28, p < 0.05), and hospitals in the Northeast (OR: 1.16, 95% CI: 1.05–1.27, p < 0.05). Patient-level predictors included ascites (OR: 1.79, 95% CI: 1.63–1.97, p < 0.05), coagulopathy (OR: 1.25, 95% CI: 1.05–1.49, p < 0.05), SBP (OR: 1.89, 95% CI: 1.56–2.29), jaundice (OR: 1.462, 95% CI: 1.08–1.97), hepatic encephalopathy (OR: 1.42, 95% CI: 1.27–1.60), and HRS (OR: 3.89, 95% CI: 3.47–4.36). Conversely, conditions like CKD (OR: 0.96, 95% CI: 0.88–1.05) and hypoalbuminemia (OR: 0.97, 95% CI: 0.83–1.15) were not significantly associated with increased mortality.
Discussion: We noted a significant decline in mortality rates and increased hospital charges for DILI patients from 2016 to 2020. Mortality was strongly associated with factors such as age > 60, AKI, ascites, and HRS. These findings reveal the burden of DILI on healthcare systems and the importance of early risk stratification and focused intervention in high-risk populations.
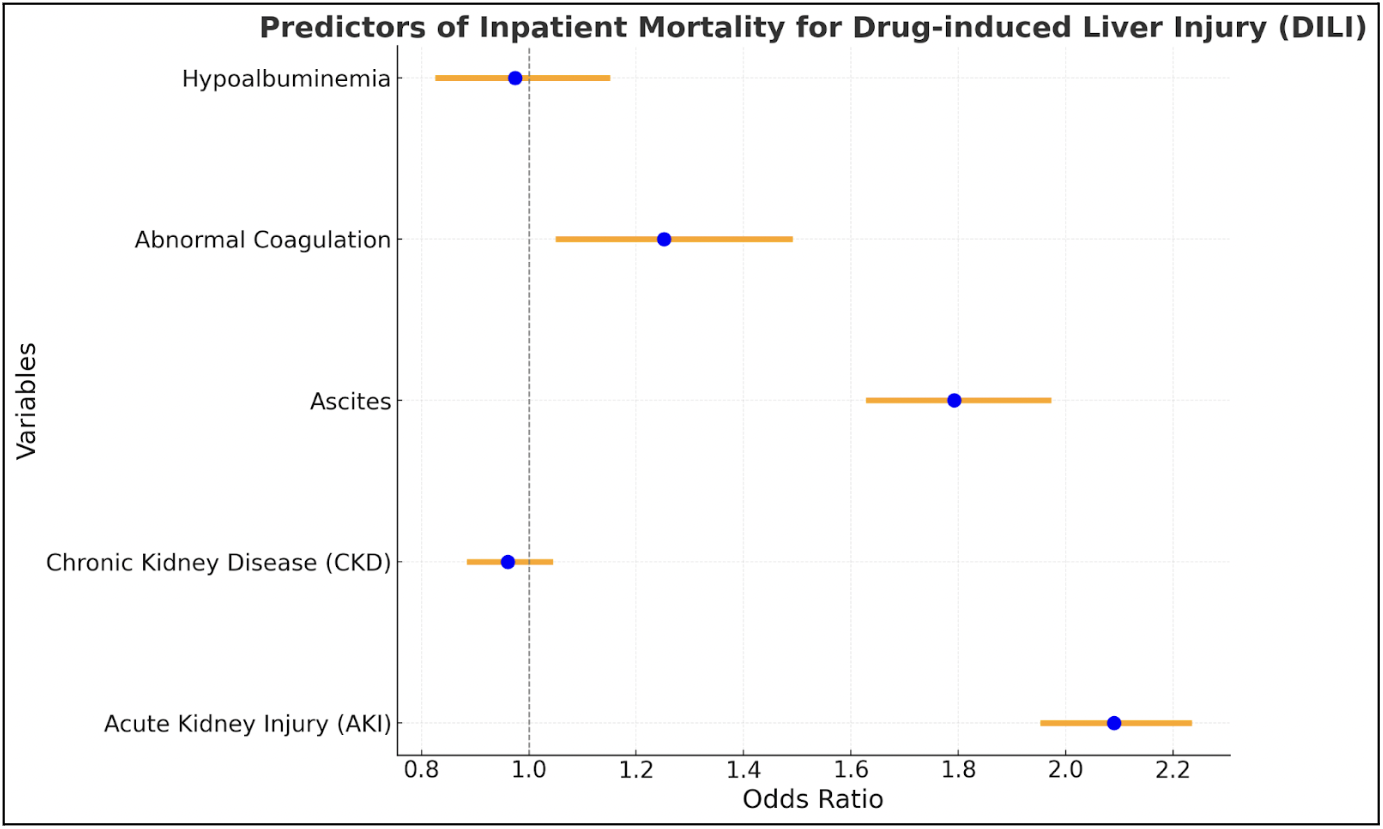
Figure: Yearwise Inpatient Mortality Trends from Drug Induced Liver Injury (DILI)
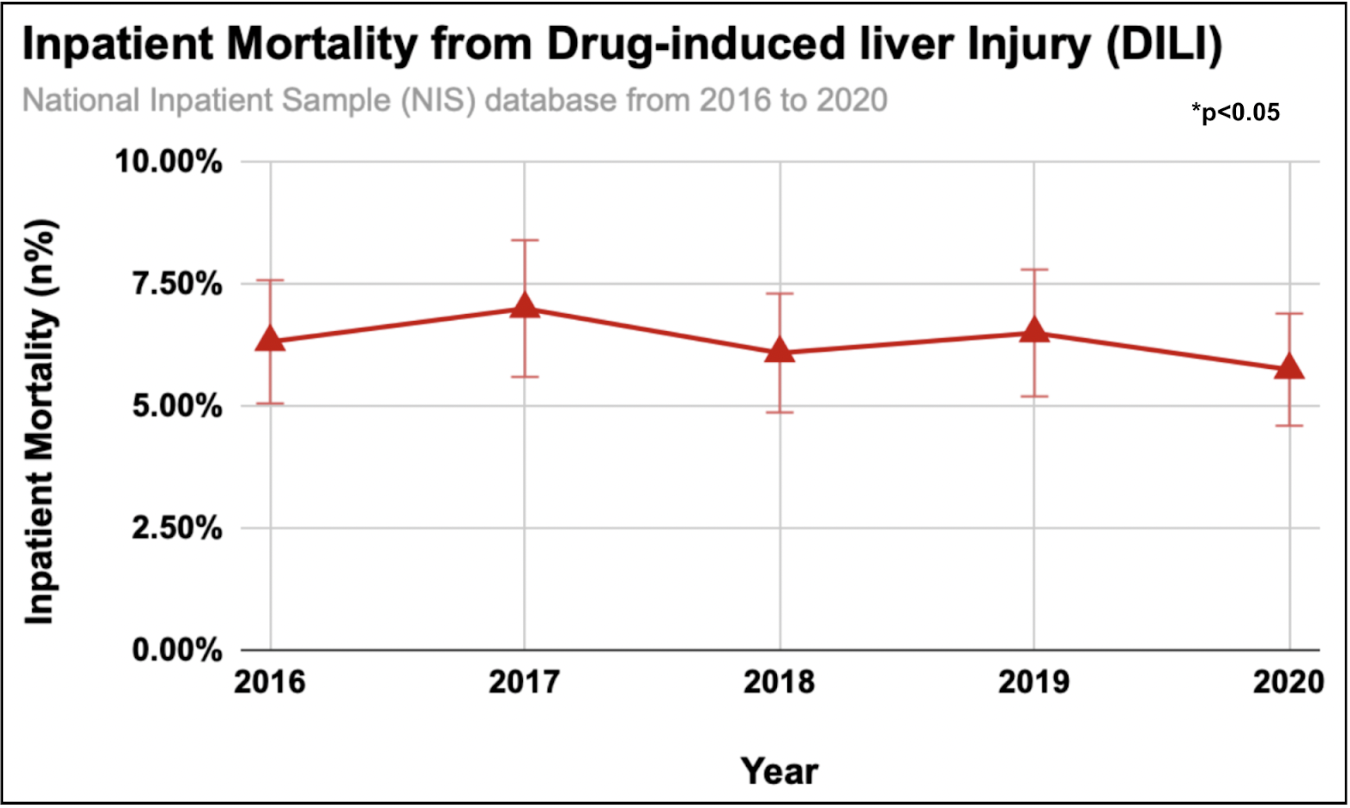
Figure: Predictors of Inpatient Mortality in Drug Induced Liver Injury (DILI)
Disclosures:
Charmy Parikh indicated no relevant financial relationships.
Raj Patel indicated no relevant financial relationships.
Sneh Sonaiya indicated no relevant financial relationships.
Karan Yagnik indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Pranav Patel indicated no relevant financial relationships.
Yash Shah indicated no relevant financial relationships.
Umang Patel indicated no relevant financial relationships.
Steven Russell indicated no relevant financial relationships.
Charmy Parikh, MD1, Raj H. Patel, MD2, Sneh Sonaiya, MD, MPH, MBA3, Karan J.. Yagnik, MD4, Yash Shah, MD5, Pranav Patel, MD6, Yash Shah, MD1, Umang Patel, DO2, Steven Russell, MD1. P5858 - Drug-Induced Liver Injury in Hospitalized Adults: US National Trends, Outcomes and Mortality Predictors, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
