Tuesday Poster Session
Category: Liver
P5840 - POSTER WITHDRAWN
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Taha Shakarchi, MD1, Muhammad Ali Butt, MD1, Ban Al-Abayechi, MD1, Brian Quigley, LICSW1, Kayla Hulburt, LICSW2, Yixin Kong, MBA2, Amir Qamar, MD3, Carmi Punzalan, MD3, Ming V.. Lin, MD3, Han Li, MD3, Mohamed E. Akoad, MD3, Bartholomew J. Kane, MD3, Sarah Meade, MD3, Raza Malik, MD3
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Clinic, Burlington, MA; 3Lahey Hospital and Medical Center, Burlington, MA
Introduction: Alcohol-related liver disease (ALD) is a leading indication for liver transplantation (LT), but post-transplant alcohol relapse remains a significant challenge. Psychosocial vulnerabilities such as anxiety, depression, and poor social support may increase the risk of relapse. Identifying these factors pre-transplant may guide interventions to improve outcomes. This study examined associations between pre-transplant psychosocial characteristics and post-transplant alcohol relapse in patients with ALD.
Methods: A retrospective cohort study was conducted at a single center involving 249 patients who underwent LT for ALD. Patients were categorized based on documented post-transplant alcohol relapse. Pre-transplant psychosocial data included scores from the Generalized Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9), along with demographic and socioeconomic variables such as age, sex, employment status, and support systems. Chi-square tests were used to assess associations between these variables and relapse.
Results: Of 249 patients, 18 (6.8%) experienced alcohol relapse post-transplant. The mean age among relapsers was 51.5 ± 9.3 years, with 50% being female. Severe anxiety (GAD-7 >15) was seen in 30% of relapsers compared to 6% of non-relapsers (p = 0.0371). Mild depression (PHQ-9 score 5–9) was present in 50% of relapsers versus 32% of non-relapsers (p = 0.034). GAD-7 and PHQ-9 scores were unavailable for 8 of the 18 relapsed patients. Unemployment was significantly more common among relapsers than among employed or retired individuals (p = 0.034). Other factors such as insurance status, support systems, and substance use markers showed no significant differences.
Discussion: Pre-transplant symptoms of anxiety and depression, along with unemployment, were significantly associated with post-transplant alcohol relapse in patients with ALD. Routine screening using tools like GAD-7 and PHQ-9 during evaluation may help identify at-risk individuals. Addressing these psychosocial vulnerabilities could reduce relapse rates and improve long-term outcomes after transplantation.
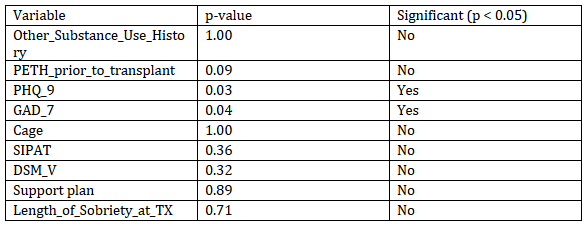
Figure: Table 1
Disclosures:
Taha Shakarchi indicated no relevant financial relationships.
Muhammad Ali Butt indicated no relevant financial relationships.
Ban Al-Abayechi indicated no relevant financial relationships.
Brian Quigley indicated no relevant financial relationships.
Kayla Hulburt indicated no relevant financial relationships.
Yixin Kong indicated no relevant financial relationships.
Amir Qamar indicated no relevant financial relationships.
Carmi Punzalan indicated no relevant financial relationships.
Ming Lin indicated no relevant financial relationships.
Han Li indicated no relevant financial relationships.
Mohamed E. Akoad indicated no relevant financial relationships.
Bartholomew J. Kane indicated no relevant financial relationships.
Sarah Meade indicated no relevant financial relationships.
Raza Malik indicated no relevant financial relationships.
Taha Shakarchi, MD1, Muhammad Ali Butt, MD1, Ban Al-Abayechi, MD1, Brian Quigley, LICSW1, Kayla Hulburt, LICSW2, Yixin Kong, MBA2, Amir Qamar, MD3, Carmi Punzalan, MD3, Ming V.. Lin, MD3, Han Li, MD3, Mohamed E. Akoad, MD3, Bartholomew J. Kane, MD3, Sarah Meade, MD3, Raza Malik, MD3. P5840 - Psychosocial Predictors of Post-Transplant Alcohol Relapse in Patients With Alcohol-Related Liver Disease: A Single-Center Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Beth Israel Lahey Health, Burlington, MA; 2Lahey Clinic, Burlington, MA; 3Lahey Hospital and Medical Center, Burlington, MA
Introduction: Alcohol-related liver disease (ALD) is a leading indication for liver transplantation (LT), but post-transplant alcohol relapse remains a significant challenge. Psychosocial vulnerabilities such as anxiety, depression, and poor social support may increase the risk of relapse. Identifying these factors pre-transplant may guide interventions to improve outcomes. This study examined associations between pre-transplant psychosocial characteristics and post-transplant alcohol relapse in patients with ALD.
Methods: A retrospective cohort study was conducted at a single center involving 249 patients who underwent LT for ALD. Patients were categorized based on documented post-transplant alcohol relapse. Pre-transplant psychosocial data included scores from the Generalized Anxiety Disorder-7 (GAD-7) and Patient Health Questionnaire-9 (PHQ-9), along with demographic and socioeconomic variables such as age, sex, employment status, and support systems. Chi-square tests were used to assess associations between these variables and relapse.
Results: Of 249 patients, 18 (6.8%) experienced alcohol relapse post-transplant. The mean age among relapsers was 51.5 ± 9.3 years, with 50% being female. Severe anxiety (GAD-7 >15) was seen in 30% of relapsers compared to 6% of non-relapsers (p = 0.0371). Mild depression (PHQ-9 score 5–9) was present in 50% of relapsers versus 32% of non-relapsers (p = 0.034). GAD-7 and PHQ-9 scores were unavailable for 8 of the 18 relapsed patients. Unemployment was significantly more common among relapsers than among employed or retired individuals (p = 0.034). Other factors such as insurance status, support systems, and substance use markers showed no significant differences.
Discussion: Pre-transplant symptoms of anxiety and depression, along with unemployment, were significantly associated with post-transplant alcohol relapse in patients with ALD. Routine screening using tools like GAD-7 and PHQ-9 during evaluation may help identify at-risk individuals. Addressing these psychosocial vulnerabilities could reduce relapse rates and improve long-term outcomes after transplantation.
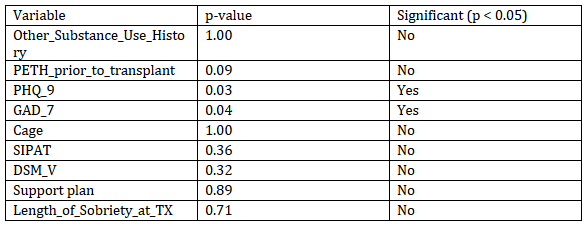
Figure: Table 1
Disclosures:
Taha Shakarchi indicated no relevant financial relationships.
Muhammad Ali Butt indicated no relevant financial relationships.
Ban Al-Abayechi indicated no relevant financial relationships.
Brian Quigley indicated no relevant financial relationships.
Kayla Hulburt indicated no relevant financial relationships.
Yixin Kong indicated no relevant financial relationships.
Amir Qamar indicated no relevant financial relationships.
Carmi Punzalan indicated no relevant financial relationships.
Ming Lin indicated no relevant financial relationships.
Han Li indicated no relevant financial relationships.
Mohamed E. Akoad indicated no relevant financial relationships.
Bartholomew J. Kane indicated no relevant financial relationships.
Sarah Meade indicated no relevant financial relationships.
Raza Malik indicated no relevant financial relationships.
Taha Shakarchi, MD1, Muhammad Ali Butt, MD1, Ban Al-Abayechi, MD1, Brian Quigley, LICSW1, Kayla Hulburt, LICSW2, Yixin Kong, MBA2, Amir Qamar, MD3, Carmi Punzalan, MD3, Ming V.. Lin, MD3, Han Li, MD3, Mohamed E. Akoad, MD3, Bartholomew J. Kane, MD3, Sarah Meade, MD3, Raza Malik, MD3. P5840 - Psychosocial Predictors of Post-Transplant Alcohol Relapse in Patients With Alcohol-Related Liver Disease: A Single-Center Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
