Tuesday Poster Session
Category: Liver
P5836 - Trends and Disparities in Liver Disease and Viral Hepatitis-Related Mortality in Adults ≥ 65 Years From 1999 to 2023 in the United States
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Khizar Hayat, MBBS, MD, BSc (he/him/his)
Waheed Khanzada Medical Center
Lahore, Punjab, Pakistan
Presenting Author(s)
Khizar Hayat, MBBS, MD, BSc1, Anas Nasir, MBBS2, Muhammad Ali, MBBS3, Komal Khalid, MD, MBBS, BSc4, Dania Hussain, MBBS5, Sadia Ghafur, MBBS5, Shaikh Muhammad Daniyal, MBBS6, Saif Ur Rehman, MBBS7, Shireen Asifa, MBBS6, Haider Imran, MBBS8
1Waheed Khanzada Medical Center, Lahore, Punjab, Pakistan; 2Shaikh Zayed Medical College, Lahore, Punjab, Pakistan; 3Dow University of Health Sciences, Sugar Land, TX; 4Hameed Latif Hospital, Lahore, Punjab, Pakistan; 5united medical and dental college, Karachi, Sindh, Pakistan; 6Dow Medical College, Karachi, Sindh, Pakistan; 7bacha khan, Mardan, North-West Frontier, Pakistan; 8Foundation University Medical College, Islamabad, Islamabad, Pakistan
Introduction: Liver disease and viral hepatitis are common, and both are interrelated, and their concurrence is associated with poorer outcomes and accelerated mortality. Research on liver disease and viral hepatitis-related mortality trends stratified by demographic and regional classifications in the United States is limited. This study analyzes national liver disease and viral hepatitis-related mortality trends among adults ≥ 65 years from 1999 to 2023.
Methods: The CDC WONDER Multiple-Cause-of-Death dataset (1999–2023) was used to assess mortality trends among adults ≥ 65 years using ICD-10 codes for liver disease (K70-K76) and viral hepatitis (B15-B19). Data were stratified by year, demographic, and geographic classifications. Age-adjusted mortality rates (AAMR) were calculated per 100,000 persons with 95% confidence intervals (95%CI). Average annual percent change (AAPC) was calculated via the Joinpoint regression model, with statistical significance defined as P < 0.05.
Results: A total of 64,053 liver disease and viral hepatitis-related deaths occurred from 1999 to 2023.
Overall, AAMR remained stable from 5.7 in 1999 to 6.0 in 2023. Men, in comparison to women, had higher average AAMR and had stable rates, while women had declining rates (AAPC: -1.76; 95%CI: -2.96 to -0.54). Racially, non-Hispanic (NH) Asian/Pacific Islanders had the highest average AAMR, and had declining rates along with Hispanic/Latinos (AAPC NH Asian/Pacific Islander: -2.63; 95%CI: -3.68 to -1.56, AAPC Hispanic/Latino: -1.58; 95%CI: -2.60 to -0.55). NH Black/African Americans had increasing rates (AAPC: 1.51; 95%CI: 0.33 to 2.70), while NH Whites saw stable rates. Regionally, the West had the highest average AAMR, and the Northeast had the highest rate of decline (AAPC: -5.70; 95%CI: -8.73 to -2.58). From 1999 to 2020, urban areas, in comparison to rural areas, had higher average AAMR, but rural areas saw increasing rates compared to stable rates for urban areas (AAPC rural areas: 1.76; 95%CI: 0.03 to 3.51).
Discussion: While liver disease and viral hepatitis-related mortality among adults ≥65 years was stable from 1999 to 2023, marked disparities across demographic and geographic groups were noted. These disparities emphasize the urgency for targeted strategies and public health policy changes to decrease mortality rates in at-risk communities.
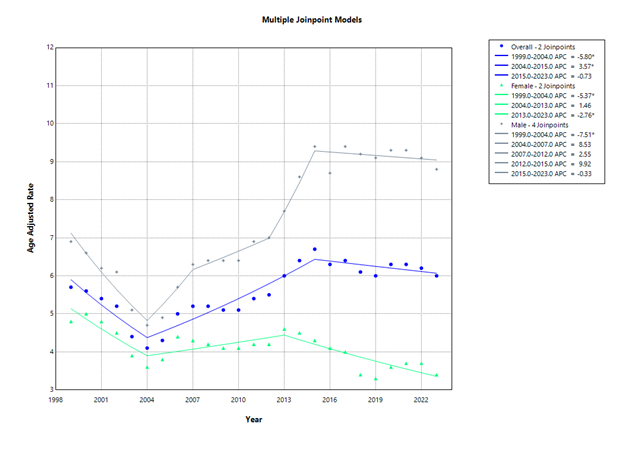
Figure: Multiple Joinpoint Models
Disclosures:
Khizar Hayat indicated no relevant financial relationships.
Anas Nasir indicated no relevant financial relationships.
Muhammad Ali indicated no relevant financial relationships.
Komal Khalid indicated no relevant financial relationships.
Dania Hussain indicated no relevant financial relationships.
Sadia Ghafur indicated no relevant financial relationships.
Shaikh Muhammad Daniyal indicated no relevant financial relationships.
Saif Ur Rehman indicated no relevant financial relationships.
Shireen Asifa indicated no relevant financial relationships.
Haider Imran indicated no relevant financial relationships.
Khizar Hayat, MBBS, MD, BSc1, Anas Nasir, MBBS2, Muhammad Ali, MBBS3, Komal Khalid, MD, MBBS, BSc4, Dania Hussain, MBBS5, Sadia Ghafur, MBBS5, Shaikh Muhammad Daniyal, MBBS6, Saif Ur Rehman, MBBS7, Shireen Asifa, MBBS6, Haider Imran, MBBS8. P5836 - Trends and Disparities in Liver Disease and Viral Hepatitis-Related Mortality in Adults ≥ 65 Years From 1999 to 2023 in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Waheed Khanzada Medical Center, Lahore, Punjab, Pakistan; 2Shaikh Zayed Medical College, Lahore, Punjab, Pakistan; 3Dow University of Health Sciences, Sugar Land, TX; 4Hameed Latif Hospital, Lahore, Punjab, Pakistan; 5united medical and dental college, Karachi, Sindh, Pakistan; 6Dow Medical College, Karachi, Sindh, Pakistan; 7bacha khan, Mardan, North-West Frontier, Pakistan; 8Foundation University Medical College, Islamabad, Islamabad, Pakistan
Introduction: Liver disease and viral hepatitis are common, and both are interrelated, and their concurrence is associated with poorer outcomes and accelerated mortality. Research on liver disease and viral hepatitis-related mortality trends stratified by demographic and regional classifications in the United States is limited. This study analyzes national liver disease and viral hepatitis-related mortality trends among adults ≥ 65 years from 1999 to 2023.
Methods: The CDC WONDER Multiple-Cause-of-Death dataset (1999–2023) was used to assess mortality trends among adults ≥ 65 years using ICD-10 codes for liver disease (K70-K76) and viral hepatitis (B15-B19). Data were stratified by year, demographic, and geographic classifications. Age-adjusted mortality rates (AAMR) were calculated per 100,000 persons with 95% confidence intervals (95%CI). Average annual percent change (AAPC) was calculated via the Joinpoint regression model, with statistical significance defined as P < 0.05.
Results: A total of 64,053 liver disease and viral hepatitis-related deaths occurred from 1999 to 2023.
Overall, AAMR remained stable from 5.7 in 1999 to 6.0 in 2023. Men, in comparison to women, had higher average AAMR and had stable rates, while women had declining rates (AAPC: -1.76; 95%CI: -2.96 to -0.54). Racially, non-Hispanic (NH) Asian/Pacific Islanders had the highest average AAMR, and had declining rates along with Hispanic/Latinos (AAPC NH Asian/Pacific Islander: -2.63; 95%CI: -3.68 to -1.56, AAPC Hispanic/Latino: -1.58; 95%CI: -2.60 to -0.55). NH Black/African Americans had increasing rates (AAPC: 1.51; 95%CI: 0.33 to 2.70), while NH Whites saw stable rates. Regionally, the West had the highest average AAMR, and the Northeast had the highest rate of decline (AAPC: -5.70; 95%CI: -8.73 to -2.58). From 1999 to 2020, urban areas, in comparison to rural areas, had higher average AAMR, but rural areas saw increasing rates compared to stable rates for urban areas (AAPC rural areas: 1.76; 95%CI: 0.03 to 3.51).
Discussion: While liver disease and viral hepatitis-related mortality among adults ≥65 years was stable from 1999 to 2023, marked disparities across demographic and geographic groups were noted. These disparities emphasize the urgency for targeted strategies and public health policy changes to decrease mortality rates in at-risk communities.
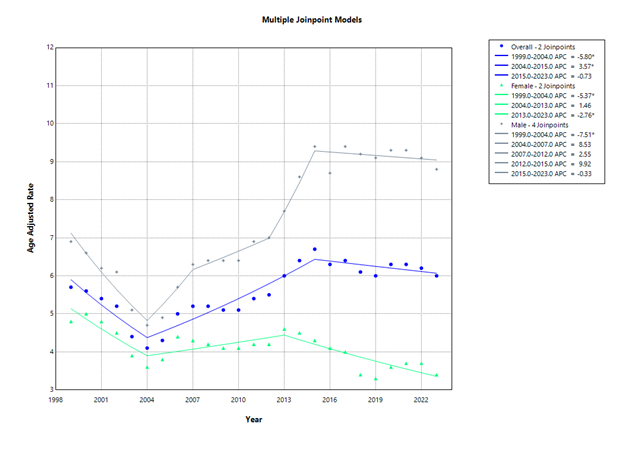
Figure: Multiple Joinpoint Models
Disclosures:
Khizar Hayat indicated no relevant financial relationships.
Anas Nasir indicated no relevant financial relationships.
Muhammad Ali indicated no relevant financial relationships.
Komal Khalid indicated no relevant financial relationships.
Dania Hussain indicated no relevant financial relationships.
Sadia Ghafur indicated no relevant financial relationships.
Shaikh Muhammad Daniyal indicated no relevant financial relationships.
Saif Ur Rehman indicated no relevant financial relationships.
Shireen Asifa indicated no relevant financial relationships.
Haider Imran indicated no relevant financial relationships.
Khizar Hayat, MBBS, MD, BSc1, Anas Nasir, MBBS2, Muhammad Ali, MBBS3, Komal Khalid, MD, MBBS, BSc4, Dania Hussain, MBBS5, Sadia Ghafur, MBBS5, Shaikh Muhammad Daniyal, MBBS6, Saif Ur Rehman, MBBS7, Shireen Asifa, MBBS6, Haider Imran, MBBS8. P5836 - Trends and Disparities in Liver Disease and Viral Hepatitis-Related Mortality in Adults ≥ 65 Years From 1999 to 2023 in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
