Tuesday Poster Session
Category: Liver
P5832 - Hospital Outcomes in Patients With Cirrhosis: An Analysis by Etiology Using 2020 National Inpatient Sample Database
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SH
Seunghee Han, MBChB
MedStar Health
Baltimore, MD
Presenting Author(s)
Seunghee Han, MBChB1, Boniface Mensah, MBChB, MPh2, Simardeep Singh, MBBS2, Ramya Vasireddy, MBBS1, Greeshma Gaddipati, MD1, Rachel Boateng, MD1, Joseph Atarere, MD1, Haider A. Naqvi, MD3, Albert E.. Orhin, MBChB, MHS4, Joo Hee Park, MD5
1MedStar Health, Baltimore, MD; 2MedStar Georgetown University Hospital, Baltimore, MD; 3MedStar Franklin Square Medical Center, Baltimore, MD; 4Ascension Saint Agnes Hospital, Baltimore, MD; 5North Central Bronx Hospital, Bronx, NY
Introduction: Cirrhosis is a major cause of morbidity and mortality worldwide, contributing significantly to hospital admissions and healthcare burden. The etiologies of cirrhosis in these admissions are diverse, with common causes including alcohol-associated liver disease (ALD), chronic hepatitis infections (such as hepatitis B and C), metabolic-dysfunction associated steatohepatitis (MASH), autoimmune conditions, and metabolic disorders. Research has shown that critically ill patients with ALD often experience worse outcomes compared to those with other etiologies of cirrhosis. However, data on the full spectrum of in-hospital outcomes is scarce. This study aims to fill this gap by analyzing the in-hospital outcomes of patients admitted with cirrhosis, stratified by etiology.
Methods: We analyzed 2020 National Inpatient Sample (NIS) data, identifying patients admitted with cirrhosis using ICD-10 codes. Patients were stratified by etiology (ALD, hepatitis B/C, MASLD/MASH, autoimmune, and metabolic disorders). The primary outcome was mortality; secondary outcomes included hospital stay length, death odds, and total charges. Analyses adjusted for demographics and used sampling weights for national estimates.
Results: A total of 148,740 were included in the study. ALD was the most common etiology for cirrhosis (66.5%) and metabolic disorders was the least common cause (0.9%). Our findings indicate that ALD patients have the highest mortality (2.5%), followed by chronic hepatitis infection (1.9%) and MASLD/MASH (1.3%). All other causes of cirrhosis had significantly lower odds of death compared to ALD. Patient with MASLD/MASH and autoimmune conditions had significant shorter length of hospital stay compared to ALD. Total hospital charges were not significantly different across etiologies.
Discussion: The results suggest that cirrhosis etiology plays a critical role in determining patient outcomes during hospitalization. ALD continues to present the most challenging clinical course, with higher mortality and longer hospital stays, likely due to the severity of organ damage and comorbidities associated with alcohol use. On the other hand, MASH/MASLD and Autoimmune conditions associated with cirrhosis tend to have better outcomes, potentially due to earlier detection and more manageable disease progression. Future research to explore long-term outcomes to elucidate the impact of etiology on cirrhosis prognosis and post-hospitalization recovery are needed.
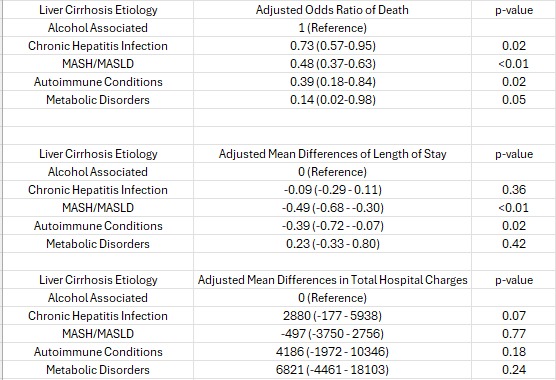
Figure: Analysis of Hospital Outcomes by Liver Cirrhosis Etiology Adjusted for Baseline Characteristics
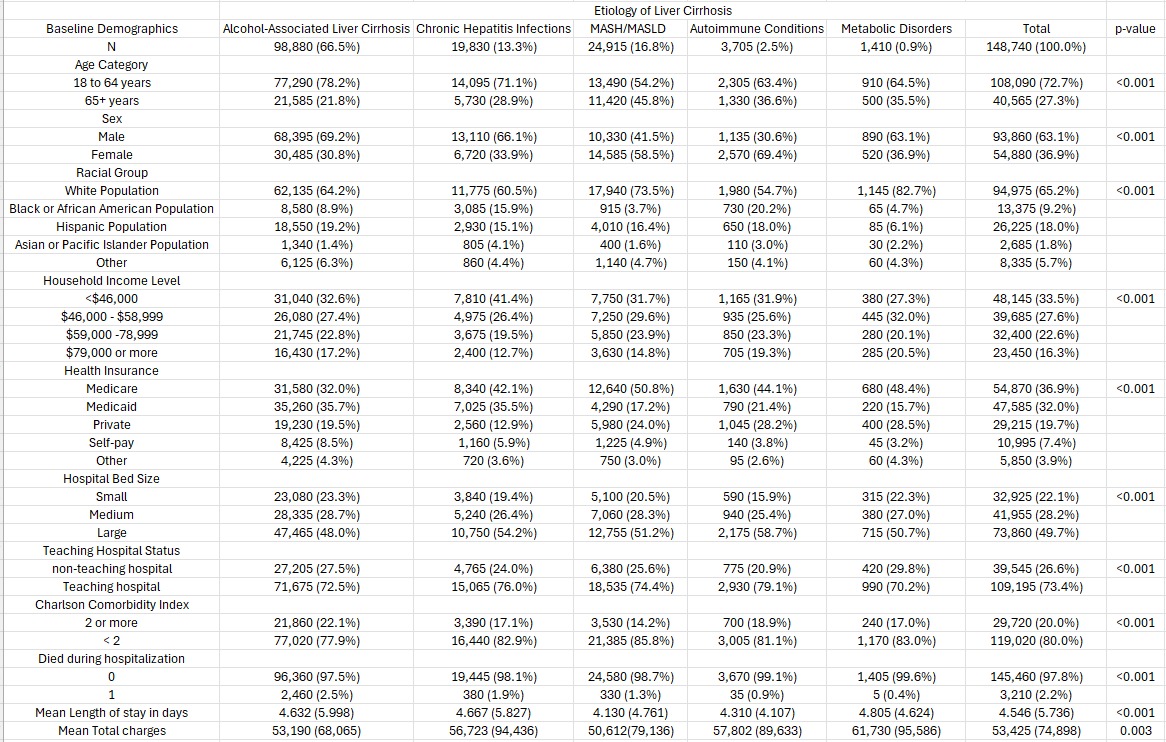
Figure: Baseline Demographics of Study Participants
Disclosures:
Seunghee Han indicated no relevant financial relationships.
Boniface Mensah indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Ramya Vasireddy indicated no relevant financial relationships.
Greeshma Gaddipati indicated no relevant financial relationships.
Rachel Boateng indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Albert Orhin indicated no relevant financial relationships.
Joo Hee Park indicated no relevant financial relationships.
Seunghee Han, MBChB1, Boniface Mensah, MBChB, MPh2, Simardeep Singh, MBBS2, Ramya Vasireddy, MBBS1, Greeshma Gaddipati, MD1, Rachel Boateng, MD1, Joseph Atarere, MD1, Haider A. Naqvi, MD3, Albert E.. Orhin, MBChB, MHS4, Joo Hee Park, MD5. P5832 - Hospital Outcomes in Patients With Cirrhosis: An Analysis by Etiology Using 2020 National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Health, Baltimore, MD; 2MedStar Georgetown University Hospital, Baltimore, MD; 3MedStar Franklin Square Medical Center, Baltimore, MD; 4Ascension Saint Agnes Hospital, Baltimore, MD; 5North Central Bronx Hospital, Bronx, NY
Introduction: Cirrhosis is a major cause of morbidity and mortality worldwide, contributing significantly to hospital admissions and healthcare burden. The etiologies of cirrhosis in these admissions are diverse, with common causes including alcohol-associated liver disease (ALD), chronic hepatitis infections (such as hepatitis B and C), metabolic-dysfunction associated steatohepatitis (MASH), autoimmune conditions, and metabolic disorders. Research has shown that critically ill patients with ALD often experience worse outcomes compared to those with other etiologies of cirrhosis. However, data on the full spectrum of in-hospital outcomes is scarce. This study aims to fill this gap by analyzing the in-hospital outcomes of patients admitted with cirrhosis, stratified by etiology.
Methods: We analyzed 2020 National Inpatient Sample (NIS) data, identifying patients admitted with cirrhosis using ICD-10 codes. Patients were stratified by etiology (ALD, hepatitis B/C, MASLD/MASH, autoimmune, and metabolic disorders). The primary outcome was mortality; secondary outcomes included hospital stay length, death odds, and total charges. Analyses adjusted for demographics and used sampling weights for national estimates.
Results: A total of 148,740 were included in the study. ALD was the most common etiology for cirrhosis (66.5%) and metabolic disorders was the least common cause (0.9%). Our findings indicate that ALD patients have the highest mortality (2.5%), followed by chronic hepatitis infection (1.9%) and MASLD/MASH (1.3%). All other causes of cirrhosis had significantly lower odds of death compared to ALD. Patient with MASLD/MASH and autoimmune conditions had significant shorter length of hospital stay compared to ALD. Total hospital charges were not significantly different across etiologies.
Discussion: The results suggest that cirrhosis etiology plays a critical role in determining patient outcomes during hospitalization. ALD continues to present the most challenging clinical course, with higher mortality and longer hospital stays, likely due to the severity of organ damage and comorbidities associated with alcohol use. On the other hand, MASH/MASLD and Autoimmune conditions associated with cirrhosis tend to have better outcomes, potentially due to earlier detection and more manageable disease progression. Future research to explore long-term outcomes to elucidate the impact of etiology on cirrhosis prognosis and post-hospitalization recovery are needed.
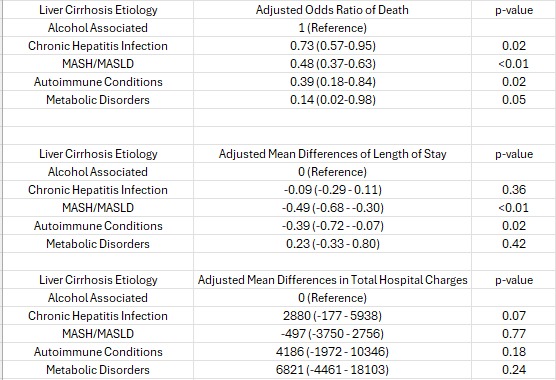
Figure: Analysis of Hospital Outcomes by Liver Cirrhosis Etiology Adjusted for Baseline Characteristics
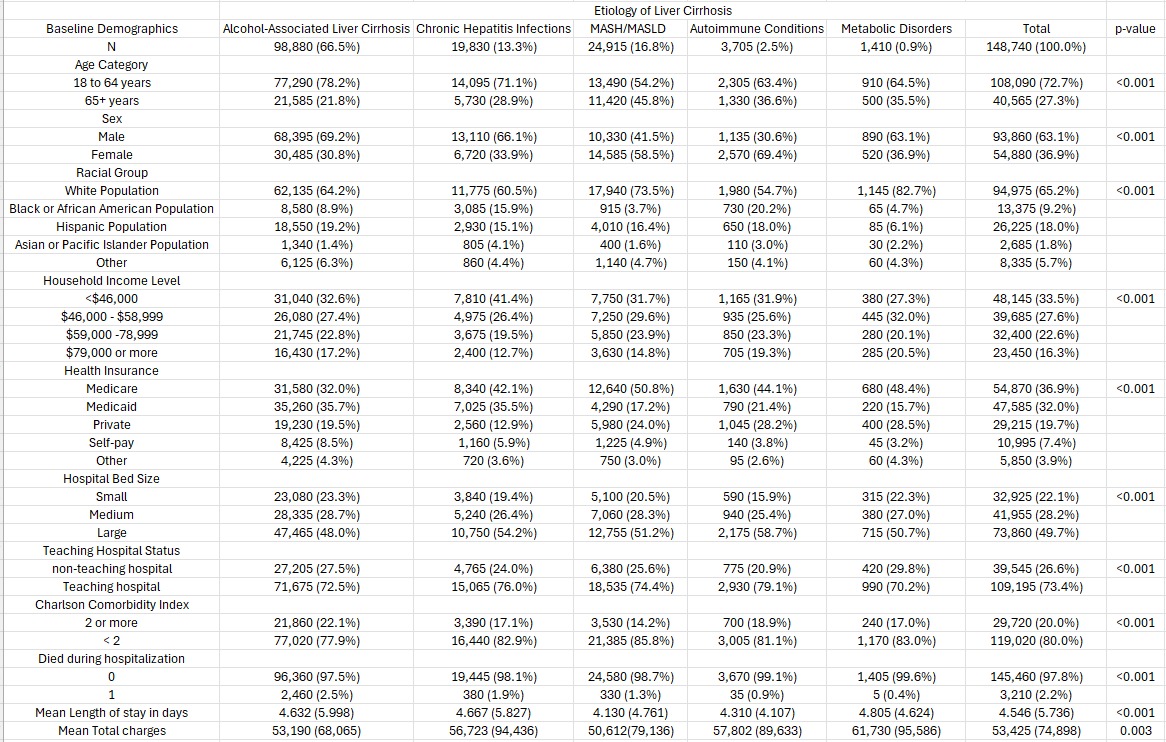
Figure: Baseline Demographics of Study Participants
Disclosures:
Seunghee Han indicated no relevant financial relationships.
Boniface Mensah indicated no relevant financial relationships.
Simardeep Singh indicated no relevant financial relationships.
Ramya Vasireddy indicated no relevant financial relationships.
Greeshma Gaddipati indicated no relevant financial relationships.
Rachel Boateng indicated no relevant financial relationships.
Joseph Atarere indicated no relevant financial relationships.
Haider Naqvi indicated no relevant financial relationships.
Albert Orhin indicated no relevant financial relationships.
Joo Hee Park indicated no relevant financial relationships.
Seunghee Han, MBChB1, Boniface Mensah, MBChB, MPh2, Simardeep Singh, MBBS2, Ramya Vasireddy, MBBS1, Greeshma Gaddipati, MD1, Rachel Boateng, MD1, Joseph Atarere, MD1, Haider A. Naqvi, MD3, Albert E.. Orhin, MBChB, MHS4, Joo Hee Park, MD5. P5832 - Hospital Outcomes in Patients With Cirrhosis: An Analysis by Etiology Using 2020 National Inpatient Sample Database, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
