Tuesday Poster Session
Category: Liver
P5801 - Beyond the Virus: Unveiling the Real-World Mortality Burden of Viral Hepatitis Using CDC WONDER Large Database (1999-2023)
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- RA
Rehmat ullah Awan, MD
West Virginia University
Morgantown, WV
Presenting Author(s)
Fatima Shahid, MBBS1, Saleha Azeem, MBBS1, Muhammad Ayyan, MBBS2, Afra Zahid, MBBS1, Kebire Gofar, 3, Ambreen Nabeel, MBBS4, Rehmat Ullah Awan, MD4, Khalid Mumtaz, MBBS, MSc5
1Department of Medicine, King Edward Medical University, Lahore, Pakistan, Lahore, Punjab, Pakistan; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3The Ohio State University, Columbus, OH; 4West Virginia University, Morgantown, WV; 5The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Viral hepatitis remains a significant public health challenge worldwide, contributing substantially to liver-related morbidity and mortality in the United States. However, the real-world mortality burden of viral hepatitis is often underestimated due to under-reporting and mis-classification errors on death certificates.
Methods: Mortality data from 1999 to 2023 were extracted from the CDC WONDER database. Deaths with ICD-10 codes B15-B19 (viral hepatitis) listed as a multiple cause of death were included. Crude and age-adjusted mortality rates (AAMR) per 100,000 populations were calculated. Joinpoint regression analysis was used to estimate annual percent change (APC) and average annual percent change (AAPC) with 95% confidence intervals (CIs).
Results: From 1999-2020, a total of 359,715 deaths were attributed to viral hepatitis. The AAMR itself increased from 3.41 in 1999 to 3.89 in 2020 (AAPC: 0.15, 95% CI: -0.37 to 0.69). The AAMR was significantly higher in males than females (7.00 vs 2.69). Moreover, females had a decreasing trend in mortality (AAPC: -0.32, 95% CI: -0.92 to 0.28) and males had an increasing trend (AAPC: 0.31, 95% CI: -0.20 to 0.83). The crude mortality rate was highest in 55-64 years’ age group (17.90). Among the different ethnic groups, American Indian or Alaska Natives had the highest AAMR (9.26) and the White had the lowest AAMR (4.05). The Hispanic demonstrated the highest decrease in mortality (AAPC: -2.29, 95% CI: -4.11 to -0.45). Geographically, the West had the highest AAMR (6.71) but an overall decreasing mortality trend (AAPC: -0.26, 95% CI: -0.97 to 0.44) and the Northeast had the highest decrease in mortality (AAPC: -1.78, 95% CI: -2.54 to -1.02). Among the states, District of Columbia had the highest AAMR i.e. 12.15 and Wisconsin had the lowest i.e. 2.27. The AAMR was comparable in metropolitan and non-metropolitan regions (4.85 and 4.31), however, over the years, the mortality rate decreased in the metropolitan areas (AAPC: -0.18, 95% CI: -0.71 to 0.34) and increased in non-metropolitan areas (AAPC: 2.24, 95% CI: 1.56 to 2.93). The highest percentage of deaths were reported in inpatient-medical facility (48.66%).
Discussion: Viral hepatitis-related mortality has steadily increased over the past two decades, with striking increases in males, 55-64 years of age individuals, American Indians or Alaska Natives, the West, and in rural areas which highlight the need for targeted intervention.
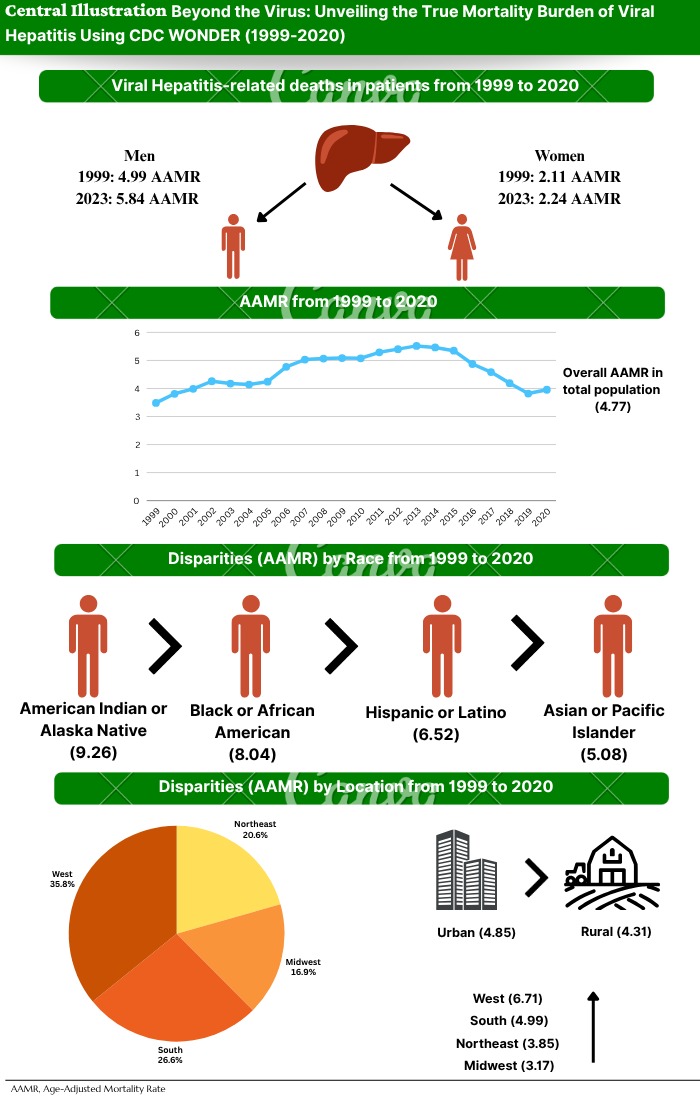
Figure: Mortality Data
Disclosures:
Fatima Shahid indicated no relevant financial relationships.
Saleha Azeem indicated no relevant financial relationships.
Muhammad Ayyan indicated no relevant financial relationships.
Afra Zahid indicated no relevant financial relationships.
Kebire Gofar indicated no relevant financial relationships.
Ambreen Nabeel indicated no relevant financial relationships.
Rehmat Ullah Awan indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Fatima Shahid, MBBS1, Saleha Azeem, MBBS1, Muhammad Ayyan, MBBS2, Afra Zahid, MBBS1, Kebire Gofar, 3, Ambreen Nabeel, MBBS4, Rehmat Ullah Awan, MD4, Khalid Mumtaz, MBBS, MSc5. P5801 - Beyond the Virus: Unveiling the Real-World Mortality Burden of Viral Hepatitis Using CDC WONDER Large Database (1999-2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Medicine, King Edward Medical University, Lahore, Pakistan, Lahore, Punjab, Pakistan; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3The Ohio State University, Columbus, OH; 4West Virginia University, Morgantown, WV; 5The Ohio State University Wexner Medical Center, Columbus, OH
Introduction: Viral hepatitis remains a significant public health challenge worldwide, contributing substantially to liver-related morbidity and mortality in the United States. However, the real-world mortality burden of viral hepatitis is often underestimated due to under-reporting and mis-classification errors on death certificates.
Methods: Mortality data from 1999 to 2023 were extracted from the CDC WONDER database. Deaths with ICD-10 codes B15-B19 (viral hepatitis) listed as a multiple cause of death were included. Crude and age-adjusted mortality rates (AAMR) per 100,000 populations were calculated. Joinpoint regression analysis was used to estimate annual percent change (APC) and average annual percent change (AAPC) with 95% confidence intervals (CIs).
Results: From 1999-2020, a total of 359,715 deaths were attributed to viral hepatitis. The AAMR itself increased from 3.41 in 1999 to 3.89 in 2020 (AAPC: 0.15, 95% CI: -0.37 to 0.69). The AAMR was significantly higher in males than females (7.00 vs 2.69). Moreover, females had a decreasing trend in mortality (AAPC: -0.32, 95% CI: -0.92 to 0.28) and males had an increasing trend (AAPC: 0.31, 95% CI: -0.20 to 0.83). The crude mortality rate was highest in 55-64 years’ age group (17.90). Among the different ethnic groups, American Indian or Alaska Natives had the highest AAMR (9.26) and the White had the lowest AAMR (4.05). The Hispanic demonstrated the highest decrease in mortality (AAPC: -2.29, 95% CI: -4.11 to -0.45). Geographically, the West had the highest AAMR (6.71) but an overall decreasing mortality trend (AAPC: -0.26, 95% CI: -0.97 to 0.44) and the Northeast had the highest decrease in mortality (AAPC: -1.78, 95% CI: -2.54 to -1.02). Among the states, District of Columbia had the highest AAMR i.e. 12.15 and Wisconsin had the lowest i.e. 2.27. The AAMR was comparable in metropolitan and non-metropolitan regions (4.85 and 4.31), however, over the years, the mortality rate decreased in the metropolitan areas (AAPC: -0.18, 95% CI: -0.71 to 0.34) and increased in non-metropolitan areas (AAPC: 2.24, 95% CI: 1.56 to 2.93). The highest percentage of deaths were reported in inpatient-medical facility (48.66%).
Discussion: Viral hepatitis-related mortality has steadily increased over the past two decades, with striking increases in males, 55-64 years of age individuals, American Indians or Alaska Natives, the West, and in rural areas which highlight the need for targeted intervention.
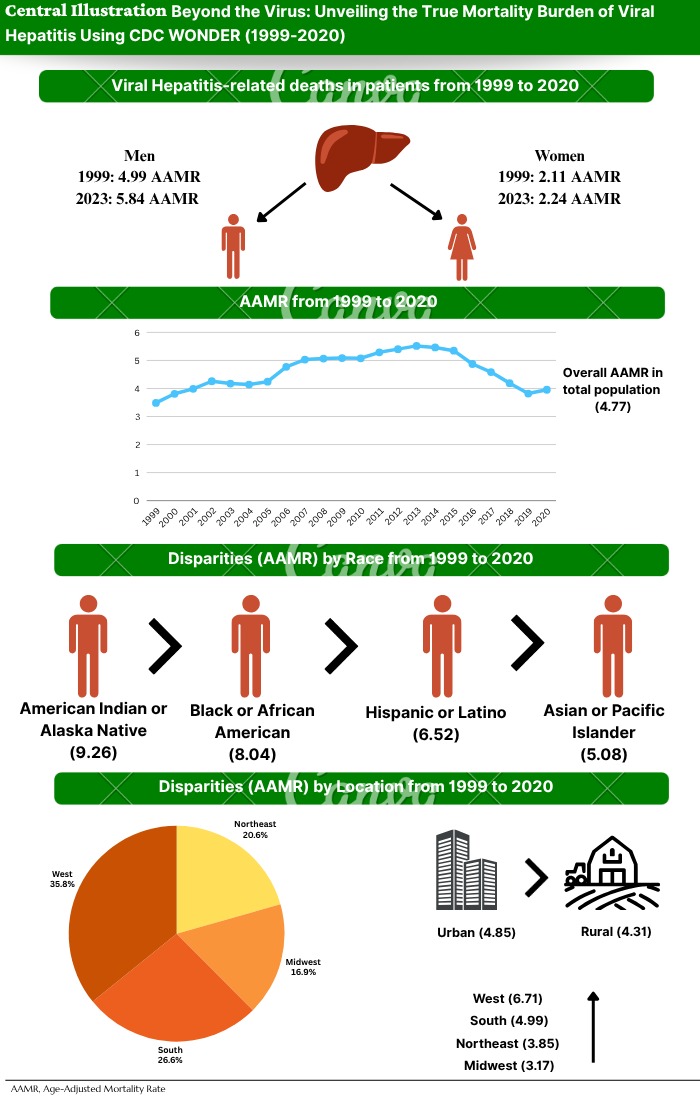
Figure: Mortality Data
Disclosures:
Fatima Shahid indicated no relevant financial relationships.
Saleha Azeem indicated no relevant financial relationships.
Muhammad Ayyan indicated no relevant financial relationships.
Afra Zahid indicated no relevant financial relationships.
Kebire Gofar indicated no relevant financial relationships.
Ambreen Nabeel indicated no relevant financial relationships.
Rehmat Ullah Awan indicated no relevant financial relationships.
Khalid Mumtaz indicated no relevant financial relationships.
Fatima Shahid, MBBS1, Saleha Azeem, MBBS1, Muhammad Ayyan, MBBS2, Afra Zahid, MBBS1, Kebire Gofar, 3, Ambreen Nabeel, MBBS4, Rehmat Ullah Awan, MD4, Khalid Mumtaz, MBBS, MSc5. P5801 - Beyond the Virus: Unveiling the Real-World Mortality Burden of Viral Hepatitis Using CDC WONDER Large Database (1999-2023), ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
