Tuesday Poster Session
Category: Liver
P5797 - Global Burden of Acute Hepatitis B From 1990 to 2021: A Joinpoint Analysis Across Socio-Demographic Index Levels
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Osama Alshakhatreh, MD (he/him/his)
Albany Medical Center
Norfolk, VA
Presenting Author(s)
Osama Alshakhatreh, MD, Ibrahim Mohammed, MD, Tarick Ahmad, BS, Shunsa Tarar, DO, Seth Richter, MD, FACG
Albany Medical Center, Albany, NY
Introduction: Acute hepatitis B (AHB) remains a pressing global health challenge, particularly in low-income regions lacking universal vaccination and access to treatment. In contrast, high- and middle-SDI regions have reduced AHB incidence and mortality through birth-dose vaccination, perinatal prevention, and stronger health systems. This study analyzes Global Burden of Disease (GBD) data using Joinpoint regression to identify shifts in AHB trends across SDI levels.
Methods: We used GBD database estimates for age-standardized incidence, prevalence, and mortality rates of AHB from 1990 to 2021, stratified by SDI (high, middle, low). Trends were analyzed using the Joinpoint Regression Program v5.4.0 to identify inflection points in disease burden over time.
Results: From 1990 to 2021, ASIR declined across all SDI groups, most in middle (–51.5%) and high (–49.5%) SDI regions, and least in low SDI (–24.4%). Low SDI had the highest incidence throughout. Joinpoint analysis showed steady declines in middle/high SDI; low SDI remained stable until 2001 (APC –0.08%, p< 0.05), then declined.
ASPR followed a similar pattern, with low SDI showing smaller reductions (–24.1%) and a delayed decline after 2003 (APC –1.39%, p< 0.05).
ASMR decreased in all SDI groups. Mortality rose in low SDI until 1999, then dropped sharply (APC –4.90%, p< 0.05); AAPC –3.4 (95% CI: –3.6 to –3.2; p< 0.0001). Middle/high SDI declined faster early, then slowed over the past decade (APC –1.91% and –2.84%; p< 0.05).
Trends differed significantly across SDI groups for all three measures when assessed for parallelism (p< 0.05).
Discussion: Low SDI countries continue to carry the highest burden of acute hepatitis B across incidence, prevalence, and mortality. While declines since 1990 were smallest in this group, later-onset downward trends suggest they are in a catch-up phase. The more pronounced declines in mortality compared to incidence may reflect improvements in treatment access, but the slower decline in incidence highlights gaps in prevention and broader disparities in social determinants of health. These findings call for focused efforts to enhance vaccination, screening, and health infrastructure in low SDI regions.
The observed non-parallel trends across SDI categories reinforce persistent structural inequities in public health infrastructure, access to care, and the delivery of preventive services.
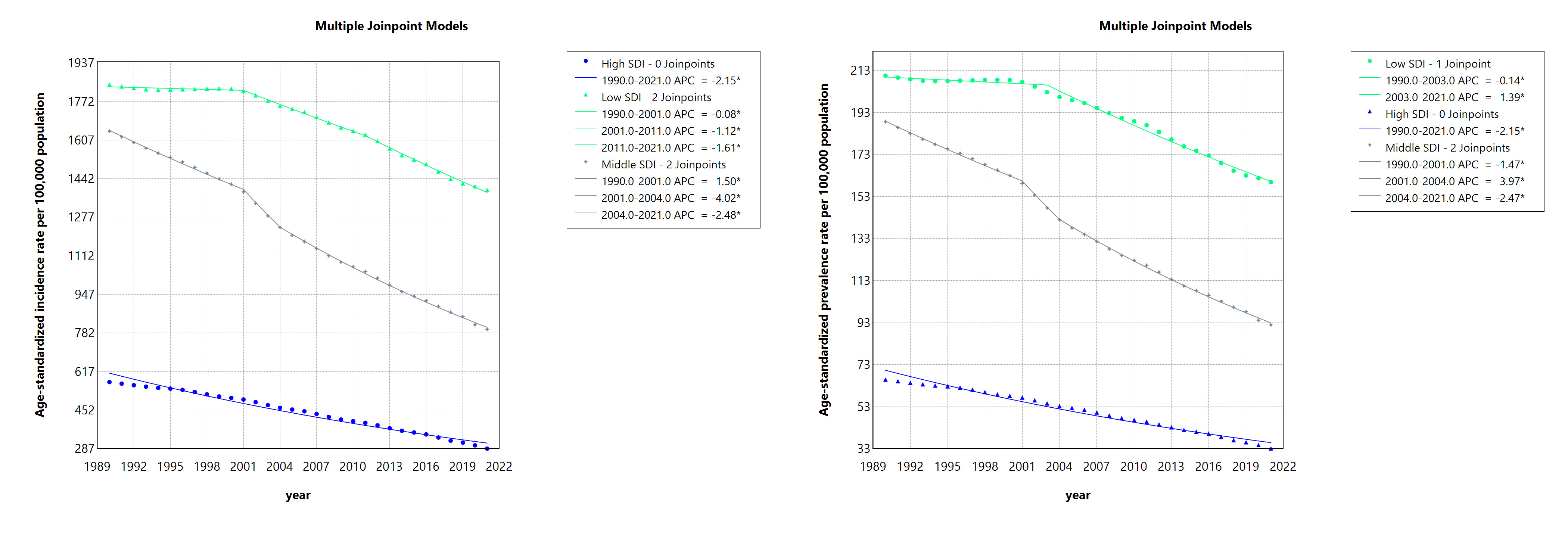
Figure: Figure 1. Trends in age-standardized incidence and prevalence rates of acute hepatitis B from 1990 to 2021 by Socio-Demographic Index
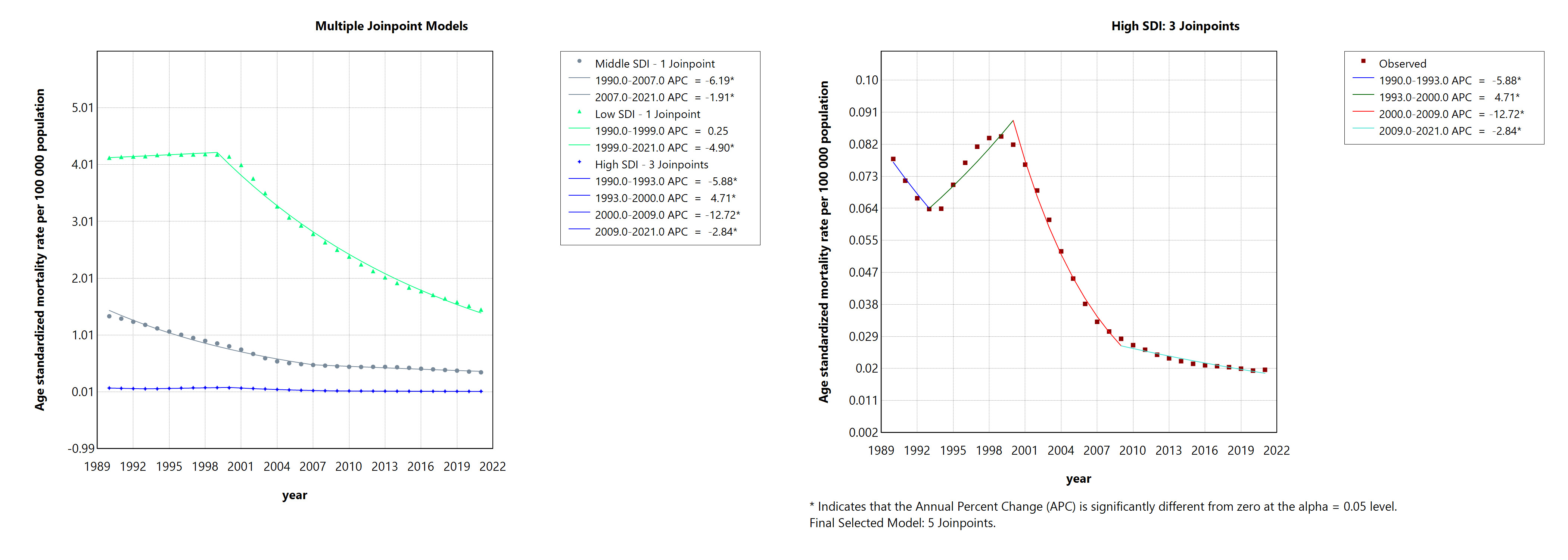
Figure: Figure 2. Mortality trends for acute hepatitis B (1990–2021) by SDI. High SDI is shown separately due to minimal change relative to other groups.
Disclosures:
Osama Alshakhatreh indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Tarick Ahmad indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Osama Alshakhatreh, MD, Ibrahim Mohammed, MD, Tarick Ahmad, BS, Shunsa Tarar, DO, Seth Richter, MD, FACG. P5797 - Global Burden of Acute Hepatitis B From 1990 to 2021: A Joinpoint Analysis Across Socio-Demographic Index Levels, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Albany Medical Center, Albany, NY
Introduction: Acute hepatitis B (AHB) remains a pressing global health challenge, particularly in low-income regions lacking universal vaccination and access to treatment. In contrast, high- and middle-SDI regions have reduced AHB incidence and mortality through birth-dose vaccination, perinatal prevention, and stronger health systems. This study analyzes Global Burden of Disease (GBD) data using Joinpoint regression to identify shifts in AHB trends across SDI levels.
Methods: We used GBD database estimates for age-standardized incidence, prevalence, and mortality rates of AHB from 1990 to 2021, stratified by SDI (high, middle, low). Trends were analyzed using the Joinpoint Regression Program v5.4.0 to identify inflection points in disease burden over time.
Results: From 1990 to 2021, ASIR declined across all SDI groups, most in middle (–51.5%) and high (–49.5%) SDI regions, and least in low SDI (–24.4%). Low SDI had the highest incidence throughout. Joinpoint analysis showed steady declines in middle/high SDI; low SDI remained stable until 2001 (APC –0.08%, p< 0.05), then declined.
ASPR followed a similar pattern, with low SDI showing smaller reductions (–24.1%) and a delayed decline after 2003 (APC –1.39%, p< 0.05).
ASMR decreased in all SDI groups. Mortality rose in low SDI until 1999, then dropped sharply (APC –4.90%, p< 0.05); AAPC –3.4 (95% CI: –3.6 to –3.2; p< 0.0001). Middle/high SDI declined faster early, then slowed over the past decade (APC –1.91% and –2.84%; p< 0.05).
Trends differed significantly across SDI groups for all three measures when assessed for parallelism (p< 0.05).
Discussion: Low SDI countries continue to carry the highest burden of acute hepatitis B across incidence, prevalence, and mortality. While declines since 1990 were smallest in this group, later-onset downward trends suggest they are in a catch-up phase. The more pronounced declines in mortality compared to incidence may reflect improvements in treatment access, but the slower decline in incidence highlights gaps in prevention and broader disparities in social determinants of health. These findings call for focused efforts to enhance vaccination, screening, and health infrastructure in low SDI regions.
The observed non-parallel trends across SDI categories reinforce persistent structural inequities in public health infrastructure, access to care, and the delivery of preventive services.
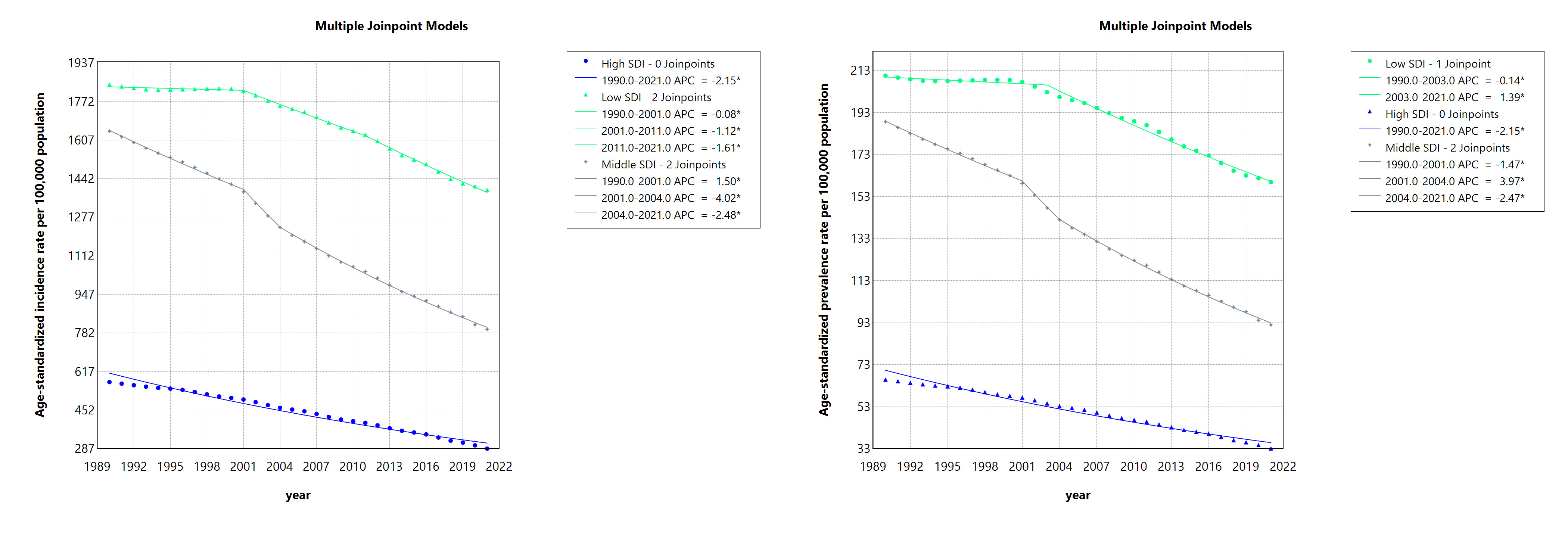
Figure: Figure 1. Trends in age-standardized incidence and prevalence rates of acute hepatitis B from 1990 to 2021 by Socio-Demographic Index
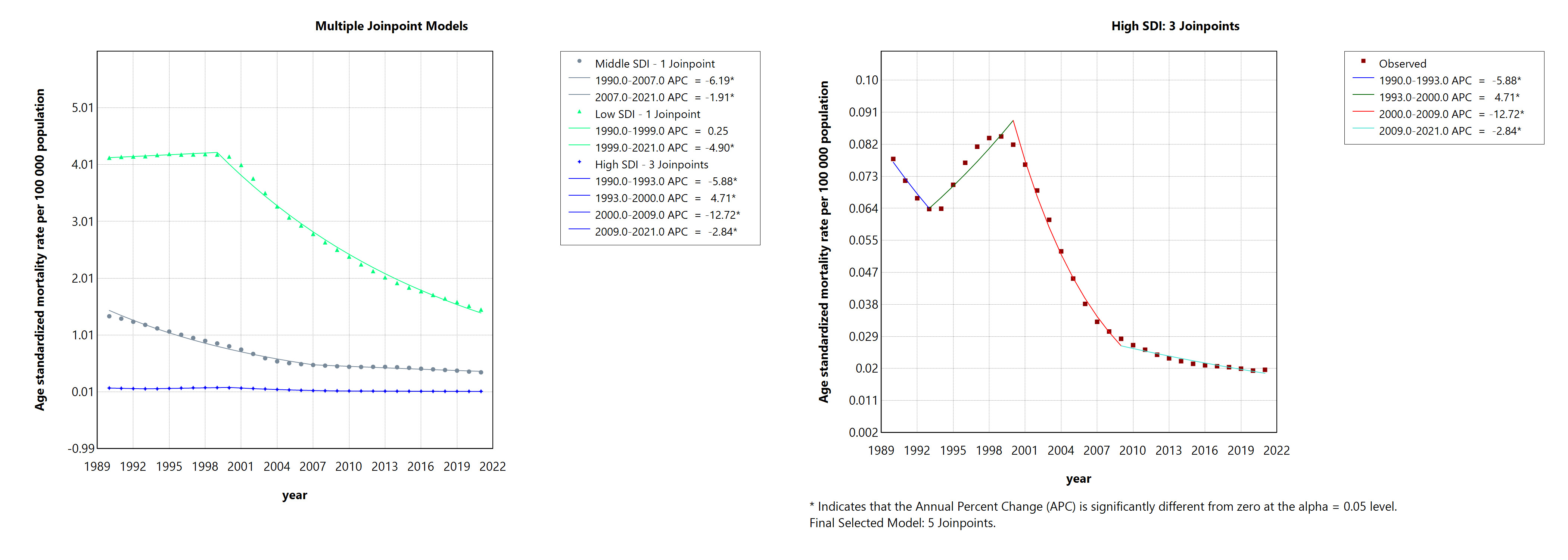
Figure: Figure 2. Mortality trends for acute hepatitis B (1990–2021) by SDI. High SDI is shown separately due to minimal change relative to other groups.
Disclosures:
Osama Alshakhatreh indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Tarick Ahmad indicated no relevant financial relationships.
Shunsa Tarar indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Osama Alshakhatreh, MD, Ibrahim Mohammed, MD, Tarick Ahmad, BS, Shunsa Tarar, DO, Seth Richter, MD, FACG. P5797 - Global Burden of Acute Hepatitis B From 1990 to 2021: A Joinpoint Analysis Across Socio-Demographic Index Levels, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
