Tuesday Poster Session
Category: Liver
P5792 - Impact of Hospital Size on Outcomes and Resource Utilization Following Transjugular Intrahepatic Portosystemic Shunt (TIPS): A 7-Year Retrospective Analysis in the United States
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Omar Alkasabrah, MD (he/him/his)
Landmark Medical Center
Woonsocket, RI
Presenting Author(s)
Omar Alkasabrah, MD1, Abdullah Hafeez, MD1, Ritu C. Tated, MBBS, MPH2, Siddharth Agrawal, MD1, Mutaz Kalas, MD3, Radhe Shah, MD4, Mostafa Eysha, MD3, Muhammad Qasim Chaudhry, MD1, Faiza Jajja, MD1, Jatin Thukral, MD1, Tanuj Sharma, MD1
1Landmark Medical Center, Woonsocket, RI; 2New York Medical College, Valhalla, NY; 3Texas Tech University Health Science Center El Paso, El Paso, TX; 4Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Hospital size may influence outcomes and resource use in complex procedures like TIPS, yet its role remains unclear.
Methods: Adult TIPS procedures (2016–2022) were identified in the National Inpatient Sample. Hospitals were stratified by size (small, medium, large) per AHRQ definitions. Patient and hospital characteristics were compared. Multivariable regression assessed associations between hospital size and in-hospital mortality, complications, length of stay (LOS), and total hospital charges (TOTCHG), adjusting for demographics, comorbidities, and hospital factors.
Results: Among 163,135 TIPS patients, 21.3% were treated at small, 32.3% at medium, and 46.4% at large hospitals. Compared to medium and large hospitals, small hospital TAVR admissions were more likely to have female sex, white race, and Medicare/Medicaid payer (Table). Crude mortality increased with hospital size (small: 2.6%, medium: 3.2%, large: 3.5%; p< 0.001). On adjusted analysis, large hospitals had significantly higher odds of mortality (aOR 1.13; 95% CI: 1.09–1.17; p< 0.001). Large hospital size was also associated with increased odds of bleeding (aOR 1.40), AKI (aOR 1.19), and DVT (aOR 1.46) (all p< 0.001). LOS increased with hospital size (small: 5.0±0.06 days; large: 6.26±0.05; p< 0.001), as did TOTCHG (small: $62,997; large: $95,587; p< 0.001).
Discussion: These results suggest that TIPS procedures performed at large hospitals are associated with higher in-hospital mortality, complication rates, and healthcare costs. This may reflect greater case complexity at tertiary centers and underscores the importance of improved risk adjustment and resource allocation in TIPS care. Importantly, the findings also highlight that small hospitals are performing well in delivering safe and effective TIPS outcomes. Further studies are warranted to understand the drivers of these disparities and inform system-level improvements.
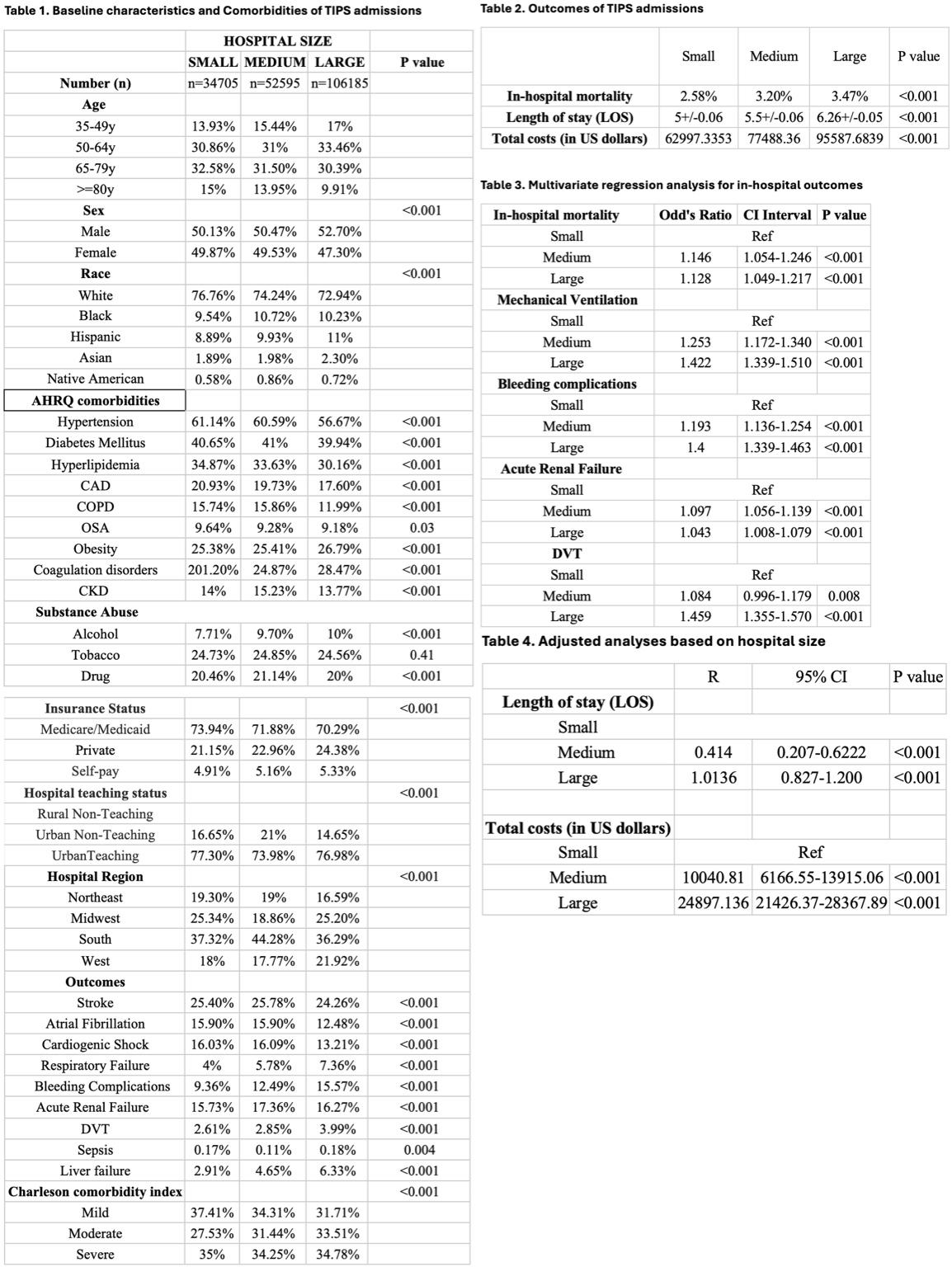
Figure: Summary of baseline characteristics, in-hospital outcomes, and adjusted analyses by hospital size among patients undergoing TIPS (2016–2022).
Disclosures:
Omar Alkasabrah indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Ritu C. Tated indicated no relevant financial relationships.
Siddharth Agrawal indicated no relevant financial relationships.
Mutaz Kalas indicated no relevant financial relationships.
Radhe Shah indicated no relevant financial relationships.
Mostafa Eysha indicated no relevant financial relationships.
Muhammad Qasim Chaudhry indicated no relevant financial relationships.
Faiza Jajja indicated no relevant financial relationships.
Jatin Thukral indicated no relevant financial relationships.
Tanuj Sharma indicated no relevant financial relationships.
Omar Alkasabrah, MD1, Abdullah Hafeez, MD1, Ritu C. Tated, MBBS, MPH2, Siddharth Agrawal, MD1, Mutaz Kalas, MD3, Radhe Shah, MD4, Mostafa Eysha, MD3, Muhammad Qasim Chaudhry, MD1, Faiza Jajja, MD1, Jatin Thukral, MD1, Tanuj Sharma, MD1. P5792 - Impact of Hospital Size on Outcomes and Resource Utilization Following Transjugular Intrahepatic Portosystemic Shunt (TIPS): A 7-Year Retrospective Analysis in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Landmark Medical Center, Woonsocket, RI; 2New York Medical College, Valhalla, NY; 3Texas Tech University Health Science Center El Paso, El Paso, TX; 4Beth Israel Deaconess Medical Center, Harvard Medical School, Boston, MA
Introduction: Hospital size may influence outcomes and resource use in complex procedures like TIPS, yet its role remains unclear.
Methods: Adult TIPS procedures (2016–2022) were identified in the National Inpatient Sample. Hospitals were stratified by size (small, medium, large) per AHRQ definitions. Patient and hospital characteristics were compared. Multivariable regression assessed associations between hospital size and in-hospital mortality, complications, length of stay (LOS), and total hospital charges (TOTCHG), adjusting for demographics, comorbidities, and hospital factors.
Results: Among 163,135 TIPS patients, 21.3% were treated at small, 32.3% at medium, and 46.4% at large hospitals. Compared to medium and large hospitals, small hospital TAVR admissions were more likely to have female sex, white race, and Medicare/Medicaid payer (Table). Crude mortality increased with hospital size (small: 2.6%, medium: 3.2%, large: 3.5%; p< 0.001). On adjusted analysis, large hospitals had significantly higher odds of mortality (aOR 1.13; 95% CI: 1.09–1.17; p< 0.001). Large hospital size was also associated with increased odds of bleeding (aOR 1.40), AKI (aOR 1.19), and DVT (aOR 1.46) (all p< 0.001). LOS increased with hospital size (small: 5.0±0.06 days; large: 6.26±0.05; p< 0.001), as did TOTCHG (small: $62,997; large: $95,587; p< 0.001).
Discussion: These results suggest that TIPS procedures performed at large hospitals are associated with higher in-hospital mortality, complication rates, and healthcare costs. This may reflect greater case complexity at tertiary centers and underscores the importance of improved risk adjustment and resource allocation in TIPS care. Importantly, the findings also highlight that small hospitals are performing well in delivering safe and effective TIPS outcomes. Further studies are warranted to understand the drivers of these disparities and inform system-level improvements.
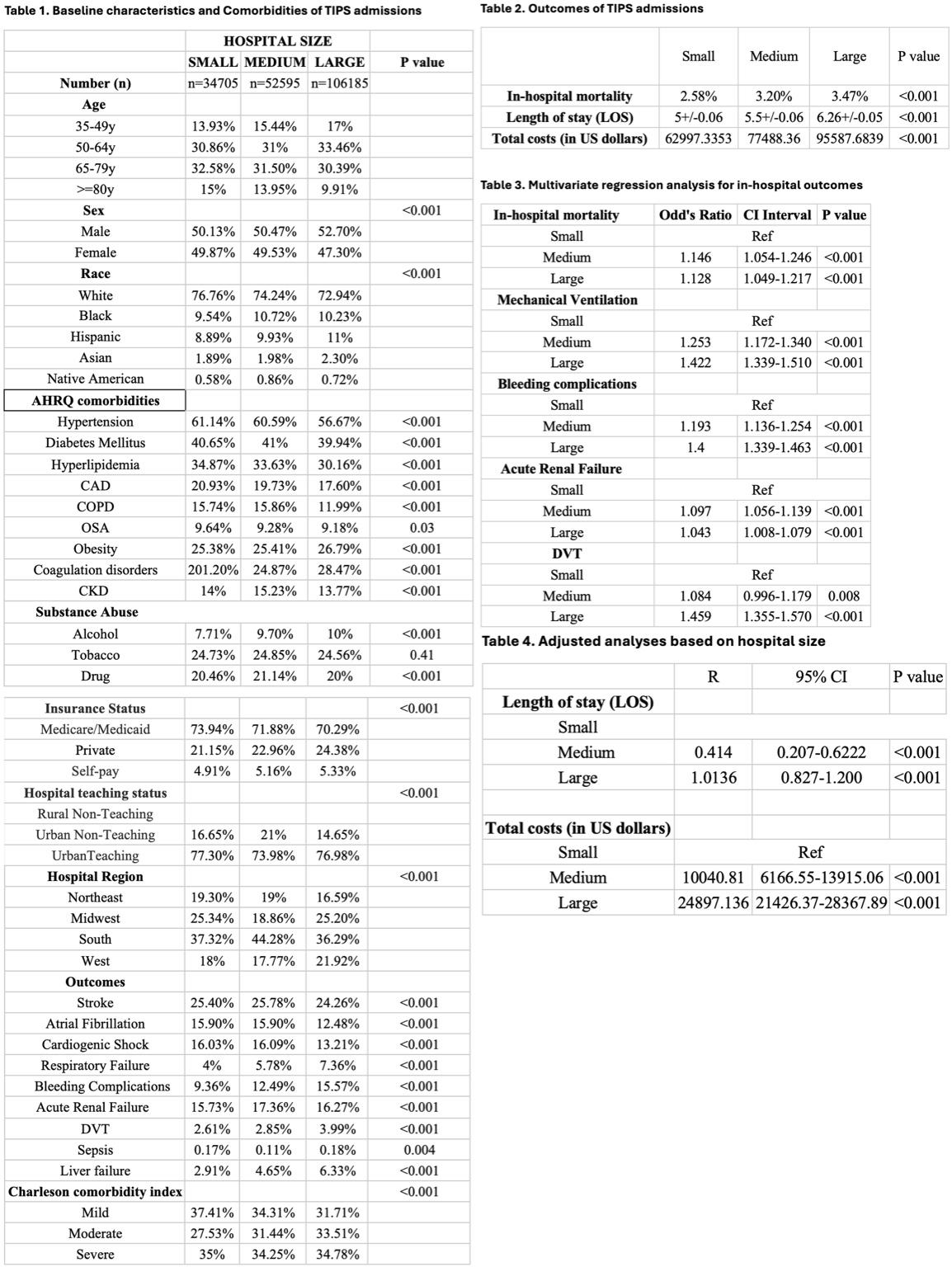
Figure: Summary of baseline characteristics, in-hospital outcomes, and adjusted analyses by hospital size among patients undergoing TIPS (2016–2022).
Disclosures:
Omar Alkasabrah indicated no relevant financial relationships.
Abdullah Hafeez indicated no relevant financial relationships.
Ritu C. Tated indicated no relevant financial relationships.
Siddharth Agrawal indicated no relevant financial relationships.
Mutaz Kalas indicated no relevant financial relationships.
Radhe Shah indicated no relevant financial relationships.
Mostafa Eysha indicated no relevant financial relationships.
Muhammad Qasim Chaudhry indicated no relevant financial relationships.
Faiza Jajja indicated no relevant financial relationships.
Jatin Thukral indicated no relevant financial relationships.
Tanuj Sharma indicated no relevant financial relationships.
Omar Alkasabrah, MD1, Abdullah Hafeez, MD1, Ritu C. Tated, MBBS, MPH2, Siddharth Agrawal, MD1, Mutaz Kalas, MD3, Radhe Shah, MD4, Mostafa Eysha, MD3, Muhammad Qasim Chaudhry, MD1, Faiza Jajja, MD1, Jatin Thukral, MD1, Tanuj Sharma, MD1. P5792 - Impact of Hospital Size on Outcomes and Resource Utilization Following Transjugular Intrahepatic Portosystemic Shunt (TIPS): A 7-Year Retrospective Analysis in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
