Tuesday Poster Session
Category: Liver
P5784 - Racial Disparities in Vaccine-Preventable Infections and Outcomes in Chronic Liver Disease: A National Perspective
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Bright Nwatamole, MBBS (he/him/his)
Vassar Brothers Medical Center - Nuvance Health
Poughkeepsie, NY
Presenting Author(s)
Bright Nwatamole, MBBS1, Adedeji Adenusi, MD, MPH2, Emeka Stanley. Obi, MBBS, MPH3, Nzubechukwu Stanley. Okeke, MBBS4, Ibukunoluwa Oshobu, MD5
1Vassar Brothers Medical Center - Nuvance Health, Poughkeepsie, NY; 2One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 3Brookdale University Hospital Medical Center, Brokelyne, NY; 4Nuvance Health, Poughkeepsie, NY; 5University of Missouri, Missouri, MO
Introduction: Chronic liver disease (CLD) patients are at high risk for severe outcomes from vaccine-preventable infections (VPIs) due to immune dysfunction and comorbidities. Despite established vaccination guidelines, racial disparities in VPI incidence and outcomes in CLD remain underexplored. This study aims to evaluate racial differences in the incidence of VPIs and associated outcomes in hospitalized CLD patients in the United States.
Methods: We conducted a retrospective cohort study using the 2016–2020 National Inpatient Sample (NIS) to identify adult patients hospitalized with CLD. VPIs included influenza, pneumococcal, hepatitis A, hepatitis B, and COVID-19 infections. Primary outcomes were in-hospital mortality and prolonged length of stay ( >7 days). Multivariable survey-weighted logistic regression models were used to assess the impact of race and VPIs on outcomes, adjusting for demographics, comorbidities, hospital characteristics, and illness severity.
Results: Among 21,410 hospitalized CLD patients, the mean age was 60 years, with the majority being White (67.1%), followed by Hispanic (17.9%), Black (11.7%), and Asian (3.3%). Mortality rates varied significantly by race, with Black patients having a 67% higher odds of in-hospital mortality compared to White patients (aOR 1.67, 95% CI 1.23-2.28, p=0.0012), while Asians had more than double the risk (aOR 2.27, 95% CI 1.20-4.29, p=0.0116). Hispanic patients showed a non-significant trend toward lower mortality risk (aOR 0.72, 95% CI 0.52-1.01, p=0.0573). COVID-19 infection significantly increased mortality (aOR 2.42, 95% CI 1.49-3.92, p=0.0003), while hepatitis B was associated with prolonged hospitalization (aOR 2.85, 95% CI 1.56-5.21, p=0.0007). Income level also influenced mortality, with the lowest income quartile having a more than twofold increased risk compared to the highest quartile (aOR 2.14, 95% CI 1.38-3.31, p=0.0007).
Discussion: Significant racial disparities exist in the outcomes of hospitalized CLD patients with VPIs, with Black and Asian patients experiencing substantially higher mortality. These findings highlight the need for targeted public health interventions to address racial inequities in vaccination and chronic liver disease management, particularly in the context of COVID-19. Future efforts should focus on reducing these disparities through improved vaccination rates and tailored healthcare strategies.
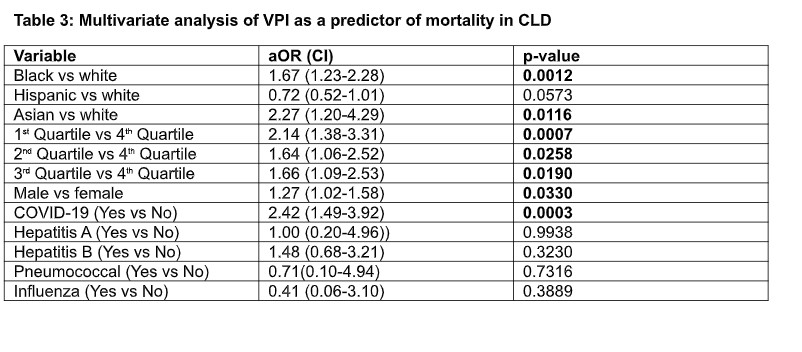
Figure: Table 3: Multivariate analysis of VPI as a predictor of mortality in CLD
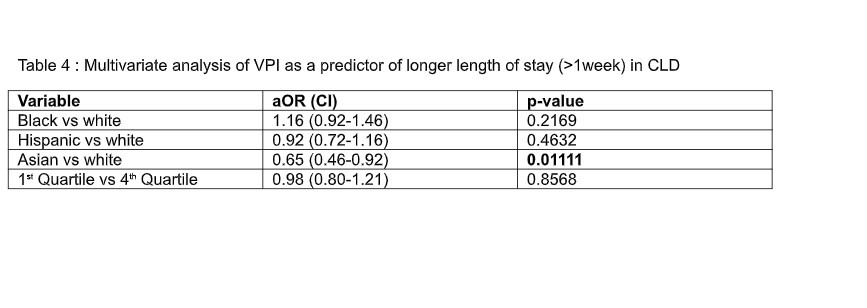
Figure: Table 4: Multivariate analysis of VPI as a predictor of longer length of stay (>1week) in CLD
Disclosures:
Bright Nwatamole indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Emeka Obi indicated no relevant financial relationships.
Nzubechukwu Okeke indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Bright Nwatamole, MBBS1, Adedeji Adenusi, MD, MPH2, Emeka Stanley. Obi, MBBS, MPH3, Nzubechukwu Stanley. Okeke, MBBS4, Ibukunoluwa Oshobu, MD5. P5784 - Racial Disparities in Vaccine-Preventable Infections and Outcomes in Chronic Liver Disease: A National Perspective, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Vassar Brothers Medical Center - Nuvance Health, Poughkeepsie, NY; 2One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 3Brookdale University Hospital Medical Center, Brokelyne, NY; 4Nuvance Health, Poughkeepsie, NY; 5University of Missouri, Missouri, MO
Introduction: Chronic liver disease (CLD) patients are at high risk for severe outcomes from vaccine-preventable infections (VPIs) due to immune dysfunction and comorbidities. Despite established vaccination guidelines, racial disparities in VPI incidence and outcomes in CLD remain underexplored. This study aims to evaluate racial differences in the incidence of VPIs and associated outcomes in hospitalized CLD patients in the United States.
Methods: We conducted a retrospective cohort study using the 2016–2020 National Inpatient Sample (NIS) to identify adult patients hospitalized with CLD. VPIs included influenza, pneumococcal, hepatitis A, hepatitis B, and COVID-19 infections. Primary outcomes were in-hospital mortality and prolonged length of stay ( >7 days). Multivariable survey-weighted logistic regression models were used to assess the impact of race and VPIs on outcomes, adjusting for demographics, comorbidities, hospital characteristics, and illness severity.
Results: Among 21,410 hospitalized CLD patients, the mean age was 60 years, with the majority being White (67.1%), followed by Hispanic (17.9%), Black (11.7%), and Asian (3.3%). Mortality rates varied significantly by race, with Black patients having a 67% higher odds of in-hospital mortality compared to White patients (aOR 1.67, 95% CI 1.23-2.28, p=0.0012), while Asians had more than double the risk (aOR 2.27, 95% CI 1.20-4.29, p=0.0116). Hispanic patients showed a non-significant trend toward lower mortality risk (aOR 0.72, 95% CI 0.52-1.01, p=0.0573). COVID-19 infection significantly increased mortality (aOR 2.42, 95% CI 1.49-3.92, p=0.0003), while hepatitis B was associated with prolonged hospitalization (aOR 2.85, 95% CI 1.56-5.21, p=0.0007). Income level also influenced mortality, with the lowest income quartile having a more than twofold increased risk compared to the highest quartile (aOR 2.14, 95% CI 1.38-3.31, p=0.0007).
Discussion: Significant racial disparities exist in the outcomes of hospitalized CLD patients with VPIs, with Black and Asian patients experiencing substantially higher mortality. These findings highlight the need for targeted public health interventions to address racial inequities in vaccination and chronic liver disease management, particularly in the context of COVID-19. Future efforts should focus on reducing these disparities through improved vaccination rates and tailored healthcare strategies.
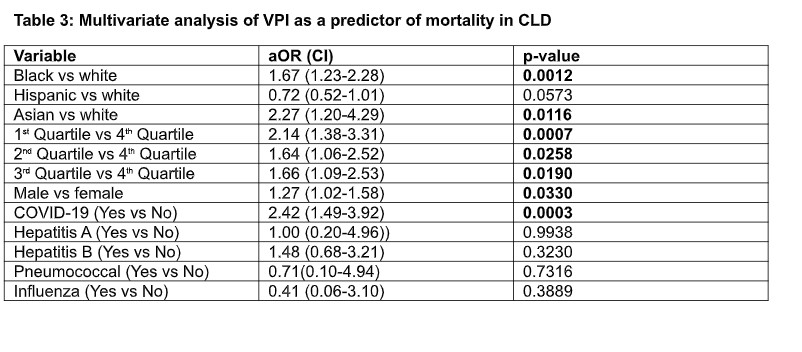
Figure: Table 3: Multivariate analysis of VPI as a predictor of mortality in CLD
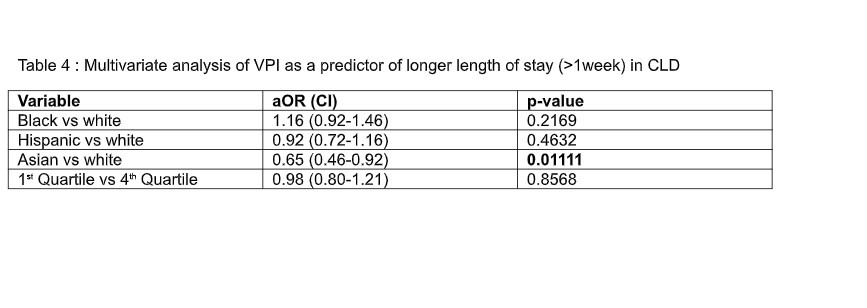
Figure: Table 4: Multivariate analysis of VPI as a predictor of longer length of stay (>1week) in CLD
Disclosures:
Bright Nwatamole indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Emeka Obi indicated no relevant financial relationships.
Nzubechukwu Okeke indicated no relevant financial relationships.
Ibukunoluwa Oshobu indicated no relevant financial relationships.
Bright Nwatamole, MBBS1, Adedeji Adenusi, MD, MPH2, Emeka Stanley. Obi, MBBS, MPH3, Nzubechukwu Stanley. Okeke, MBBS4, Ibukunoluwa Oshobu, MD5. P5784 - Racial Disparities in Vaccine-Preventable Infections and Outcomes in Chronic Liver Disease: A National Perspective, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
