Tuesday Poster Session
Category: Liver
P5770 - Limited Hepatology Care for High-Risk Cirrhosis Patients in a Health System That Utilizes Two Electronic Medical Records
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdelrhman Refaey, MD
Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences
Teaneck, NJ
Presenting Author(s)
Abdelrhman Refaey, MD1, Ahmed Ebeid, MD2, Puja Sasankan, BS3, Ahmed Attia, MD2, Mohamed Abdou, MD2, Asil Alsaad, MD2, Ameer Abutaleb, MD4
1Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 2Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 3George Washington University School of Medicine and Health Sciences, Washington, DC; 4The George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC
Introduction: In current practice, patients with MELD scores >15 are referred for liver transplant evaluation. In April 2022, our health system started hepatology clinics and liver transplant services. Presently, these services use an electronic medical record system that is distinct from the one used in the outpatient group practice. Our study’s aim was to analyze linkage to care for hepatology services within this dynamic.
Methods: We retrospectively reviewed patient records, including inpatient and outpatient notes, from January 2022 to April 2024. We included any patient with an ICD-10 diagnosis code related to cirrhosis or portal hypertension and aged between 18 and 91 years old through an electronic algorithm. Patients with a history of hepatocellular carcinoma or underwent liver transplant were excluded from the analysis. We collected basic demographic data and the most recent clinical lab values to characterize liver disease burden and calculate a MELD 3.0 score.
Results: A total of 1,786 patients were retrieved from records, with 848 having lab values for MELD 3.0. Of those, 59.6% had a MELD 3.0 >15 (n = 505). The average age was 61. Of those with a MELD 3.0 >15, 60.8% were males (n = 307), and 39.2% were females (n = 198). 50.3% were African Americans (n = 254), 28.1% were White (n = 142), 20.6% self-identified as Multiple/Other (n = 104), and 1.6% Asian (n = 8). 84.4% were inpatient visits (n = 426) and 15.6% were outpatient (n = 79). 67.1% lacked a primary care physician (n = 339). Overall, 49.1% with a MELD 3.0 > 15 did not receive a hepatology referral (n = 248). 81% of those were from inpatient visits (n = 201). 56% were males (n = 140) and 44% were females (n = 109). 30.6% were African Americans (n = 76), 13.7% White (n = 34), 11.3% Multiple/Other (n = 28), and 1.2% Asian (n = 3).
Discussion: Among 848 patients with MELD 3.0 scores, 59.6% (n = 505) had scores greater than 15. Despite this, 49.1% (n = 248) did not receive referrals for outpatient hepatology care. This issue is exacerbated by 67.1% (n = 339) of patients lacking a primary care physician. Further research is needed to develop mechanisms through the electronic medical record systems that achieve adequate linkage to care in this patient population.
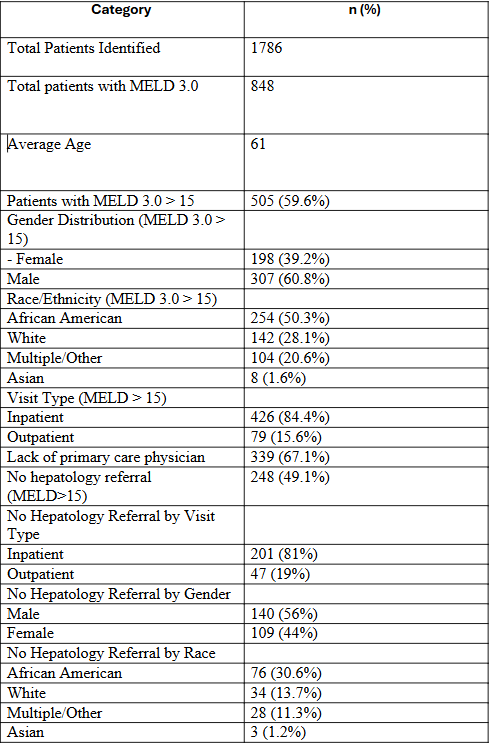
Figure: A table summerizing the main results
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Ahmed Ebeid indicated no relevant financial relationships.
Puja Sasankan indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Mohamed Abdou indicated no relevant financial relationships.
Asil Alsaad indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Abdelrhman Refaey, MD1, Ahmed Ebeid, MD2, Puja Sasankan, BS3, Ahmed Attia, MD2, Mohamed Abdou, MD2, Asil Alsaad, MD2, Ameer Abutaleb, MD4. P5770 - Limited Hepatology Care for High-Risk Cirrhosis Patients in a Health System That Utilizes Two Electronic Medical Records, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Division of Gastroenterology and Liver Disease, Department of Medicine, George Washington University School of Medicine and Health Sciences, Washington, DC; 2Transplant Institute, Department of Surgery, George Washington University School of Medicine and Health Science, Washington, DC; 3George Washington University School of Medicine and Health Sciences, Washington, DC; 4The George Washington Transplant Institute, Department of Surgery, The George Washington University Hospital, Washington, DC
Introduction: In current practice, patients with MELD scores >15 are referred for liver transplant evaluation. In April 2022, our health system started hepatology clinics and liver transplant services. Presently, these services use an electronic medical record system that is distinct from the one used in the outpatient group practice. Our study’s aim was to analyze linkage to care for hepatology services within this dynamic.
Methods: We retrospectively reviewed patient records, including inpatient and outpatient notes, from January 2022 to April 2024. We included any patient with an ICD-10 diagnosis code related to cirrhosis or portal hypertension and aged between 18 and 91 years old through an electronic algorithm. Patients with a history of hepatocellular carcinoma or underwent liver transplant were excluded from the analysis. We collected basic demographic data and the most recent clinical lab values to characterize liver disease burden and calculate a MELD 3.0 score.
Results: A total of 1,786 patients were retrieved from records, with 848 having lab values for MELD 3.0. Of those, 59.6% had a MELD 3.0 >15 (n = 505). The average age was 61. Of those with a MELD 3.0 >15, 60.8% were males (n = 307), and 39.2% were females (n = 198). 50.3% were African Americans (n = 254), 28.1% were White (n = 142), 20.6% self-identified as Multiple/Other (n = 104), and 1.6% Asian (n = 8). 84.4% were inpatient visits (n = 426) and 15.6% were outpatient (n = 79). 67.1% lacked a primary care physician (n = 339). Overall, 49.1% with a MELD 3.0 > 15 did not receive a hepatology referral (n = 248). 81% of those were from inpatient visits (n = 201). 56% were males (n = 140) and 44% were females (n = 109). 30.6% were African Americans (n = 76), 13.7% White (n = 34), 11.3% Multiple/Other (n = 28), and 1.2% Asian (n = 3).
Discussion: Among 848 patients with MELD 3.0 scores, 59.6% (n = 505) had scores greater than 15. Despite this, 49.1% (n = 248) did not receive referrals for outpatient hepatology care. This issue is exacerbated by 67.1% (n = 339) of patients lacking a primary care physician. Further research is needed to develop mechanisms through the electronic medical record systems that achieve adequate linkage to care in this patient population.
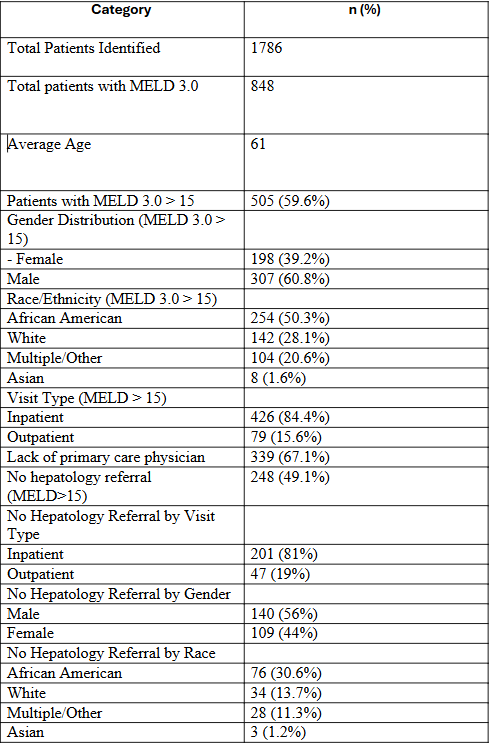
Figure: A table summerizing the main results
Disclosures:
Abdelrhman Refaey indicated no relevant financial relationships.
Ahmed Ebeid indicated no relevant financial relationships.
Puja Sasankan indicated no relevant financial relationships.
Ahmed Attia indicated no relevant financial relationships.
Mohamed Abdou indicated no relevant financial relationships.
Asil Alsaad indicated no relevant financial relationships.
Ameer Abutaleb indicated no relevant financial relationships.
Abdelrhman Refaey, MD1, Ahmed Ebeid, MD2, Puja Sasankan, BS3, Ahmed Attia, MD2, Mohamed Abdou, MD2, Asil Alsaad, MD2, Ameer Abutaleb, MD4. P5770 - Limited Hepatology Care for High-Risk Cirrhosis Patients in a Health System That Utilizes Two Electronic Medical Records, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
