Tuesday Poster Session
Category: Liver
P5766 - The Impact of MASLD on All-Cause Mortality Among Elevated Cardiovascular Risk Patients: A Propensity Score-Matched Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Iyad Al-Bustami, MD, MPH (he/him/his)
Brooklyn Hospital Center
Brooklyn, NY
Presenting Author(s)
Iyad Al-Bustami, MD, MPH1, Sweta Lohani, MD1, Chaula Desai, MD1, Kenan Alrejjal, MBBS2, Kazi Haque, MD3, Ammar Yasser. Abdulfattah, MBBCh4, Abbas H. Mallick, MD5, Delwar Khan, MD1, Rasha Hamid Numan Saleh, 6, Muhammad Desouky, MD7, Daniel Low, MD8, Jamil Shah, MD1
1Brooklyn Hospital Center, Brooklyn, NY; 2MedStar Georgetown/Washington Hospital Center, Washington, DC; 3University of Texas Health, McGovern Medical School, Houston, TX; 4SUNY Downstate Medical Center, Brooklyn, NY; 5The Brooklyn Hospital Center, New York, NY; 6MD, Brooklyn, NY; 7The Brooklyn Hospital Center, Brooklyn, NY; 8University of Toronto, Toronto, ON, Canada
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) significantly contributes to cardiovascular risks, but its precise impact within populations already at elevated cardiovascular risk remains insufficiently studied.
Methods: This retrospective, propensity score-matched cohort study used data from the TriNetX global federated health network, examining 48,947 adult patients per group, each receiving lipid-lowering therapy due to heightened cardiovascular risks (e.g., diabetes mellitus, severe hypercholesterolemia). The cohorts were matched based on demographics and clinical characteristics, comparing outcomes between MASLD and non-MASLD groups. All-cause mortality was compared between the cohorts using risk analysis, odds ratios, and time-to-event analysis. Hazard ratios were calculated to evaluate proportional risks.
Results: In the all-cause mortality analysis, mean age was comparable between the MASLD (57.6 ± 13.6 years) and control cohorts (57.7 ± 13.5 years; p = 0.282), with approximately 70% of patients being white in both groups. Gender distribution was also equivalent (50.7% female; p = 0.939). During follow-up, all-cause mortality was significantly higher in the MASLD cohort (11.0%, n = 5,376) compared to controls (3.1%, n = 1,519), yielding an absolute risk difference of 7.9% (95% CI: 7.6–8.2, p < 0.001), a risk ratio of 3.54 (95% CI: 3.35–3.74), and an odds ratio of 3.85 (95% CI: 3.63–4.08). Kaplan–Meier curves demonstrated significantly lower survival probability in the MASLD group (77.5% vs. 93.7%, p < 0.001). The hazard ratio for mortality was 2.60 (95% CI: 2.46–2.76).
Discussion: This study demonstrates that MASLD substantially increases the risk of all-cause mortality among patients at elevated cardiovascular risk, independent of traditional risk factors and lipid-lowering therapy. The significantly higher mortality observed in the MASLD cohort underscores the critical importance of considering MASLD as an independent predictor of adverse outcomes. Current cardiovascular risk assessment models do not incorporate MASLD, highlighting a notable limitation. Integrating MASLD into future risk stratification tools may enable more accurate identification of high-risk individuals, potentially improving clinical management and outcomes.
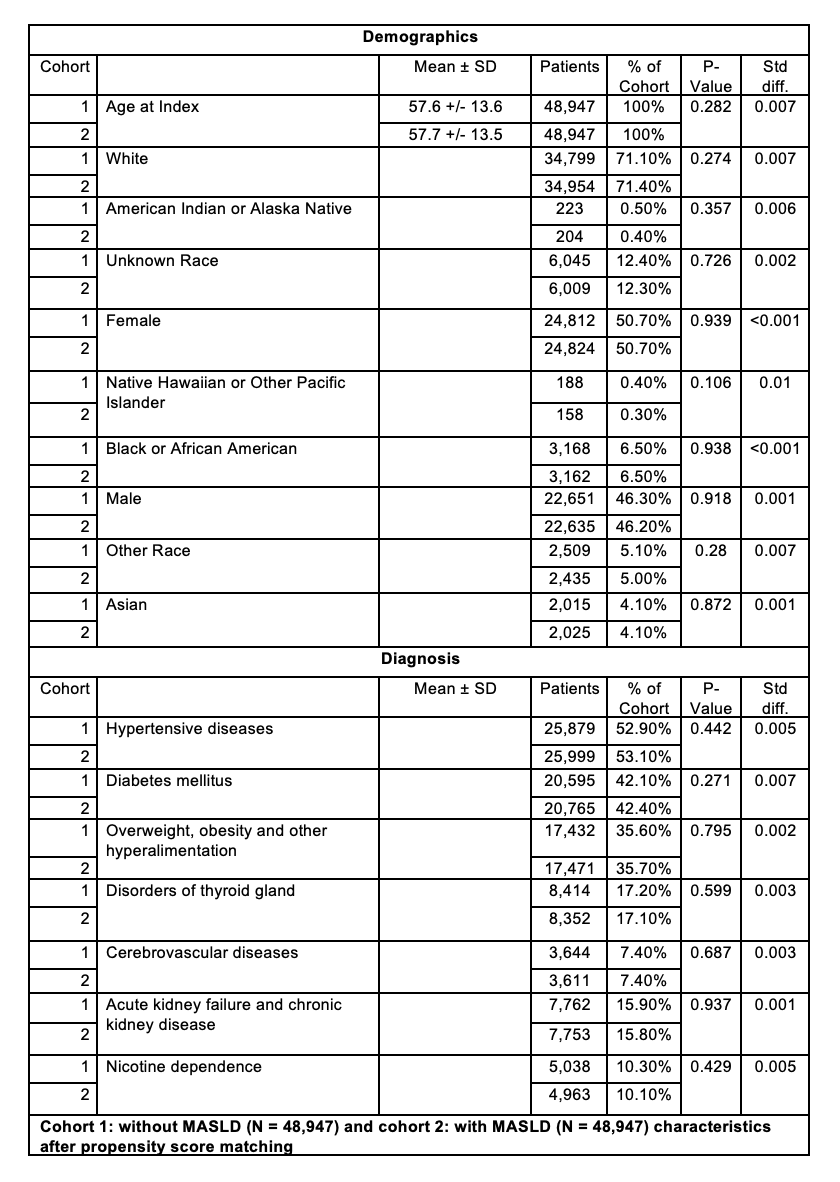
Figure: Table 1: Baseline characteristics for cohorts in the all-cause mortality analysis.
Disclosures:
Iyad Al-Bustami indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Kenan Alrejjal indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Ammar Abdulfattah indicated no relevant financial relationships.
Abbas Mallick indicated no relevant financial relationships.
Delwar Khan indicated no relevant financial relationships.
Rasha Hamid Numan Saleh indicated no relevant financial relationships.
Muhammad Desouky indicated no relevant financial relationships.
Daniel Low indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Iyad Al-Bustami, MD, MPH1, Sweta Lohani, MD1, Chaula Desai, MD1, Kenan Alrejjal, MBBS2, Kazi Haque, MD3, Ammar Yasser. Abdulfattah, MBBCh4, Abbas H. Mallick, MD5, Delwar Khan, MD1, Rasha Hamid Numan Saleh, 6, Muhammad Desouky, MD7, Daniel Low, MD8, Jamil Shah, MD1. P5766 - The Impact of MASLD on All-Cause Mortality Among Elevated Cardiovascular Risk Patients: A Propensity Score-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brooklyn Hospital Center, Brooklyn, NY; 2MedStar Georgetown/Washington Hospital Center, Washington, DC; 3University of Texas Health, McGovern Medical School, Houston, TX; 4SUNY Downstate Medical Center, Brooklyn, NY; 5The Brooklyn Hospital Center, New York, NY; 6MD, Brooklyn, NY; 7The Brooklyn Hospital Center, Brooklyn, NY; 8University of Toronto, Toronto, ON, Canada
Introduction: Metabolic dysfunction-associated steatotic liver disease (MASLD) significantly contributes to cardiovascular risks, but its precise impact within populations already at elevated cardiovascular risk remains insufficiently studied.
Methods: This retrospective, propensity score-matched cohort study used data from the TriNetX global federated health network, examining 48,947 adult patients per group, each receiving lipid-lowering therapy due to heightened cardiovascular risks (e.g., diabetes mellitus, severe hypercholesterolemia). The cohorts were matched based on demographics and clinical characteristics, comparing outcomes between MASLD and non-MASLD groups. All-cause mortality was compared between the cohorts using risk analysis, odds ratios, and time-to-event analysis. Hazard ratios were calculated to evaluate proportional risks.
Results: In the all-cause mortality analysis, mean age was comparable between the MASLD (57.6 ± 13.6 years) and control cohorts (57.7 ± 13.5 years; p = 0.282), with approximately 70% of patients being white in both groups. Gender distribution was also equivalent (50.7% female; p = 0.939). During follow-up, all-cause mortality was significantly higher in the MASLD cohort (11.0%, n = 5,376) compared to controls (3.1%, n = 1,519), yielding an absolute risk difference of 7.9% (95% CI: 7.6–8.2, p < 0.001), a risk ratio of 3.54 (95% CI: 3.35–3.74), and an odds ratio of 3.85 (95% CI: 3.63–4.08). Kaplan–Meier curves demonstrated significantly lower survival probability in the MASLD group (77.5% vs. 93.7%, p < 0.001). The hazard ratio for mortality was 2.60 (95% CI: 2.46–2.76).
Discussion: This study demonstrates that MASLD substantially increases the risk of all-cause mortality among patients at elevated cardiovascular risk, independent of traditional risk factors and lipid-lowering therapy. The significantly higher mortality observed in the MASLD cohort underscores the critical importance of considering MASLD as an independent predictor of adverse outcomes. Current cardiovascular risk assessment models do not incorporate MASLD, highlighting a notable limitation. Integrating MASLD into future risk stratification tools may enable more accurate identification of high-risk individuals, potentially improving clinical management and outcomes.
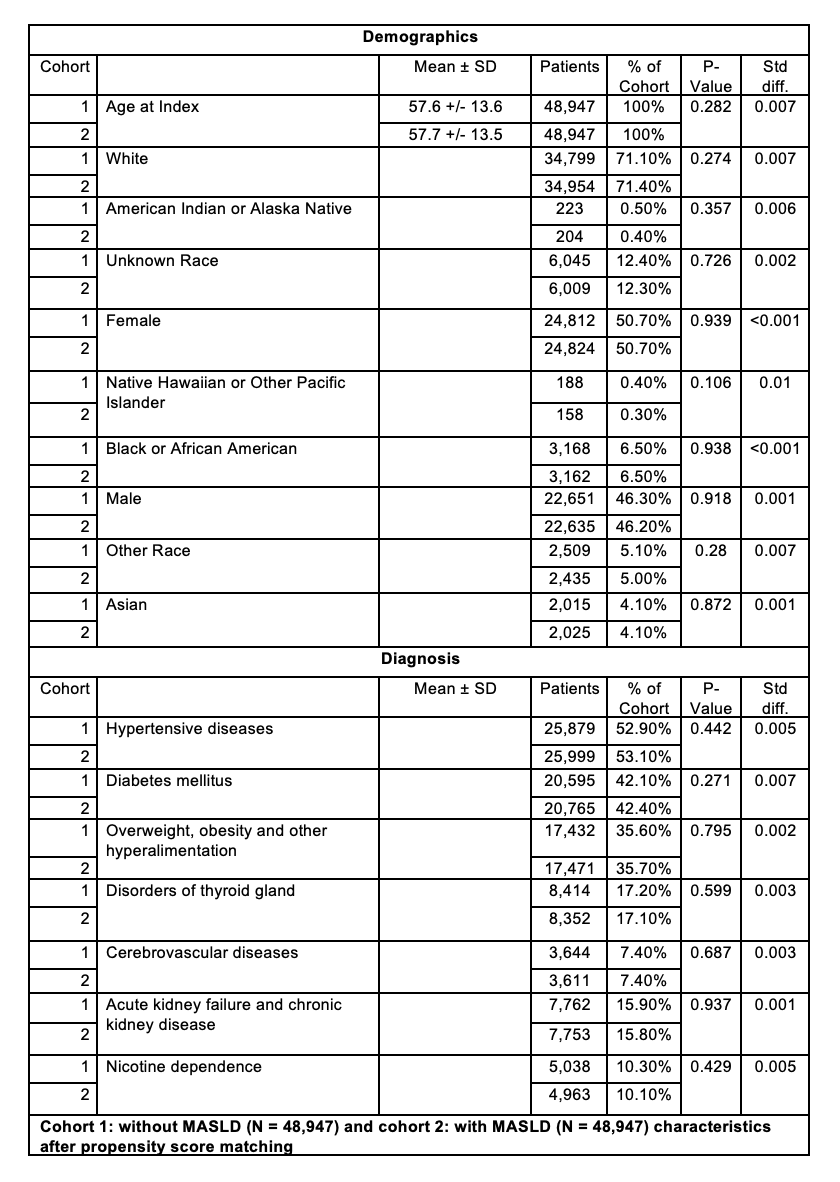
Figure: Table 1: Baseline characteristics for cohorts in the all-cause mortality analysis.
Disclosures:
Iyad Al-Bustami indicated no relevant financial relationships.
Sweta Lohani indicated no relevant financial relationships.
Chaula Desai indicated no relevant financial relationships.
Kenan Alrejjal indicated no relevant financial relationships.
Kazi Haque indicated no relevant financial relationships.
Ammar Abdulfattah indicated no relevant financial relationships.
Abbas Mallick indicated no relevant financial relationships.
Delwar Khan indicated no relevant financial relationships.
Rasha Hamid Numan Saleh indicated no relevant financial relationships.
Muhammad Desouky indicated no relevant financial relationships.
Daniel Low indicated no relevant financial relationships.
Jamil Shah indicated no relevant financial relationships.
Iyad Al-Bustami, MD, MPH1, Sweta Lohani, MD1, Chaula Desai, MD1, Kenan Alrejjal, MBBS2, Kazi Haque, MD3, Ammar Yasser. Abdulfattah, MBBCh4, Abbas H. Mallick, MD5, Delwar Khan, MD1, Rasha Hamid Numan Saleh, 6, Muhammad Desouky, MD7, Daniel Low, MD8, Jamil Shah, MD1. P5766 - The Impact of MASLD on All-Cause Mortality Among Elevated Cardiovascular Risk Patients: A Propensity Score-Matched Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
