Tuesday Poster Session
Category: Liver
P5764 - Mortality Trends From Liver Failure in Patients With Hepatic Neoplasms: CDC Data Analysis,1999 to 2020
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ammad Javaid Chaudhary, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Huzefa Habib, MD3, Fatima Sial, MBBS4, Mahrosh Kasbati, MBBS5, Rabia Shahid, MBBS6, Syed-Mohammed Jafri, MD2
1Brigham and Women's Hospital, Boston, MA; 2Henry Ford Health, Detroit, MI; 3King Edward Medical University, Mailsi, Punjab, Pakistan; 4King Edward Medical University, Lahore, Punjab, Pakistan; 5Dow University of Health Sciences, Karachi, Sindh, Pakistan; 6Faisalabad Medical University, Pakistan, Lahore, Punjab, Pakistan
Introduction: Hepatic neoplasms complicated by hepatic failure are major contributors to liver-related mortality in the United States. Their evolving burden, influenced by viral hepatitis, alcohol use, and metabolic disorders, underscores the need for stratified trend analyses to inform targeted public health interventions.
Methods: A retrospective analysis used CDC data from 1999 to 2020. AAMRs per 100,000 were calculated for individuals aged ≥25 years. Joinpoint regression evaluated trends, estimating annual percent change (APC) and average annual percent change (AAPC) with 95% confidence intervals. Analyses were stratified by year, age, sex, race/ethnicity, region, and urbanization.
Results: From 1999–2020, hepatic neoplasm and hepatic failure–related mortality accounted for 37,465 deaths in the United States, with AAMR declining from 0.90 to 0.68 per 100,000 (AAPC: –0.95; 95% CI: –1.22 to –0.58; p < 0.000001).
Crude mortality rates declined across most age groups, with the largest relative decrease among those aged 35–44 (AAPC: –2.93), then 85+ (–2.43) and 75–84 (–1.57). An insignificant trend was seen among those aged 55–64 (0.72), 65–74 (–0.24), and 45–54 (–3.80).
By sex, male AAMR declined from 1.41 to 1.05 (–1.01; p = 0.0004), and female AAMR from 0.49 to 0.37 (–1.19; p < 0.000001). Males accounted for 27,036 (72.1%) deaths, females for 10,429 (27.9%).
Among racial groups, Asian or Pacific Islanders had the steepest decline, with AAMR falling from 3.04 to 0.91 (–5.62; p < 0.000001). Hispanic individuals dropped from 1.85 to 1.12 (–1.76; p < 0.000001), while White and Black individuals declined more modestly (–0.60 and –0.63, respectively).
Regionally, the West had the greatest reduction, from 1.28 to 0.83 (–1.71; p < 0.000001), then the Northeast (–1.01). The Midwest and South had flatter, insignificant declines (–0.55 and –0.32).
By urbanization, large central metro areas declined from 1.13 to 0.66 (–2.08; p < 0.000001), then large fringe metros (–1.01). Small metro and micropolitan areas showed increasing trends (0.77 and 0.87), while noncore areas remained stable (–0.05).
Discussion: Hepatic failure–related mortality among patients with hepatic neoplasms declined overall from 1999 to 2020, especially among younger adults, females, Asian or Pacific Islanders, and residents of the West and large metro areas. Stable or rising trends in some age and geographic groups call for targeted interventions. AI tools were used to enhance writing clarity.
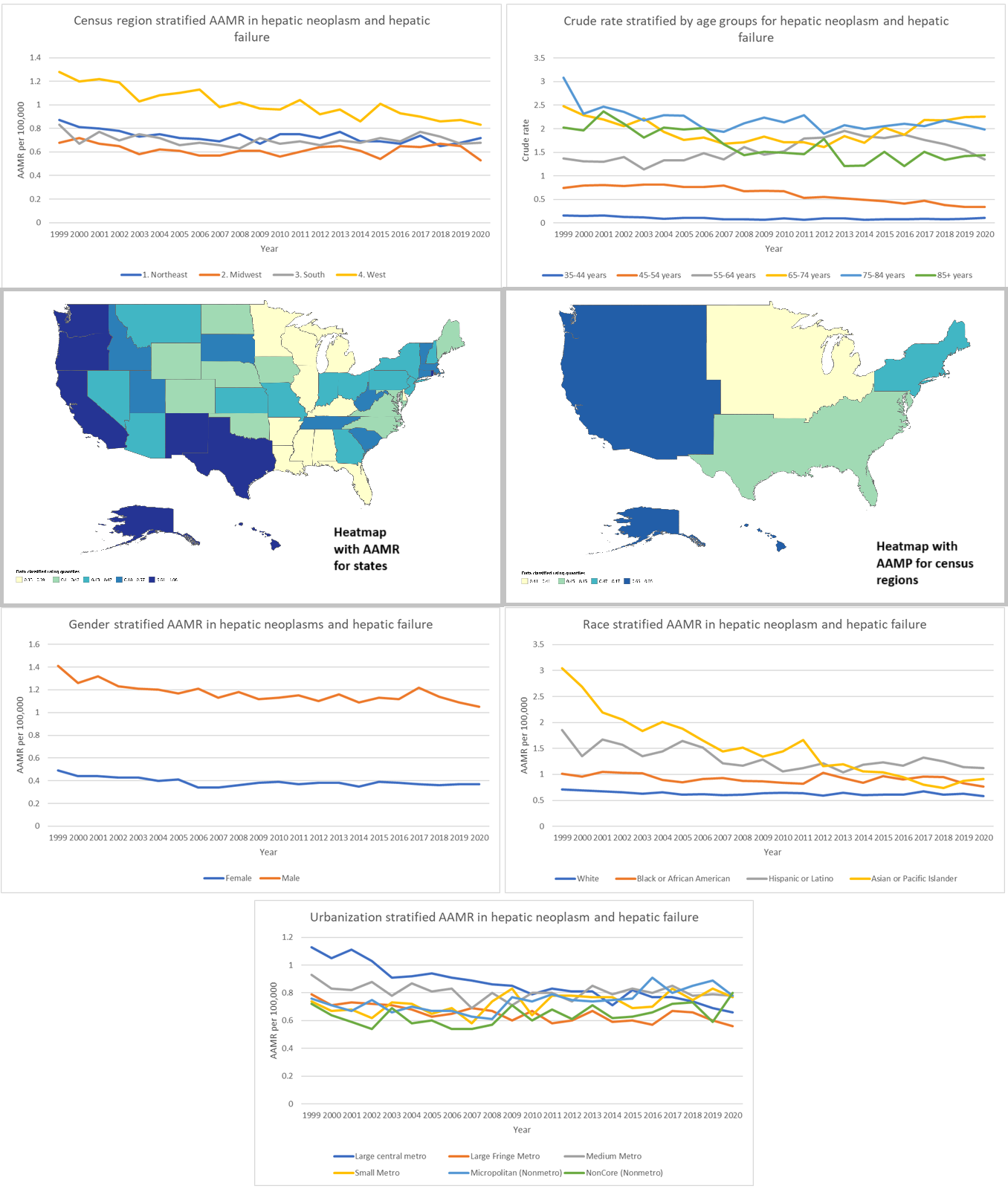
Figure: **Figure Caption:**
Trends in age-adjusted mortality rates (AAMRs) and crude rates for hepatic failure–related deaths among patients with hepatic neoplasms in the U.S. (1999–2020), stratified by region, age, sex, race/ethnicity, urbanization, and state-level distribution.
Disclosures:
Hafsa Shahid indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Huzefa Habib indicated no relevant financial relationships.
Fatima Sial indicated no relevant financial relationships.
Mahrosh Kasbati indicated no relevant financial relationships.
Rabia Shahid indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Huzefa Habib, MD3, Fatima Sial, MBBS4, Mahrosh Kasbati, MBBS5, Rabia Shahid, MBBS6, Syed-Mohammed Jafri, MD2. P5764 - Mortality Trends From Liver Failure in Patients With Hepatic Neoplasms: CDC Data Analysis,1999 to 2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Brigham and Women's Hospital, Boston, MA; 2Henry Ford Health, Detroit, MI; 3King Edward Medical University, Mailsi, Punjab, Pakistan; 4King Edward Medical University, Lahore, Punjab, Pakistan; 5Dow University of Health Sciences, Karachi, Sindh, Pakistan; 6Faisalabad Medical University, Pakistan, Lahore, Punjab, Pakistan
Introduction: Hepatic neoplasms complicated by hepatic failure are major contributors to liver-related mortality in the United States. Their evolving burden, influenced by viral hepatitis, alcohol use, and metabolic disorders, underscores the need for stratified trend analyses to inform targeted public health interventions.
Methods: A retrospective analysis used CDC data from 1999 to 2020. AAMRs per 100,000 were calculated for individuals aged ≥25 years. Joinpoint regression evaluated trends, estimating annual percent change (APC) and average annual percent change (AAPC) with 95% confidence intervals. Analyses were stratified by year, age, sex, race/ethnicity, region, and urbanization.
Results: From 1999–2020, hepatic neoplasm and hepatic failure–related mortality accounted for 37,465 deaths in the United States, with AAMR declining from 0.90 to 0.68 per 100,000 (AAPC: –0.95; 95% CI: –1.22 to –0.58; p < 0.000001).
Crude mortality rates declined across most age groups, with the largest relative decrease among those aged 35–44 (AAPC: –2.93), then 85+ (–2.43) and 75–84 (–1.57). An insignificant trend was seen among those aged 55–64 (0.72), 65–74 (–0.24), and 45–54 (–3.80).
By sex, male AAMR declined from 1.41 to 1.05 (–1.01; p = 0.0004), and female AAMR from 0.49 to 0.37 (–1.19; p < 0.000001). Males accounted for 27,036 (72.1%) deaths, females for 10,429 (27.9%).
Among racial groups, Asian or Pacific Islanders had the steepest decline, with AAMR falling from 3.04 to 0.91 (–5.62; p < 0.000001). Hispanic individuals dropped from 1.85 to 1.12 (–1.76; p < 0.000001), while White and Black individuals declined more modestly (–0.60 and –0.63, respectively).
Regionally, the West had the greatest reduction, from 1.28 to 0.83 (–1.71; p < 0.000001), then the Northeast (–1.01). The Midwest and South had flatter, insignificant declines (–0.55 and –0.32).
By urbanization, large central metro areas declined from 1.13 to 0.66 (–2.08; p < 0.000001), then large fringe metros (–1.01). Small metro and micropolitan areas showed increasing trends (0.77 and 0.87), while noncore areas remained stable (–0.05).
Discussion: Hepatic failure–related mortality among patients with hepatic neoplasms declined overall from 1999 to 2020, especially among younger adults, females, Asian or Pacific Islanders, and residents of the West and large metro areas. Stable or rising trends in some age and geographic groups call for targeted interventions. AI tools were used to enhance writing clarity.
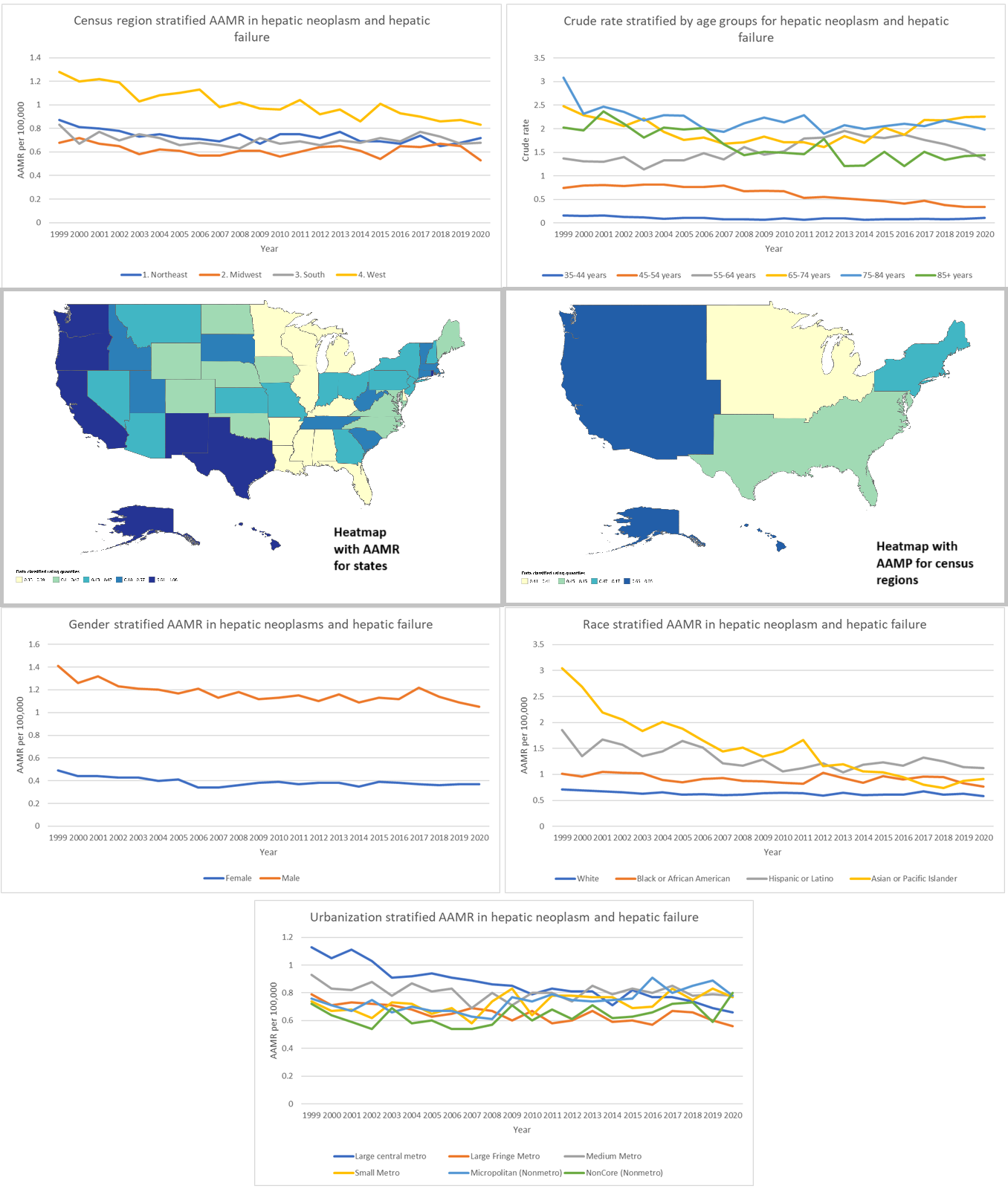
Figure: **Figure Caption:**
Trends in age-adjusted mortality rates (AAMRs) and crude rates for hepatic failure–related deaths among patients with hepatic neoplasms in the U.S. (1999–2020), stratified by region, age, sex, race/ethnicity, urbanization, and state-level distribution.
Disclosures:
Hafsa Shahid indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Huzefa Habib indicated no relevant financial relationships.
Fatima Sial indicated no relevant financial relationships.
Mahrosh Kasbati indicated no relevant financial relationships.
Rabia Shahid indicated no relevant financial relationships.
Syed-Mohammed Jafri: Abbvie – Speakers Bureau. Gilead – Speakers Bureau. Intercept – Speakers Bureau. Ironwood – Speakers Bureau. Takeda – Speakers Bureau.
Hafsa Shahid, MD1, Ammad Javaid. Chaudhary, MD2, Huzefa Habib, MD3, Fatima Sial, MBBS4, Mahrosh Kasbati, MBBS5, Rabia Shahid, MBBS6, Syed-Mohammed Jafri, MD2. P5764 - Mortality Trends From Liver Failure in Patients With Hepatic Neoplasms: CDC Data Analysis,1999 to 2020, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
