Tuesday Poster Session
Category: Interventional Endoscopy
P5734 - Silent Escape: A Catastrophic Case of Subcutaneous and Multicompartment Air Dissection Following ERCP in a Cirrhotic Patient
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Rajkumar Dipakbhai Patel, MD (he/him/his)
RWJBarnabas Health, Trinitas Regional Medical Center
Elizabeth, NJ
Presenting Author(s)
Rajkumar Dipakbhai Patel, MD1, Ahmed Omran, MD2, Vrusti Dipakbhai Patel Patel, MBBS3, Unzela Iqbal, MD1, Walaa Hasan, MD4
1RWJBarnabas Health, Trinitas Regional Medical Center, Elizabeth, NJ; 2RWJBarnabas Health, Trinitas Regional Medical Center, Linden, NJ; 3Baroda Medical College, Elizabeth, NJ; 4RWJBarnabas Health, Trinitas Regional Medical Center, Cranford, NJ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a widely used but high-risk procedure with complication rates reaching 10.1%. Common complications include post-ERCP pancreatitis (6.9%), bleeding (0.9%), infection (1%), and perforation (0.3–0.7%). Rarely, patients may develop severe air-related complications such as subcutaneous emphysema (SE), pneumothorax, pneumomediastinum, or pneumoperitoneum. Literature reports fewer than 10 such cases involving extensive SE post-ERCP, most associated with identifiable perforation sites. Mortality in ERCP-related perforation can reach 20%, particularly in older patients and those with comorbidities.
Case Description/
Methods: We present a 67-year-old male with cirrhosis and choledocholithiasis who underwent ERCP for biliary decompression. Cannulation of a peridiverticular papilla proved unsuccessful, and the procedure was aborted. The patient deteriorated rapidly, developing acute respiratory distress and widespread subcutaneous crepitus. Imaging revealed bilateral pneumothoraces, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum, and extensive SE throughout the body. Despite detailed CT evaluation, no definitive site of perforation was visualized, likely due to extensive air obscuration but most likely duodenal diverticulum. Management included blowhole incisions with subcutaneous VAC, IV antibiotics, bowel rest, and hemodynamic support. The patient subsequently developed undifferentiated shock and decompensated heart failure, passing away on day six.
Discussion: This case highlights a rare and life-threatening ERCP complication where widespread air dissection occurred without localization of a perforation. Possible contributors include microperforation, pressure-related mucosal breach, or dissection from compressed air. While many cases resolve with conservative treatment, this case required blowhole decompression and subcutaneous VAC therapy—a rare intervention previously described in trauma and severe SE literature. But prognosis remains poor in patients with significant comorbidities. This case underscores the diagnostic difficulty in patients with altered anatomy and cirrhosis, and the need for early imaging and tailored intervention. Extensive SE and air dissection post-ERCP may occur even without a visible perforation and carry significant mortality risk, particularly in high-risk patients. Early multidisciplinary management is essential, and further guidelines are needed to manage such rare complications effectively.
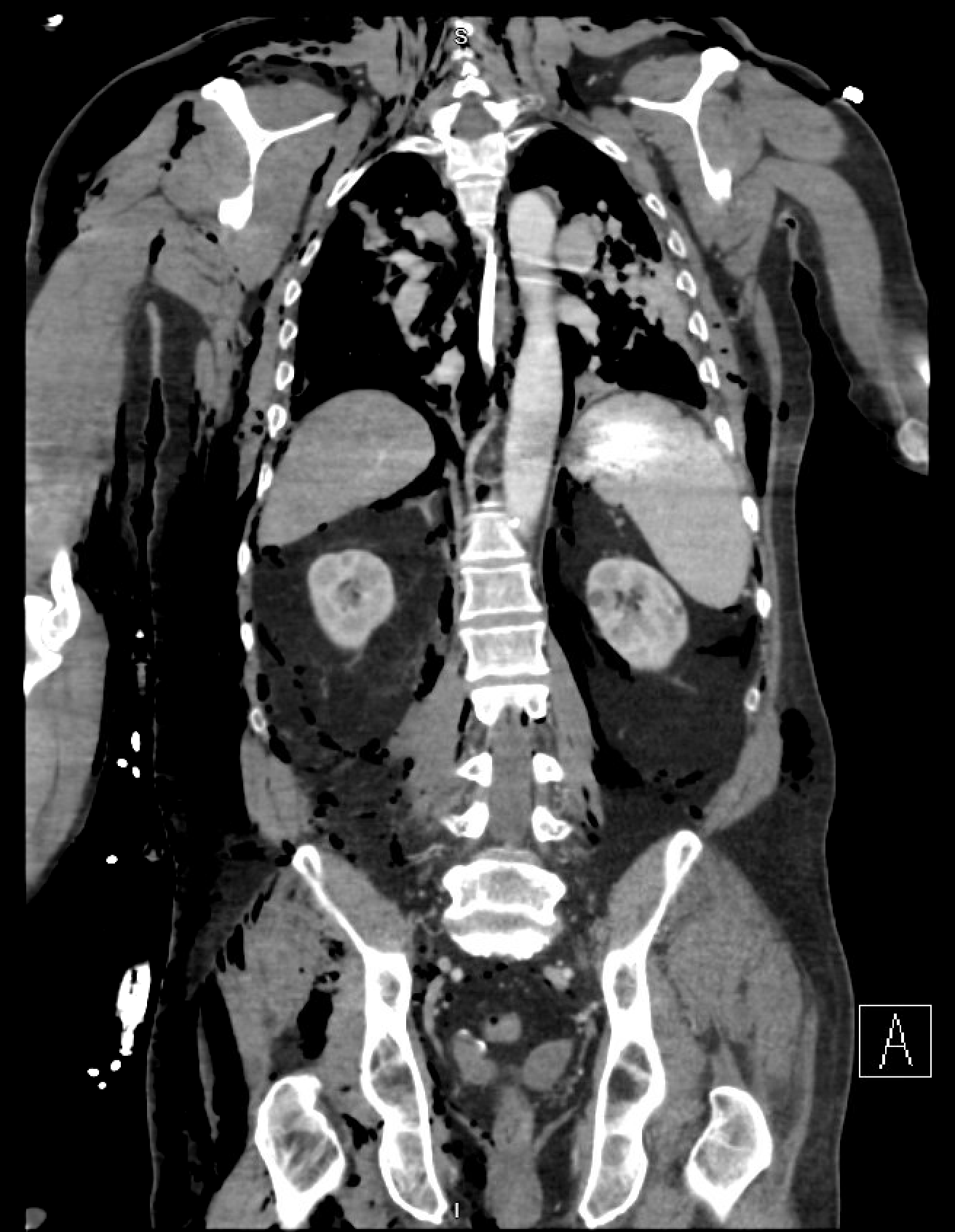
Figure: Extensive SE with pneumothorax, pneumomediastinum, pneumoretroperitoneum

Figure: Cholelithiasis, CBD 9 mm, Choledocholithiasis: 2 filling defects, upto 4 mm
Disclosures:
Rajkumar Dipakbhai Patel indicated no relevant financial relationships.
Ahmed Omran indicated no relevant financial relationships.
Vrusti Dipakbhai Patel Patel indicated no relevant financial relationships.
Unzela Iqbal indicated no relevant financial relationships.
Walaa Hasan indicated no relevant financial relationships.
Rajkumar Dipakbhai Patel, MD1, Ahmed Omran, MD2, Vrusti Dipakbhai Patel Patel, MBBS3, Unzela Iqbal, MD1, Walaa Hasan, MD4. P5734 - Silent Escape: A Catastrophic Case of Subcutaneous and Multicompartment Air Dissection Following ERCP in a Cirrhotic Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1RWJBarnabas Health, Trinitas Regional Medical Center, Elizabeth, NJ; 2RWJBarnabas Health, Trinitas Regional Medical Center, Linden, NJ; 3Baroda Medical College, Elizabeth, NJ; 4RWJBarnabas Health, Trinitas Regional Medical Center, Cranford, NJ
Introduction: Endoscopic retrograde cholangiopancreatography (ERCP) is a widely used but high-risk procedure with complication rates reaching 10.1%. Common complications include post-ERCP pancreatitis (6.9%), bleeding (0.9%), infection (1%), and perforation (0.3–0.7%). Rarely, patients may develop severe air-related complications such as subcutaneous emphysema (SE), pneumothorax, pneumomediastinum, or pneumoperitoneum. Literature reports fewer than 10 such cases involving extensive SE post-ERCP, most associated with identifiable perforation sites. Mortality in ERCP-related perforation can reach 20%, particularly in older patients and those with comorbidities.
Case Description/
Methods: We present a 67-year-old male with cirrhosis and choledocholithiasis who underwent ERCP for biliary decompression. Cannulation of a peridiverticular papilla proved unsuccessful, and the procedure was aborted. The patient deteriorated rapidly, developing acute respiratory distress and widespread subcutaneous crepitus. Imaging revealed bilateral pneumothoraces, pneumomediastinum, pneumoperitoneum, pneumoretroperitoneum, and extensive SE throughout the body. Despite detailed CT evaluation, no definitive site of perforation was visualized, likely due to extensive air obscuration but most likely duodenal diverticulum. Management included blowhole incisions with subcutaneous VAC, IV antibiotics, bowel rest, and hemodynamic support. The patient subsequently developed undifferentiated shock and decompensated heart failure, passing away on day six.
Discussion: This case highlights a rare and life-threatening ERCP complication where widespread air dissection occurred without localization of a perforation. Possible contributors include microperforation, pressure-related mucosal breach, or dissection from compressed air. While many cases resolve with conservative treatment, this case required blowhole decompression and subcutaneous VAC therapy—a rare intervention previously described in trauma and severe SE literature. But prognosis remains poor in patients with significant comorbidities. This case underscores the diagnostic difficulty in patients with altered anatomy and cirrhosis, and the need for early imaging and tailored intervention. Extensive SE and air dissection post-ERCP may occur even without a visible perforation and carry significant mortality risk, particularly in high-risk patients. Early multidisciplinary management is essential, and further guidelines are needed to manage such rare complications effectively.
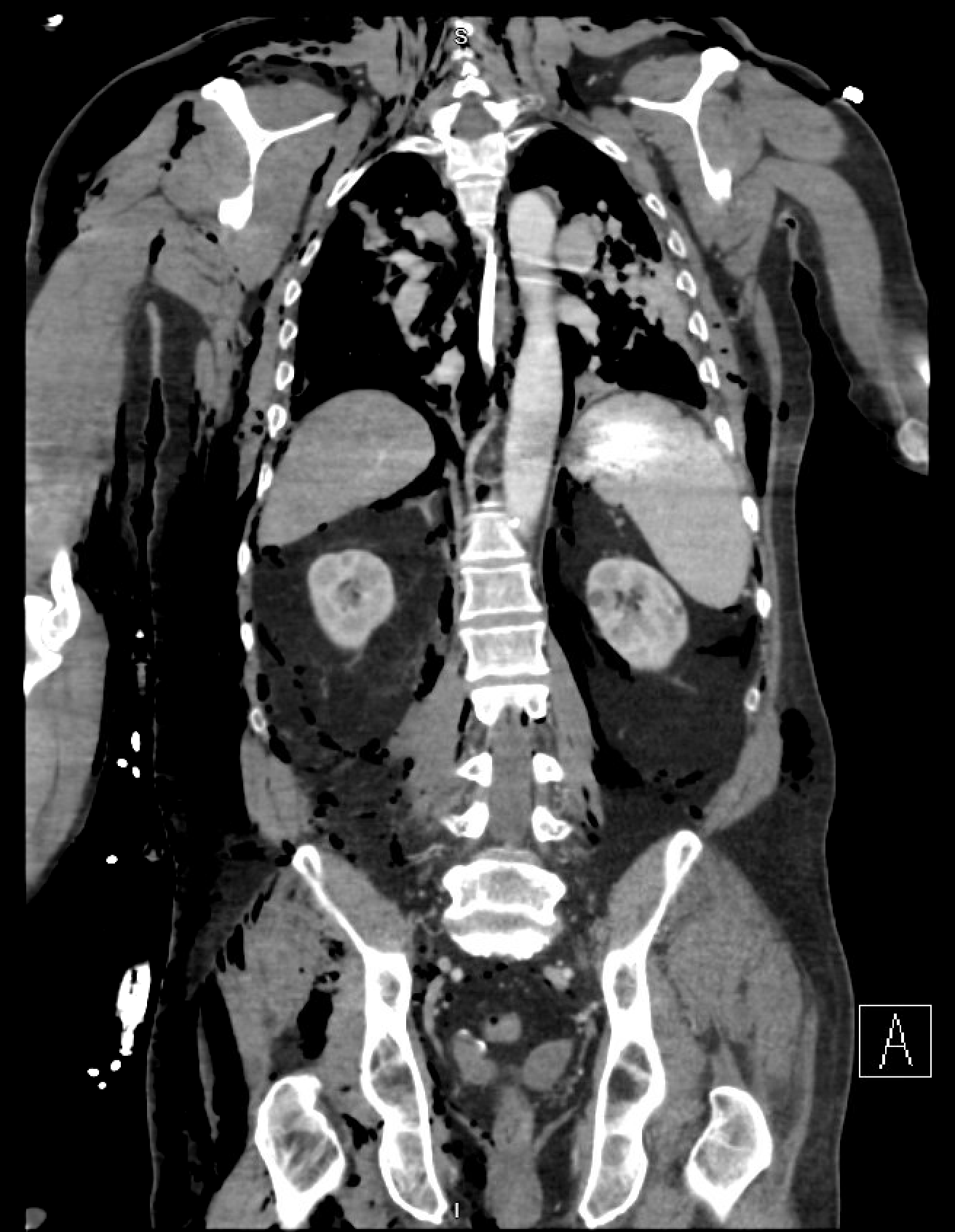
Figure: Extensive SE with pneumothorax, pneumomediastinum, pneumoretroperitoneum

Figure: Cholelithiasis, CBD 9 mm, Choledocholithiasis: 2 filling defects, upto 4 mm
Disclosures:
Rajkumar Dipakbhai Patel indicated no relevant financial relationships.
Ahmed Omran indicated no relevant financial relationships.
Vrusti Dipakbhai Patel Patel indicated no relevant financial relationships.
Unzela Iqbal indicated no relevant financial relationships.
Walaa Hasan indicated no relevant financial relationships.
Rajkumar Dipakbhai Patel, MD1, Ahmed Omran, MD2, Vrusti Dipakbhai Patel Patel, MBBS3, Unzela Iqbal, MD1, Walaa Hasan, MD4. P5734 - Silent Escape: A Catastrophic Case of Subcutaneous and Multicompartment Air Dissection Following ERCP in a Cirrhotic Patient, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
