Tuesday Poster Session
Category: Interventional Endoscopy
P5733 - Self-Inflicted Wound: Spontaneous Pancreatic Duct Stent Migration Into Hepatic Parenchyma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Asanka Ekanayake, MD
Walter Reed National Military Medical Center
Bethesda, MD
Presenting Author(s)
Asanka Ekanayake, MD, Charleston R.. Powell, MD, Patrick E.. Young, MD, FACG
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Post-operative pancreaticojejunostomy (PJ) stenosis and pancreatic fistula are complications of a pancreaticoduodenectomy. Interoperative stenting, often using pediatric feeding tubes, can mitigate these risks. Stents usually pass spontaneously but may take over a year to do so. Complications from retained stents include pancreatitis, bleeding, infection, occlusion, perforation, stent fracture, and intestinal obstruction. Stent migration through bile ducts via the biliary anastomosis has been reported to cause hepatic abscess. We report the only known case of PJ stent migration directly into the hepatic parenchyma.
Case Description/
Methods: A 67-year-old female with a history of partially resectable pancreatic adenocarcinoma after chemotherapy, radiation, Whipple procedure, and complicated by recurrent metastatic disease was admitted with cholangitis. CT imaging showed malignant obstruction of the pancreaticobiliary limb as the cause of cholangitis. Endoscopic gastrojejunostomy (GJ) using a lumen-opposing metal stent (LAMS) relieved this obstruction. Six months later, she was admitted with recurrent cholangitis. CT showed increased hepatic tumor burden, progressive biliary ductal dilation, and migration of the PJ stent into the left hepatic lobe. Enteroscopy revealed a partially migrated, patent LAMS which was removed with minimal manipulation. The jejunum was filled with dense clots that were careful dissected using snare, lavage, and forceps allowing for visualization and removal of the migrated PJ stent. Extensive clot burden and thrombocytopenia prevented safe access to the biliary anastomosis. The patient opted for a comfort-care approach over further aggressive attempts at biliary drainage and expired shortly after.
Discussion: This is the first case to show PJ stent migration directly into the liver. It illustrates the challenges of managing issues in patients with metastatic pancreatic cancer with surgically altered anatomy. While endoscopic GJ with LAMS successfully eased obstruction of the pancreaticobiliary limb, the patient developed recurrent cholangitis from both worsening intrahepatic tumor burden and clot burden from PJ stent migration into the liver. While stent migration is a rare complication, it can cause serious complications. Furthermore, endoscopic removal of a migrated stent is possible and could likely remove a nidus for the development of hepatic abscess. However, it's key to carefully weigh the risks of an invasive procedures against the patient’s overall prognosis.
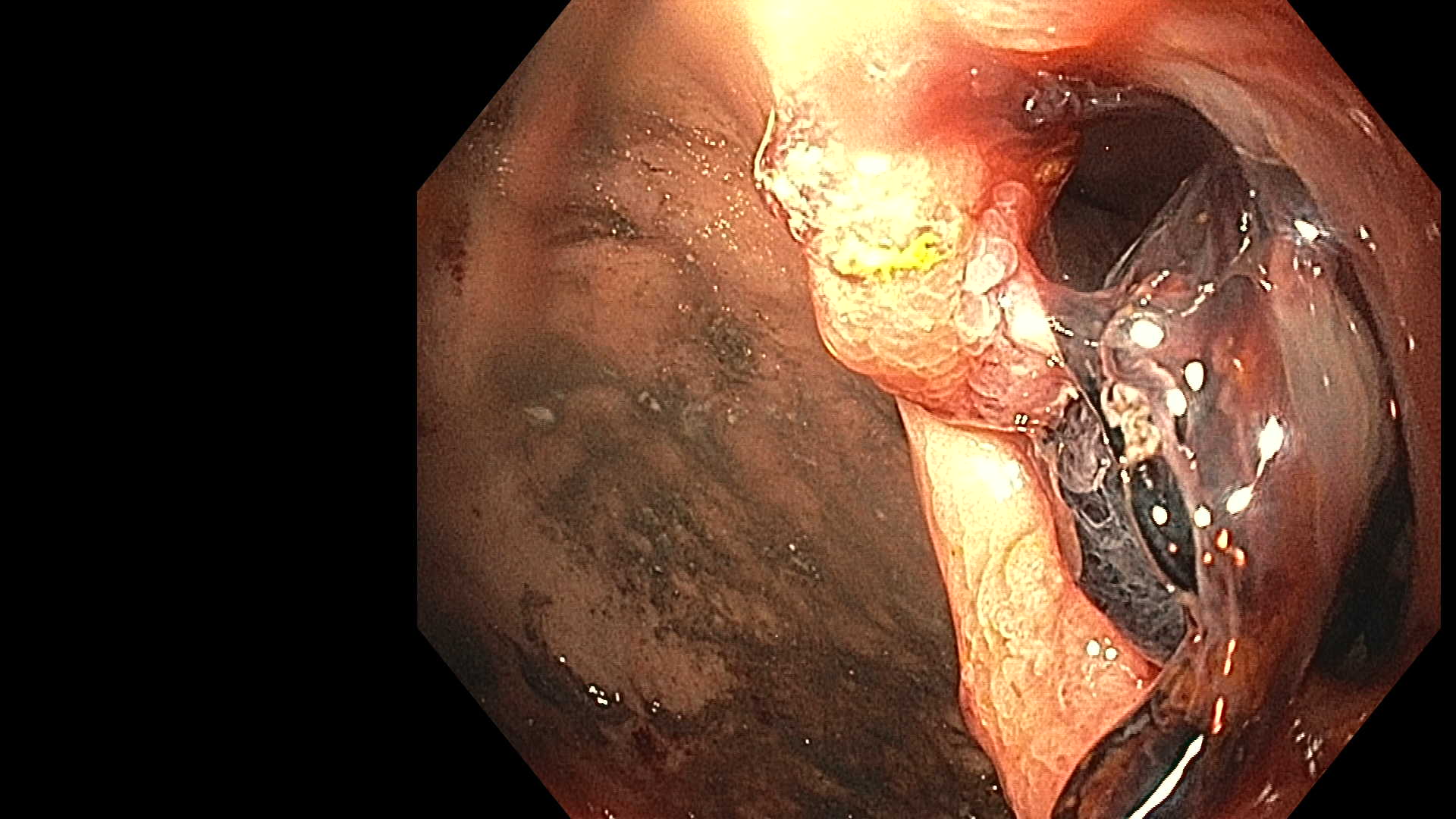
Figure: Endoscopic view of distal end of pediatric feeding tube
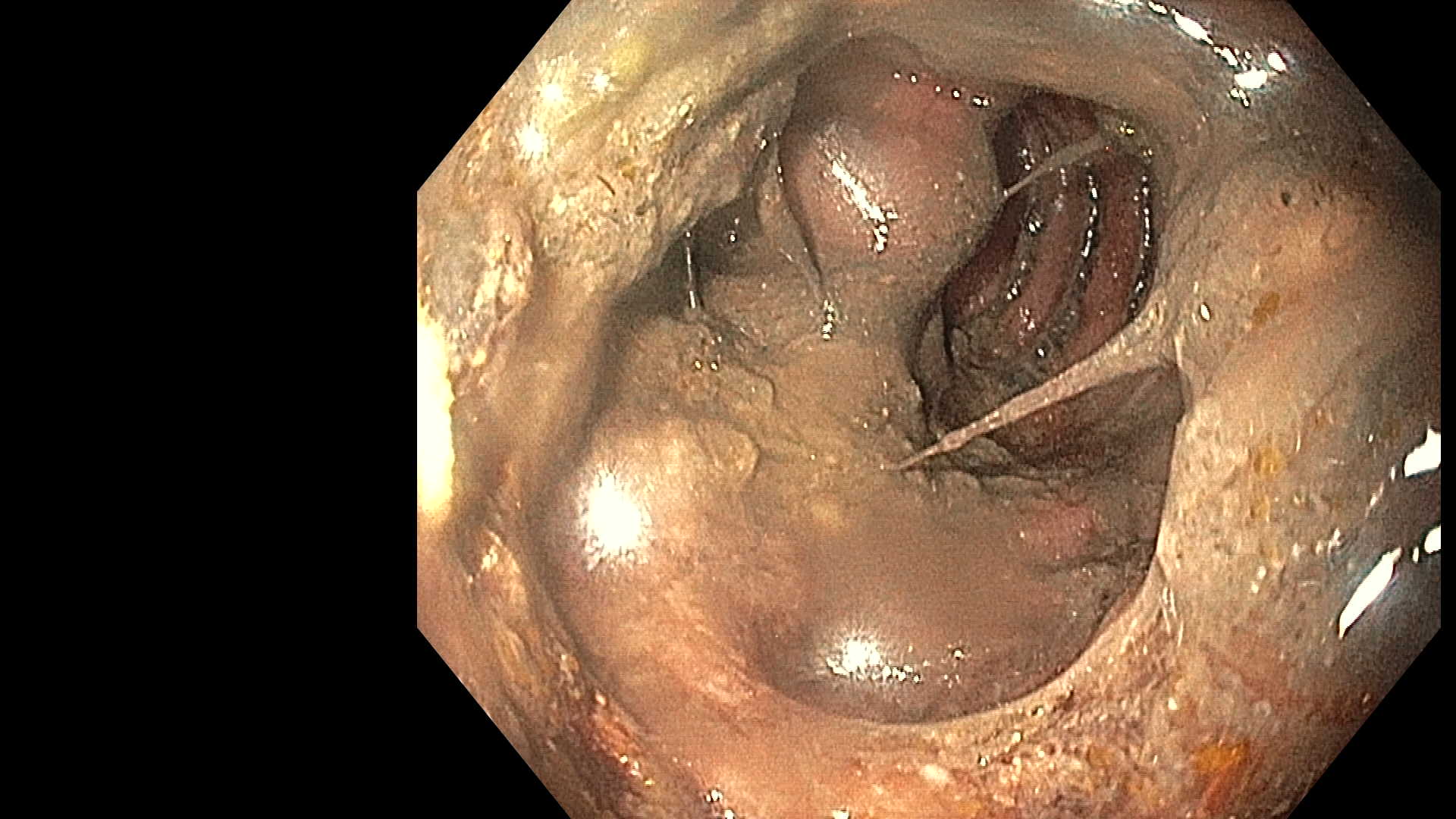
Figure: Dense clot and necrotic debris preventing biliary access
Disclosures:
Asanka Ekanayake indicated no relevant financial relationships.
Charleston Powell indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Asanka Ekanayake, MD, Charleston R.. Powell, MD, Patrick E.. Young, MD, FACG. P5733 - Self-Inflicted Wound: Spontaneous Pancreatic Duct Stent Migration Into Hepatic Parenchyma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Walter Reed National Military Medical Center, Bethesda, MD
Introduction: Post-operative pancreaticojejunostomy (PJ) stenosis and pancreatic fistula are complications of a pancreaticoduodenectomy. Interoperative stenting, often using pediatric feeding tubes, can mitigate these risks. Stents usually pass spontaneously but may take over a year to do so. Complications from retained stents include pancreatitis, bleeding, infection, occlusion, perforation, stent fracture, and intestinal obstruction. Stent migration through bile ducts via the biliary anastomosis has been reported to cause hepatic abscess. We report the only known case of PJ stent migration directly into the hepatic parenchyma.
Case Description/
Methods: A 67-year-old female with a history of partially resectable pancreatic adenocarcinoma after chemotherapy, radiation, Whipple procedure, and complicated by recurrent metastatic disease was admitted with cholangitis. CT imaging showed malignant obstruction of the pancreaticobiliary limb as the cause of cholangitis. Endoscopic gastrojejunostomy (GJ) using a lumen-opposing metal stent (LAMS) relieved this obstruction. Six months later, she was admitted with recurrent cholangitis. CT showed increased hepatic tumor burden, progressive biliary ductal dilation, and migration of the PJ stent into the left hepatic lobe. Enteroscopy revealed a partially migrated, patent LAMS which was removed with minimal manipulation. The jejunum was filled with dense clots that were careful dissected using snare, lavage, and forceps allowing for visualization and removal of the migrated PJ stent. Extensive clot burden and thrombocytopenia prevented safe access to the biliary anastomosis. The patient opted for a comfort-care approach over further aggressive attempts at biliary drainage and expired shortly after.
Discussion: This is the first case to show PJ stent migration directly into the liver. It illustrates the challenges of managing issues in patients with metastatic pancreatic cancer with surgically altered anatomy. While endoscopic GJ with LAMS successfully eased obstruction of the pancreaticobiliary limb, the patient developed recurrent cholangitis from both worsening intrahepatic tumor burden and clot burden from PJ stent migration into the liver. While stent migration is a rare complication, it can cause serious complications. Furthermore, endoscopic removal of a migrated stent is possible and could likely remove a nidus for the development of hepatic abscess. However, it's key to carefully weigh the risks of an invasive procedures against the patient’s overall prognosis.
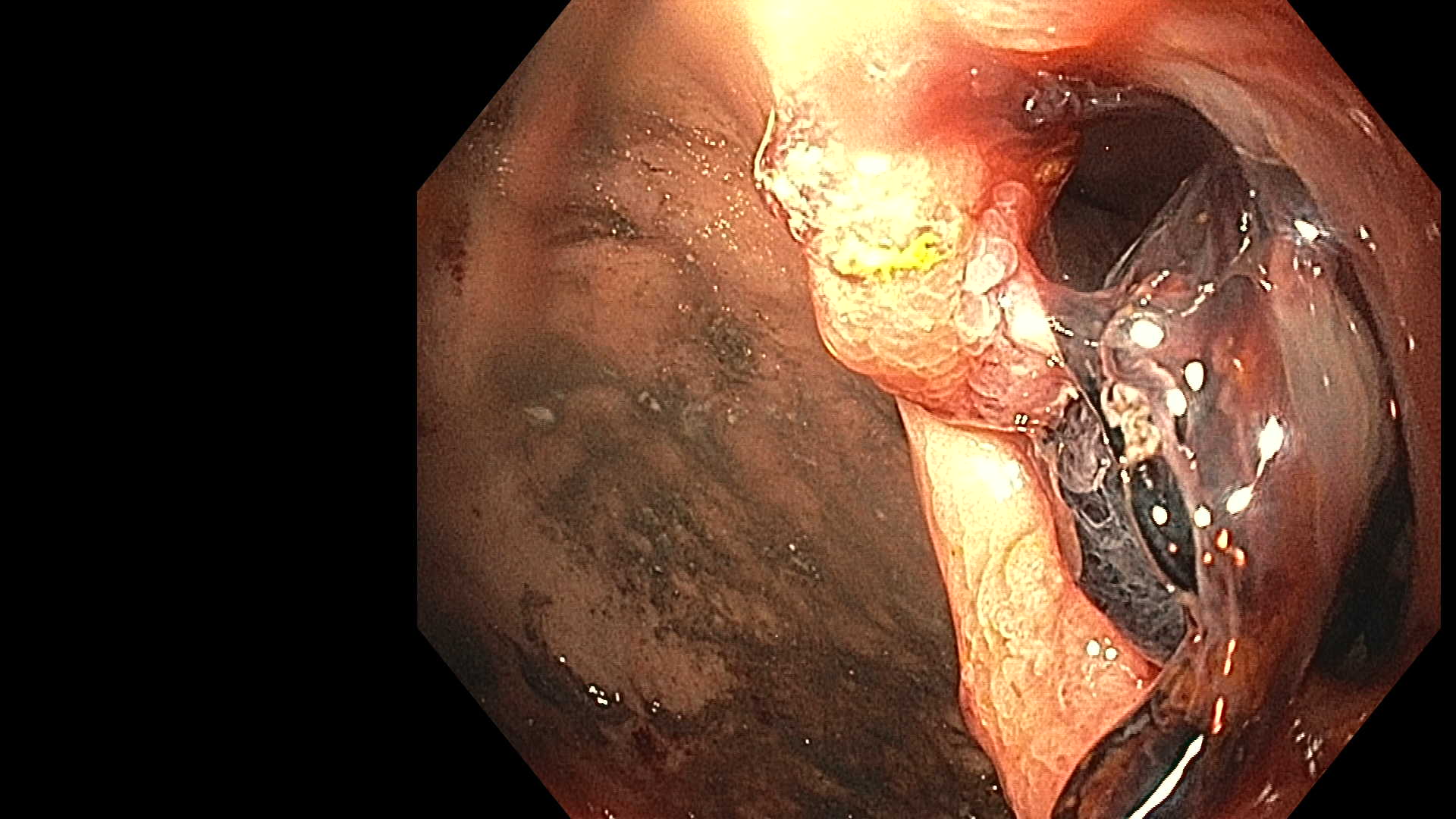
Figure: Endoscopic view of distal end of pediatric feeding tube
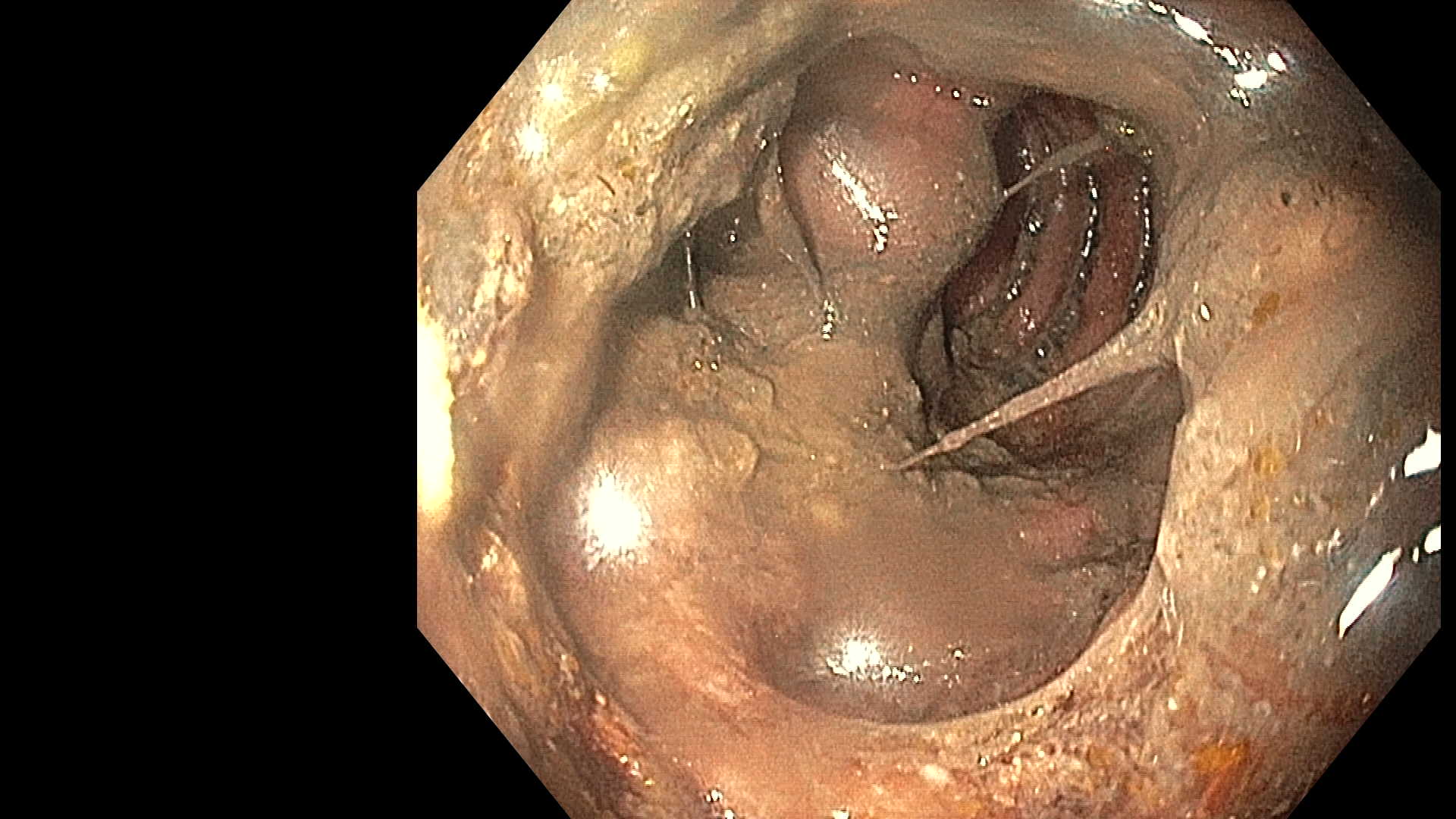
Figure: Dense clot and necrotic debris preventing biliary access
Disclosures:
Asanka Ekanayake indicated no relevant financial relationships.
Charleston Powell indicated no relevant financial relationships.
Patrick Young indicated no relevant financial relationships.
Asanka Ekanayake, MD, Charleston R.. Powell, MD, Patrick E.. Young, MD, FACG. P5733 - Self-Inflicted Wound: Spontaneous Pancreatic Duct Stent Migration Into Hepatic Parenchyma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
