Tuesday Poster Session
Category: Interventional Endoscopy
P5731 - Innovative Use of Underwater Technique to Facilitate ERCP in the Setting of Anatomic and Inflammatory Barriers in Acute Pancreatitis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- CB
Cristina Batarseh, MD (she/her/hers)
University of Massachusetts Chan Medical School - Baystate Health
Springfield, MA
Presenting Author(s)
Cristina Batarseh, MD, Aizaz Khan, MD, Tushaar Shrimanker, MD, Syed Hamza Sohail, MD, Tiago Martins, DO, Kevin Groudan, MD, Nha Duong, DO
University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA
Introduction: We present a case of complicated acute pancreatitis (AP) characterized by a pancreatic duct (PD) leak and gastric outlet obstruction (GOO) secondary to extrinsic compression from peripancreatic fluid and duodenal edema, creating a significant technical challenge for endoscopic retrograde cholangiopancreatography (ERCP).
Case Description/
Methods: Our patient is a 43-year-old M with a history of alcohol use and multiple prior admissions for uncomplicated AP, who presented with a 6 days of nausea, vomiting, and abdominal discomfort.
Initial evaluation revealed recurrent AP complicated by large-volume of pancreatic ascites (per fluid analysis) likely due to PD leak. Octreotide was initiated, and ERCP was attempted 5 days after admission (Fig1). However, severe papillary edema and congestion precluded ampullary identification, and the procedure was aborted.
The patient’s abdominal pain worsened, and repeat CT revealed necrotizing pancreatitis of the head and uncinate process. A 2nd ERCP was attempted a week later. It demonstrated progressive duodenal edema and narrowing of the 1st portion of the duodenum, causing benign GOO, preventing passage of the side-viewing scope. A forward-viewing scope reached the 2nd portion of the duodenum, but the papilla remained unvisualized and ERCP was aborted.
The 3rd ERCP attempted successful PD stenting was achieved using an underwater technique with a forward-viewing scope (Fig. 2). The patient required multiple paracentesis and was found to have infected ascitic fluid for which he started antibiotics. However, due to the presence of loculated intraabdominal fluid collections inaccessible to interventional radiology, the patient underwent exploratory laparoscopy with JP drain placement. Over time, the patient showed continued improvement, allowing for drain removal and successful PD stent extraction without evidence of recurrent leak.
Discussion: ERCP during AP is technically challenging due to inflammation and edema in the region of the biliary and pancreatic ducts. In this case, severe duodenal inflammation resulted in luminal stenosis and functional obstruction, preventing visualization of the major papilla. The use of underwater endoscopy techniques has increasingly demonstrated utility in enhancing both diagnostic and therapeutic endoscopic procedures. In this patient, underwater visualization improved duodenal distension and allowed the folds to float, which aided in the identification of the papilla in spite of the severe edema.
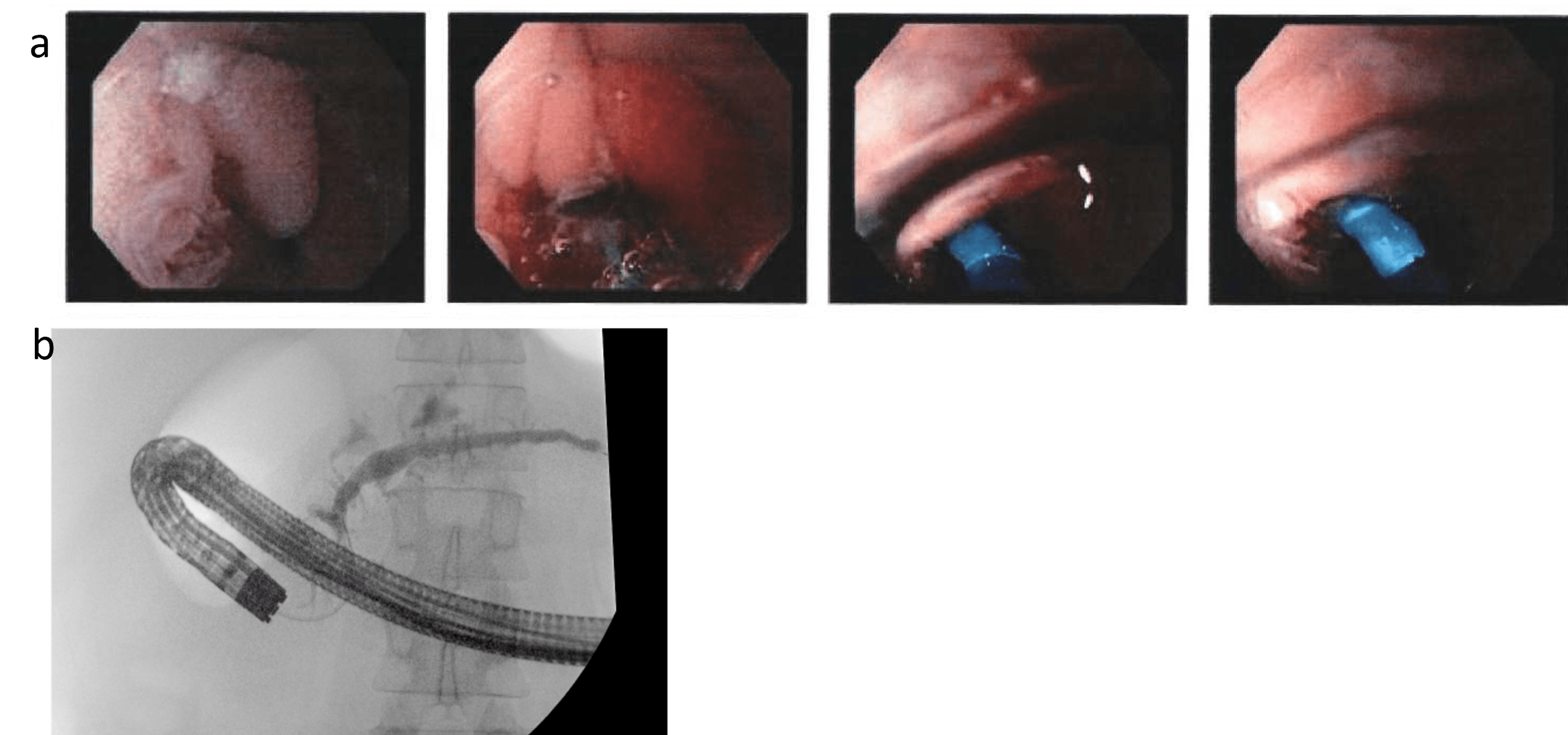
Figure: Hospital course timeline
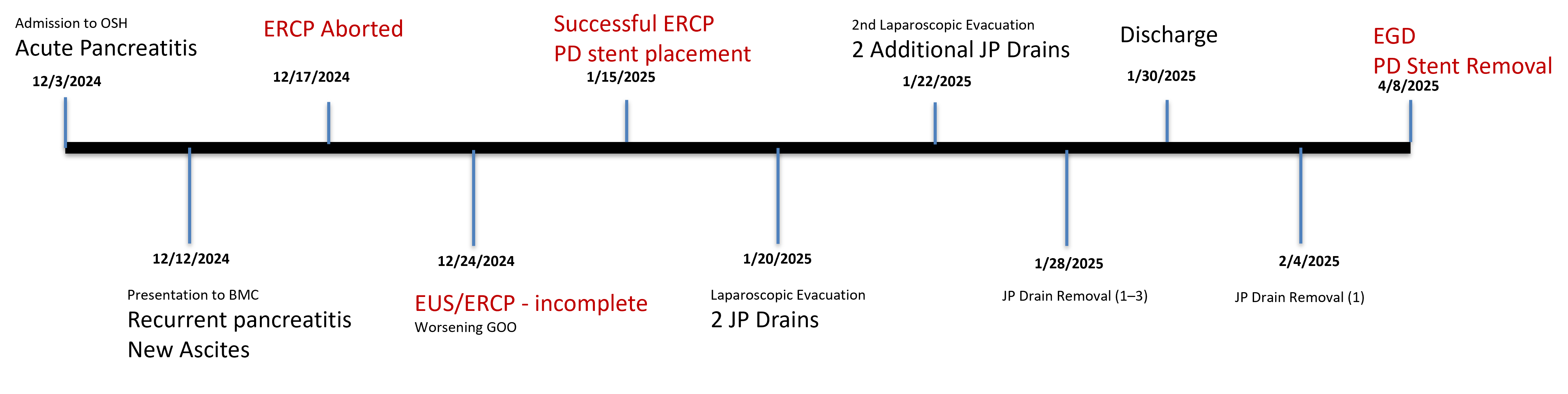
Figure: (a) A serial endoscopic image demonstrating edema and congestion in the second part of the duodenum. The ampulla is visualized underwater, before and after PD stent placement
(b) Fluoroscopic image revealing multifocal pancreatic duct leak, primary at the head and neck.
Disclosures:
Cristina Batarseh indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Tushaar Shrimanker indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Tiago Martins indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Cristina Batarseh, MD, Aizaz Khan, MD, Tushaar Shrimanker, MD, Syed Hamza Sohail, MD, Tiago Martins, DO, Kevin Groudan, MD, Nha Duong, DO. P5731 - Innovative Use of Underwater Technique to Facilitate ERCP in the Setting of Anatomic and Inflammatory Barriers in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Massachusetts Chan Medical School - Baystate Health, Springfield, MA
Introduction: We present a case of complicated acute pancreatitis (AP) characterized by a pancreatic duct (PD) leak and gastric outlet obstruction (GOO) secondary to extrinsic compression from peripancreatic fluid and duodenal edema, creating a significant technical challenge for endoscopic retrograde cholangiopancreatography (ERCP).
Case Description/
Methods: Our patient is a 43-year-old M with a history of alcohol use and multiple prior admissions for uncomplicated AP, who presented with a 6 days of nausea, vomiting, and abdominal discomfort.
Initial evaluation revealed recurrent AP complicated by large-volume of pancreatic ascites (per fluid analysis) likely due to PD leak. Octreotide was initiated, and ERCP was attempted 5 days after admission (Fig1). However, severe papillary edema and congestion precluded ampullary identification, and the procedure was aborted.
The patient’s abdominal pain worsened, and repeat CT revealed necrotizing pancreatitis of the head and uncinate process. A 2nd ERCP was attempted a week later. It demonstrated progressive duodenal edema and narrowing of the 1st portion of the duodenum, causing benign GOO, preventing passage of the side-viewing scope. A forward-viewing scope reached the 2nd portion of the duodenum, but the papilla remained unvisualized and ERCP was aborted.
The 3rd ERCP attempted successful PD stenting was achieved using an underwater technique with a forward-viewing scope (Fig. 2). The patient required multiple paracentesis and was found to have infected ascitic fluid for which he started antibiotics. However, due to the presence of loculated intraabdominal fluid collections inaccessible to interventional radiology, the patient underwent exploratory laparoscopy with JP drain placement. Over time, the patient showed continued improvement, allowing for drain removal and successful PD stent extraction without evidence of recurrent leak.
Discussion: ERCP during AP is technically challenging due to inflammation and edema in the region of the biliary and pancreatic ducts. In this case, severe duodenal inflammation resulted in luminal stenosis and functional obstruction, preventing visualization of the major papilla. The use of underwater endoscopy techniques has increasingly demonstrated utility in enhancing both diagnostic and therapeutic endoscopic procedures. In this patient, underwater visualization improved duodenal distension and allowed the folds to float, which aided in the identification of the papilla in spite of the severe edema.
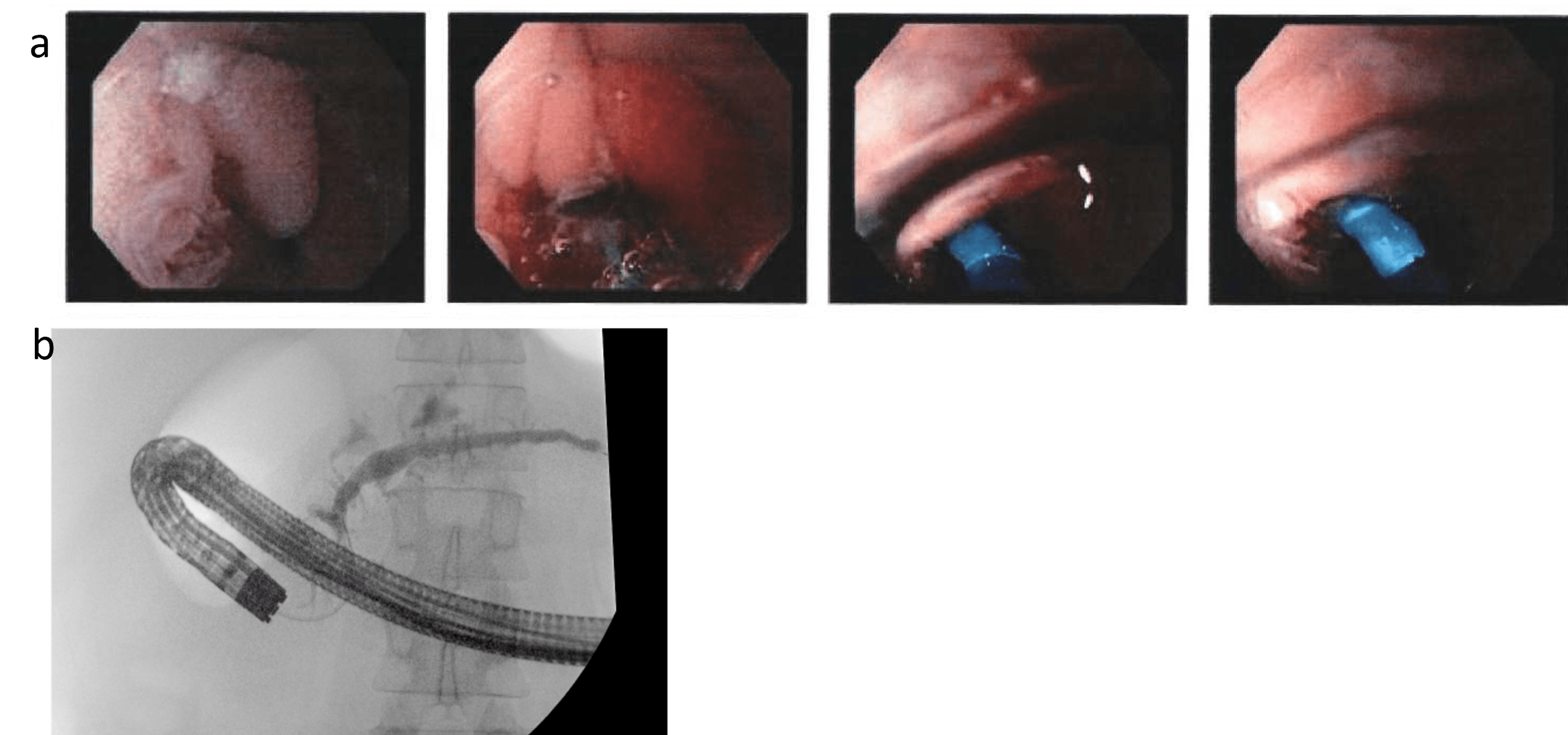
Figure: Hospital course timeline
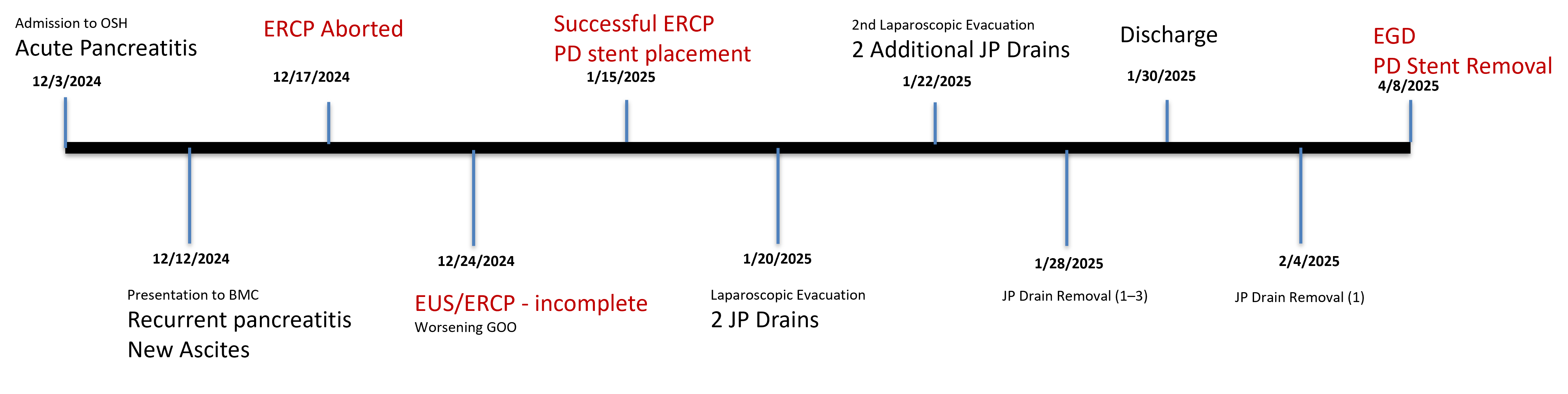
Figure: (a) A serial endoscopic image demonstrating edema and congestion in the second part of the duodenum. The ampulla is visualized underwater, before and after PD stent placement
(b) Fluoroscopic image revealing multifocal pancreatic duct leak, primary at the head and neck.
Disclosures:
Cristina Batarseh indicated no relevant financial relationships.
Aizaz Khan indicated no relevant financial relationships.
Tushaar Shrimanker indicated no relevant financial relationships.
Syed Hamza Sohail indicated no relevant financial relationships.
Tiago Martins indicated no relevant financial relationships.
Kevin Groudan indicated no relevant financial relationships.
Nha Duong indicated no relevant financial relationships.
Cristina Batarseh, MD, Aizaz Khan, MD, Tushaar Shrimanker, MD, Syed Hamza Sohail, MD, Tiago Martins, DO, Kevin Groudan, MD, Nha Duong, DO. P5731 - Innovative Use of Underwater Technique to Facilitate ERCP in the Setting of Anatomic and Inflammatory Barriers in Acute Pancreatitis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
