Tuesday Poster Session
Category: Interventional Endoscopy
P5717 - Life-Threatening Hemorrhage From a Gastroduodenal Artery Pseudoaneurysm Following LAMS Placement for a Pancreatic Pseudocyst
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vishnu Yanamaladoddi, MD
Creighton University School of Medicine
Phoenix, AZ
Presenting Author(s)
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Ariana R. Tagliaferri, MD1, Sunny Kumar, MD2, Danlu Wang, DO1, Indu Srinivasan, MD1
1Creighton University School of Medicine, Phoenix, AZ; 2Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Pancreatic pseudocysts are a common complication following acute or chronic pancreatitis. For symptomatic and persistent pseudocysts, endoscopic ultrasound (EUS)-guided drainage, typically via cystogastrostomy, is the first-line therapy. It involves the placement of a lumen-apposing metal stent (LAMS) to drain the fluid collection, and is usually removed after a few weeks. Bleeding is a known complication of LAMS placement, occurring in approximately 7-10% of cases. One potential source of bleeding is a visceral artery pseudoaneurysm. We present a case of a young female who developed hematemesis from a gastroduodenal artery pseudoaneurysm one day after LAMS placement.
Case Description/
Methods: A 28-year-old female with a history of trauma-induced pancreatitis and recurrent pancreatic pseudocysts was found unresponsive with hematemesis shortly after discharge from an outside hospital. She had recently undergone EUS-guided cystogastrostomy with LAMS placement for a recurrent pseudocyst. Her initial pancreatitis was months earlier after blunt abdominal trauma. A pseudocyst was previously drained with LAMS, which was removed after resolution. However, recurrence of symptoms led to a second stent placement.
On arrival, she was somnolent and hypotensive (BP 62/31 mmHg, HR 130–140 bpm), with blood in the oropharynx. CT angiogram revealed active contrast extravasation into a pseudocyst and a bleeding gastroduodenal artery (GDA) pseudoaneurysm. She underwent emergent embolization of the GDA and supraduodenal artery.
Post-procedure imaging confirmed successful embolization with no active bleeding. A 7.4 cm pseudocyst with hemorrhagic contents was identified in the pancreatic head. The patient was stabilized and transferred to the original treating hospital for hepatobiliary surgical evaluation.
Discussion: With the increasing use of LAMS for pancreatic pseudocyst drainage, it is important to recognize rare but serious complications like delayed bleeding from a visceral artery pseudoaneurysm. In this case, a GDA pseudoaneurysm likely developed after the first cystogastrostomy, possibly due to stent-related erosion or local inflammation, and then ruptured following a second LAMS placement leading to life-threatening hematemesis. Prompt diagnosis with angiography and emergent embolization was key to manage the bleed. As LAMS use becomes more widespread, particularly in recurrent or complex cases, clinicians should be aware of potential vascular complications and act promptly at the first sign of bleeding.
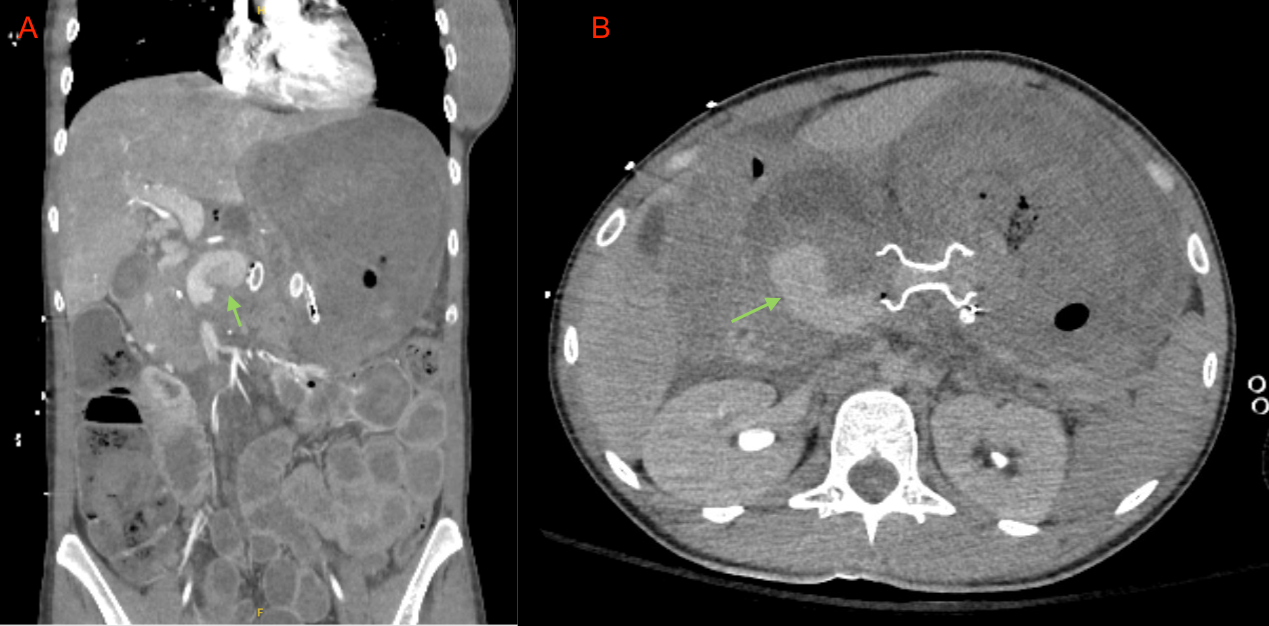
Figure: 1A - Coronal plane of CT abdomen showing gastroduodenal artery pseudoaneurysm
1B - Axial plane of CT abdomen showing gastroduodenal artery pseudoaneurysm and lumen apposing metallic stent (LAMS) connecting stomach and pseudocyst
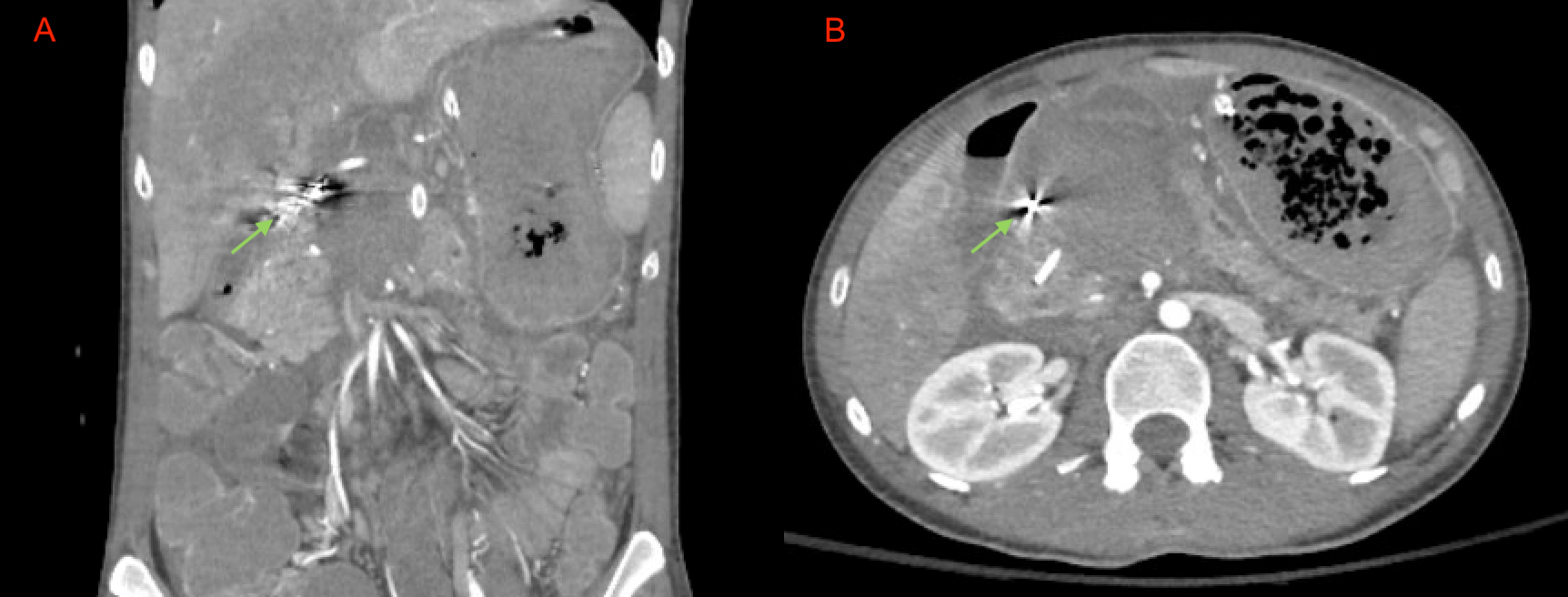
Figure: 2A - Coronal plane of CT abdomen post embolization showing persistent pseudocyst filled with hemorrhagic material without active extravasation
2B - Axial plane post embolization
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Ariana Tagliaferri indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Danlu Wang indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Ariana R. Tagliaferri, MD1, Sunny Kumar, MD2, Danlu Wang, DO1, Indu Srinivasan, MD1. P5717 - Life-Threatening Hemorrhage From a Gastroduodenal Artery Pseudoaneurysm Following LAMS Placement for a Pancreatic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Creighton University School of Medicine, Phoenix, AZ; 2Wright Center for Graduate Medical Education, Scranton, PA
Introduction: Pancreatic pseudocysts are a common complication following acute or chronic pancreatitis. For symptomatic and persistent pseudocysts, endoscopic ultrasound (EUS)-guided drainage, typically via cystogastrostomy, is the first-line therapy. It involves the placement of a lumen-apposing metal stent (LAMS) to drain the fluid collection, and is usually removed after a few weeks. Bleeding is a known complication of LAMS placement, occurring in approximately 7-10% of cases. One potential source of bleeding is a visceral artery pseudoaneurysm. We present a case of a young female who developed hematemesis from a gastroduodenal artery pseudoaneurysm one day after LAMS placement.
Case Description/
Methods: A 28-year-old female with a history of trauma-induced pancreatitis and recurrent pancreatic pseudocysts was found unresponsive with hematemesis shortly after discharge from an outside hospital. She had recently undergone EUS-guided cystogastrostomy with LAMS placement for a recurrent pseudocyst. Her initial pancreatitis was months earlier after blunt abdominal trauma. A pseudocyst was previously drained with LAMS, which was removed after resolution. However, recurrence of symptoms led to a second stent placement.
On arrival, she was somnolent and hypotensive (BP 62/31 mmHg, HR 130–140 bpm), with blood in the oropharynx. CT angiogram revealed active contrast extravasation into a pseudocyst and a bleeding gastroduodenal artery (GDA) pseudoaneurysm. She underwent emergent embolization of the GDA and supraduodenal artery.
Post-procedure imaging confirmed successful embolization with no active bleeding. A 7.4 cm pseudocyst with hemorrhagic contents was identified in the pancreatic head. The patient was stabilized and transferred to the original treating hospital for hepatobiliary surgical evaluation.
Discussion: With the increasing use of LAMS for pancreatic pseudocyst drainage, it is important to recognize rare but serious complications like delayed bleeding from a visceral artery pseudoaneurysm. In this case, a GDA pseudoaneurysm likely developed after the first cystogastrostomy, possibly due to stent-related erosion or local inflammation, and then ruptured following a second LAMS placement leading to life-threatening hematemesis. Prompt diagnosis with angiography and emergent embolization was key to manage the bleed. As LAMS use becomes more widespread, particularly in recurrent or complex cases, clinicians should be aware of potential vascular complications and act promptly at the first sign of bleeding.
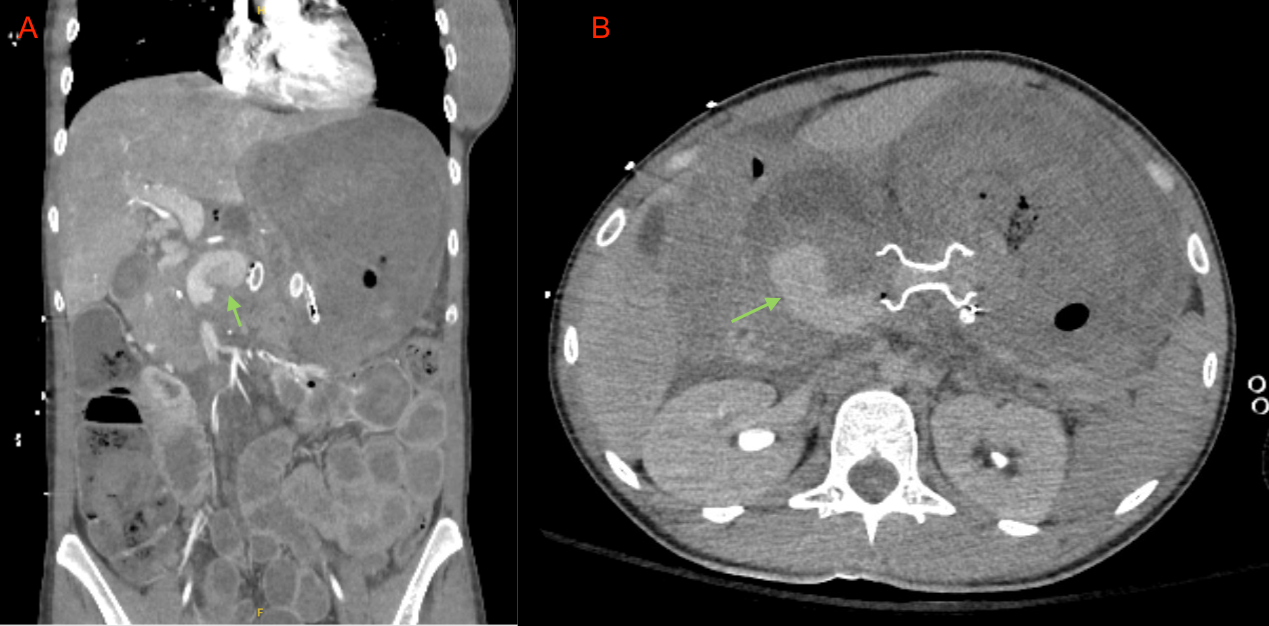
Figure: 1A - Coronal plane of CT abdomen showing gastroduodenal artery pseudoaneurysm
1B - Axial plane of CT abdomen showing gastroduodenal artery pseudoaneurysm and lumen apposing metallic stent (LAMS) connecting stomach and pseudocyst
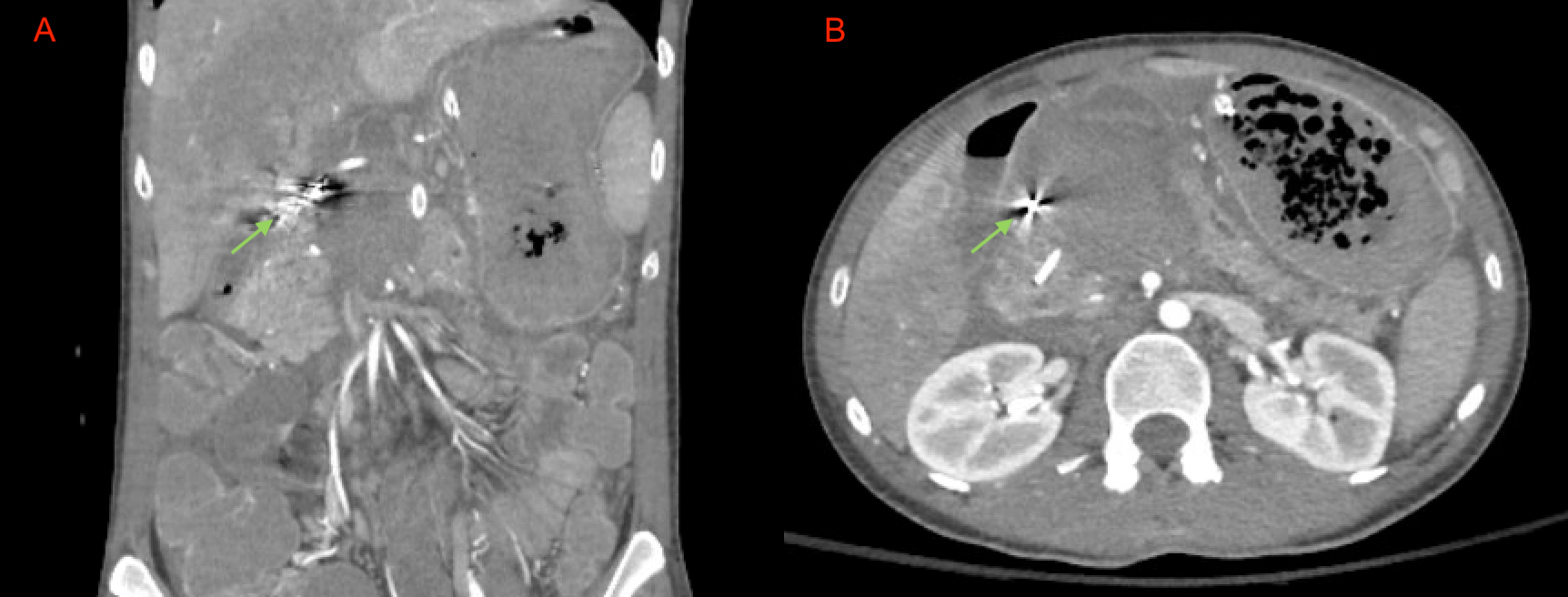
Figure: 2A - Coronal plane of CT abdomen post embolization showing persistent pseudocyst filled with hemorrhagic material without active extravasation
2B - Axial plane post embolization
Disclosures:
Vishnu Yanamaladoddi indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Ariana Tagliaferri indicated no relevant financial relationships.
Sunny Kumar indicated no relevant financial relationships.
Danlu Wang indicated no relevant financial relationships.
Indu Srinivasan indicated no relevant financial relationships.
Vishnu Yanamaladoddi, MD1, Vikash Kumar, MD1, Ariana R. Tagliaferri, MD1, Sunny Kumar, MD2, Danlu Wang, DO1, Indu Srinivasan, MD1. P5717 - Life-Threatening Hemorrhage From a Gastroduodenal Artery Pseudoaneurysm Following LAMS Placement for a Pancreatic Pseudocyst, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
