Tuesday Poster Session
Category: Interventional Endoscopy
P5708 - A Rare Case of Duodenal Perforation After ERCP: Recognizing and Managing Biliary Stent-Related Injury
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Hasan Jaber, MD (he/him/his)
University of Kansas School of Medicine
Wichita, KS
Presenting Author(s)
Hasan Jaber, MD1, Sandra Chehayeb, MD1, Stephanie J. Melquist, MD, MPH2, William J.. Salyers, MD, MPH3
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine-Wichita, Wichita, KS; 3University of Kansas School of Medicine - Wichita, Wichita, KS
Introduction: Duodenal perforation is a rare but potentially fatal complication of biliary stenting during endoscopic retrograde cholangiopancreatography (ERCP). We present a case of dual perforation within 12 hours of insertion, managed non-surgically.
Case Description/
Methods: An 80-year-old female with no significant medical history presented to the emergency department (ED) with worsening right-sided abdominal pain radiating to the back. She had undergone ERCP the day prior for evaluation of biliary ductal dilation, which revealed severe common hepatic duct stricture and mild common bile duct narrowing concerning for cholangiocarcinoma. Two plastic biliary stents were placed, and cytology samples were obtained through brushings. Within 12 hours of discharge, she returned to the ED in a nauseated state with severe abdominal pain. Labs showed leukocytosis (WBC 14.5 × 10⁹/L). Non-contrast CT abdomen revealed retroperitoneal free air and inflammatory stranding with fluid in the right abdomen, and the stents abutting the duodenum—raising concern for duodenal perforation. She was made NPO and started on IV fluids, proton pump inhibitors, and piperacillin-tazobactam. Esophagogastroduodenoscopy (EGD) revealed two plastic biliary stents with their distal tips embedded in the opposing wall of the second portion of the duodenum. The stents were removed through the scope, after which two punctate, non-bleeding duodenal perforations became clearly visible. Endoscopic closure was successfully performed using eight MANTIS clips—three at one site and five at the other. A nasoenteric tube was placed, and CT-guided drainage of a right lower quadrant fluid collection was performed, with placement of a 10 Fr pigtail catheter. The patient gradually improved with resolution of pain and leukocytosis after endoscopic closure and drainage.
Discussion: Duodenal perforation occurs in less than 1% of ERCP procedures. Stent-induced perforation is even rarer, and dual perforations are exceptional. Our patient presented within 12 hours of ERCP with severe abdominal pain, prompting imaging. Due to early identification, hemodynamic stability, and absence of diffuse peritonitis, surgical intervention was deferred. Both perforations were managed endoscopically with clip closure after stent removal. She improved rapidly, and follow-up imaging showed no residual collection or leak.This case underscores the importance of early recognition and demonstrates that endoscopic closure can be a safe, minimally invasive alternative to surgery
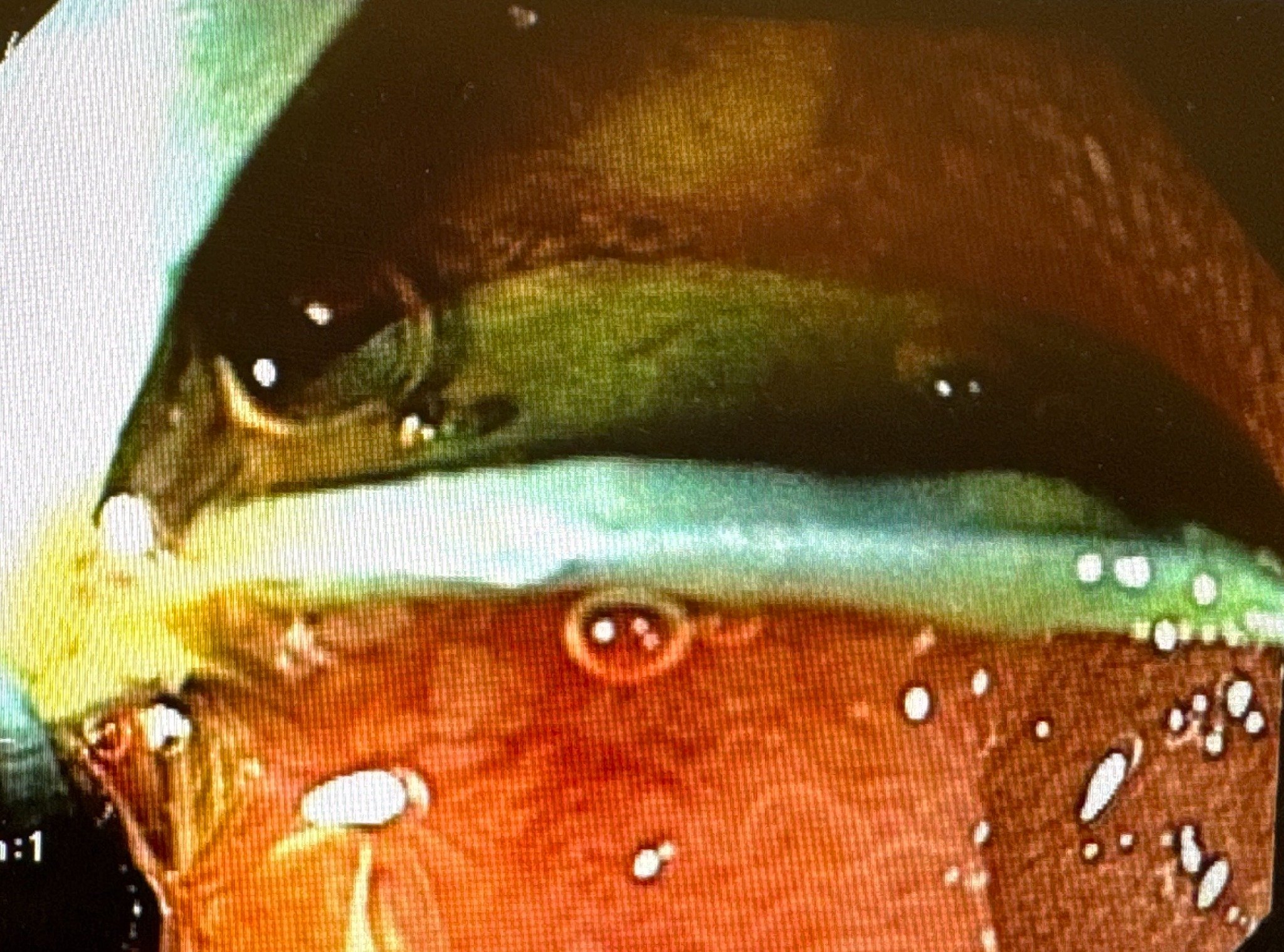
Figure: Distal tips of the stents embedded in the opposing wall of the second portion of the duodenum.
Disclosures:
Hasan Jaber indicated no relevant financial relationships.
Sandra Chehayeb indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Hasan Jaber, MD1, Sandra Chehayeb, MD1, Stephanie J. Melquist, MD, MPH2, William J.. Salyers, MD, MPH3. P5708 - A Rare Case of Duodenal Perforation After ERCP: Recognizing and Managing Biliary Stent-Related Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kansas School of Medicine, Wichita, KS; 2University of Kansas School of Medicine-Wichita, Wichita, KS; 3University of Kansas School of Medicine - Wichita, Wichita, KS
Introduction: Duodenal perforation is a rare but potentially fatal complication of biliary stenting during endoscopic retrograde cholangiopancreatography (ERCP). We present a case of dual perforation within 12 hours of insertion, managed non-surgically.
Case Description/
Methods: An 80-year-old female with no significant medical history presented to the emergency department (ED) with worsening right-sided abdominal pain radiating to the back. She had undergone ERCP the day prior for evaluation of biliary ductal dilation, which revealed severe common hepatic duct stricture and mild common bile duct narrowing concerning for cholangiocarcinoma. Two plastic biliary stents were placed, and cytology samples were obtained through brushings. Within 12 hours of discharge, she returned to the ED in a nauseated state with severe abdominal pain. Labs showed leukocytosis (WBC 14.5 × 10⁹/L). Non-contrast CT abdomen revealed retroperitoneal free air and inflammatory stranding with fluid in the right abdomen, and the stents abutting the duodenum—raising concern for duodenal perforation. She was made NPO and started on IV fluids, proton pump inhibitors, and piperacillin-tazobactam. Esophagogastroduodenoscopy (EGD) revealed two plastic biliary stents with their distal tips embedded in the opposing wall of the second portion of the duodenum. The stents were removed through the scope, after which two punctate, non-bleeding duodenal perforations became clearly visible. Endoscopic closure was successfully performed using eight MANTIS clips—three at one site and five at the other. A nasoenteric tube was placed, and CT-guided drainage of a right lower quadrant fluid collection was performed, with placement of a 10 Fr pigtail catheter. The patient gradually improved with resolution of pain and leukocytosis after endoscopic closure and drainage.
Discussion: Duodenal perforation occurs in less than 1% of ERCP procedures. Stent-induced perforation is even rarer, and dual perforations are exceptional. Our patient presented within 12 hours of ERCP with severe abdominal pain, prompting imaging. Due to early identification, hemodynamic stability, and absence of diffuse peritonitis, surgical intervention was deferred. Both perforations were managed endoscopically with clip closure after stent removal. She improved rapidly, and follow-up imaging showed no residual collection or leak.This case underscores the importance of early recognition and demonstrates that endoscopic closure can be a safe, minimally invasive alternative to surgery
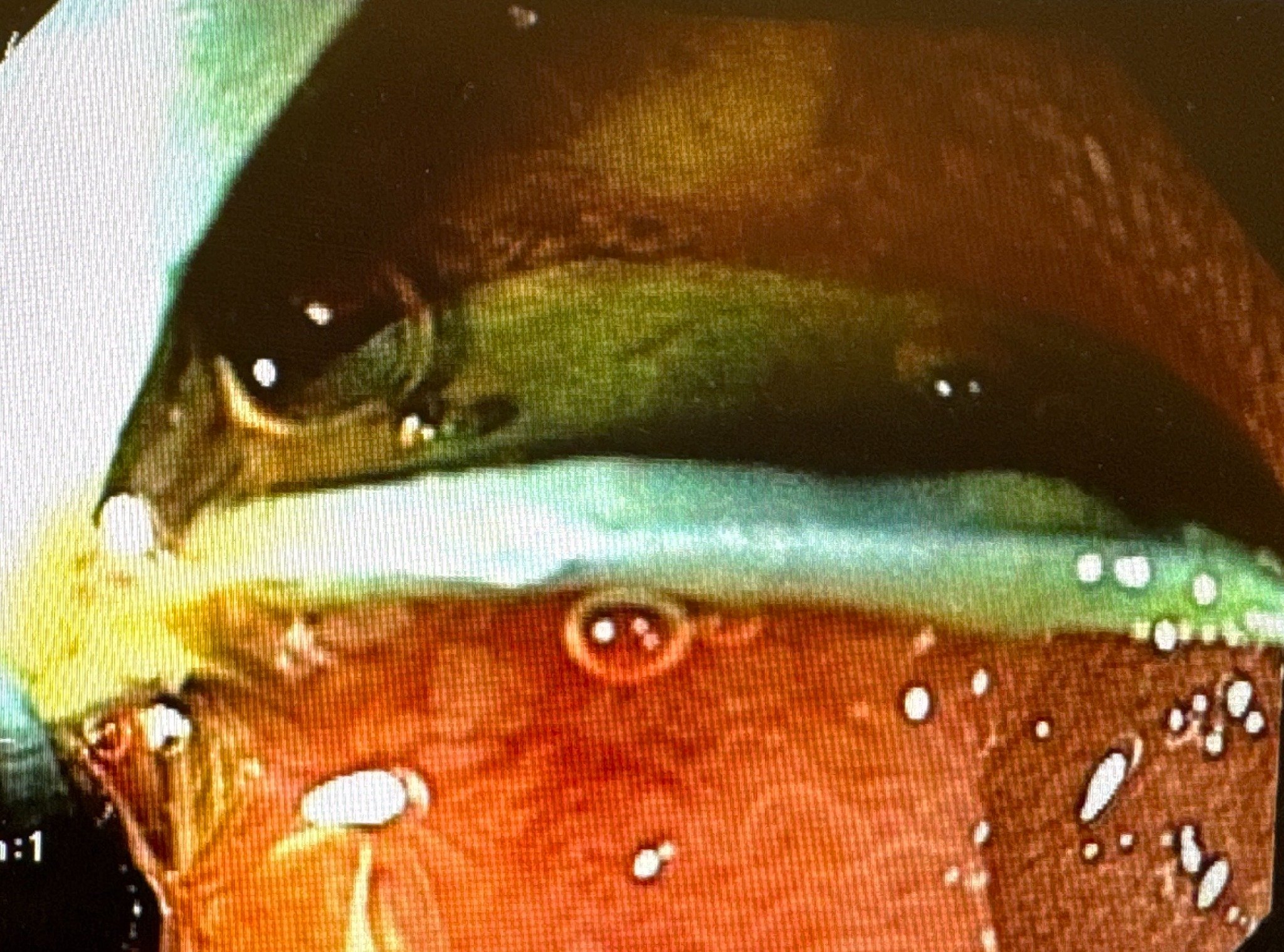
Figure: Distal tips of the stents embedded in the opposing wall of the second portion of the duodenum.
Disclosures:
Hasan Jaber indicated no relevant financial relationships.
Sandra Chehayeb indicated no relevant financial relationships.
Stephanie Melquist indicated no relevant financial relationships.
William Salyers indicated no relevant financial relationships.
Hasan Jaber, MD1, Sandra Chehayeb, MD1, Stephanie J. Melquist, MD, MPH2, William J.. Salyers, MD, MPH3. P5708 - A Rare Case of Duodenal Perforation After ERCP: Recognizing and Managing Biliary Stent-Related Injury, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

