Tuesday Poster Session
Category: Interventional Endoscopy
P5688 - No July Effect on Timing of ERCP for Acute Cholangitis in Teaching Hospitals
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Joseph A. Atarere, MBChB, MPH
MedStar Georgetown University Hospital
Baltimore, MD
Presenting Author(s)
Joseph A. Atarere, MBChB, MPH1, Chisom Nwaneki, MD2, Boniface Mensah, MBChB, MPh1, Sarpong Boateng, MD, MPH3, Eugene Annor, MD, MPH4, Seunghee Han, MBChB1, Kevin Eid, MD1, Michele Ryan, MS5, Christopher Thompson, MD, MS5
1MedStar Georgetown University Hospital, Baltimore, MD; 2Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 3Yale New Haven Health, Bridgeport, CT; 4University of Illinois College of Medicine, Morton, IL; 5Brigham and Women's Hospital, Boston, MA
Introduction: Early recognition and drainage with endoscopic retrograde cholangiopancreatography (ERCP) can reduce complications from acute cholangitis. The transition of medical trainees at the beginning of the academic year, known as the 'July effect', has been associated with worse clinical outcomes in various conditions, but it has not been thoroughly studied in patients with acute cholangitis. In this study, we assessed the July effect on the timing of ERCP for patients with acute cholangitis admitted to teaching hospitals.
Methods: We analyzed retrospective data from the 2016 to 2020 iterations of the Nationwide Inpatient Sample (NIS). We included adult admissions to teaching hospitals for acute cholangitis between May and September. The primary outcome was the timing of ERCP, categorized as urgent (within ≤48 hours) vs. non-urgent ( >48 hours). The primary variable of interest was the month of admission: May to June vs. July to September. We described the study population characteristics using chi-squared tests and examined the relationship between the month of admission and ERCP timing using multivariable logistic regression.
Results: The study included 2,436 patients, with 48.8% (1,325) admitted between April and June and 51.2% (1,247) between July and September. Most patients were female (54.5%), White (70.4%), at least 65 years old (64.1%), and admitted to large hospitals (55.6%). The majority (84.6%) underwent ERCP within 48 hours of admission. After adjusting for covariates, there was no significant difference in ERCP timing based on the month of admission [OR 0.99, 95% CI (0.76, 1.29)]. Patients with comorbid illnesses and those admitted during the weekend [OR 0.62, 95% CI (0.46, 0.83)] were however less likely to undergo urgent ERCP.
Discussion: Delays in timely ERCP are associated with worse clinical outcomes. Our study found no difference in ERCP timing (urgent vs. non-urgent) by time of year in teaching hospitals. In patients with comorbid illness, procedure delay may be warranted. The weekend effect on urgent ERCP has been noted, but its impact on mortality requires further evaluation.
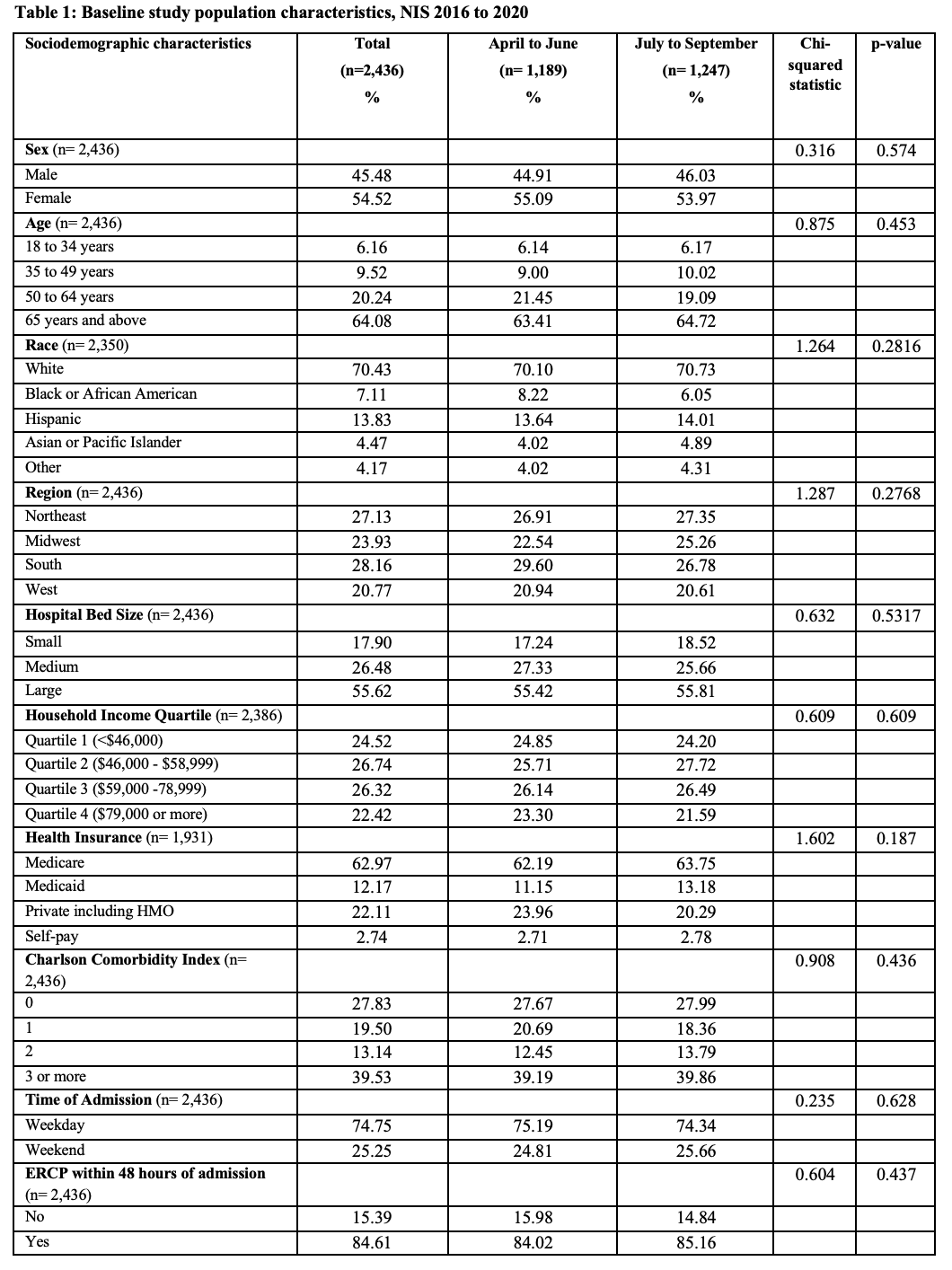
Figure: Table 1:

Figure: Figure 1
Disclosures:
Joseph Atarere indicated no relevant financial relationships.
Chisom Nwaneki indicated no relevant financial relationships.
Boniface Mensah indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Eugene Annor indicated no relevant financial relationships.
Seunghee Han indicated no relevant financial relationships.
Kevin Eid indicated no relevant financial relationships.
Michele Ryan indicated no relevant financial relationships.
Christopher Thompson indicated no relevant financial relationships.
Joseph A. Atarere, MBChB, MPH1, Chisom Nwaneki, MD2, Boniface Mensah, MBChB, MPh1, Sarpong Boateng, MD, MPH3, Eugene Annor, MD, MPH4, Seunghee Han, MBChB1, Kevin Eid, MD1, Michele Ryan, MS5, Christopher Thompson, MD, MS5. P5688 - No July Effect on Timing of ERCP for Acute Cholangitis in Teaching Hospitals, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1MedStar Georgetown University Hospital, Baltimore, MD; 2Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 3Yale New Haven Health, Bridgeport, CT; 4University of Illinois College of Medicine, Morton, IL; 5Brigham and Women's Hospital, Boston, MA
Introduction: Early recognition and drainage with endoscopic retrograde cholangiopancreatography (ERCP) can reduce complications from acute cholangitis. The transition of medical trainees at the beginning of the academic year, known as the 'July effect', has been associated with worse clinical outcomes in various conditions, but it has not been thoroughly studied in patients with acute cholangitis. In this study, we assessed the July effect on the timing of ERCP for patients with acute cholangitis admitted to teaching hospitals.
Methods: We analyzed retrospective data from the 2016 to 2020 iterations of the Nationwide Inpatient Sample (NIS). We included adult admissions to teaching hospitals for acute cholangitis between May and September. The primary outcome was the timing of ERCP, categorized as urgent (within ≤48 hours) vs. non-urgent ( >48 hours). The primary variable of interest was the month of admission: May to June vs. July to September. We described the study population characteristics using chi-squared tests and examined the relationship between the month of admission and ERCP timing using multivariable logistic regression.
Results: The study included 2,436 patients, with 48.8% (1,325) admitted between April and June and 51.2% (1,247) between July and September. Most patients were female (54.5%), White (70.4%), at least 65 years old (64.1%), and admitted to large hospitals (55.6%). The majority (84.6%) underwent ERCP within 48 hours of admission. After adjusting for covariates, there was no significant difference in ERCP timing based on the month of admission [OR 0.99, 95% CI (0.76, 1.29)]. Patients with comorbid illnesses and those admitted during the weekend [OR 0.62, 95% CI (0.46, 0.83)] were however less likely to undergo urgent ERCP.
Discussion: Delays in timely ERCP are associated with worse clinical outcomes. Our study found no difference in ERCP timing (urgent vs. non-urgent) by time of year in teaching hospitals. In patients with comorbid illness, procedure delay may be warranted. The weekend effect on urgent ERCP has been noted, but its impact on mortality requires further evaluation.
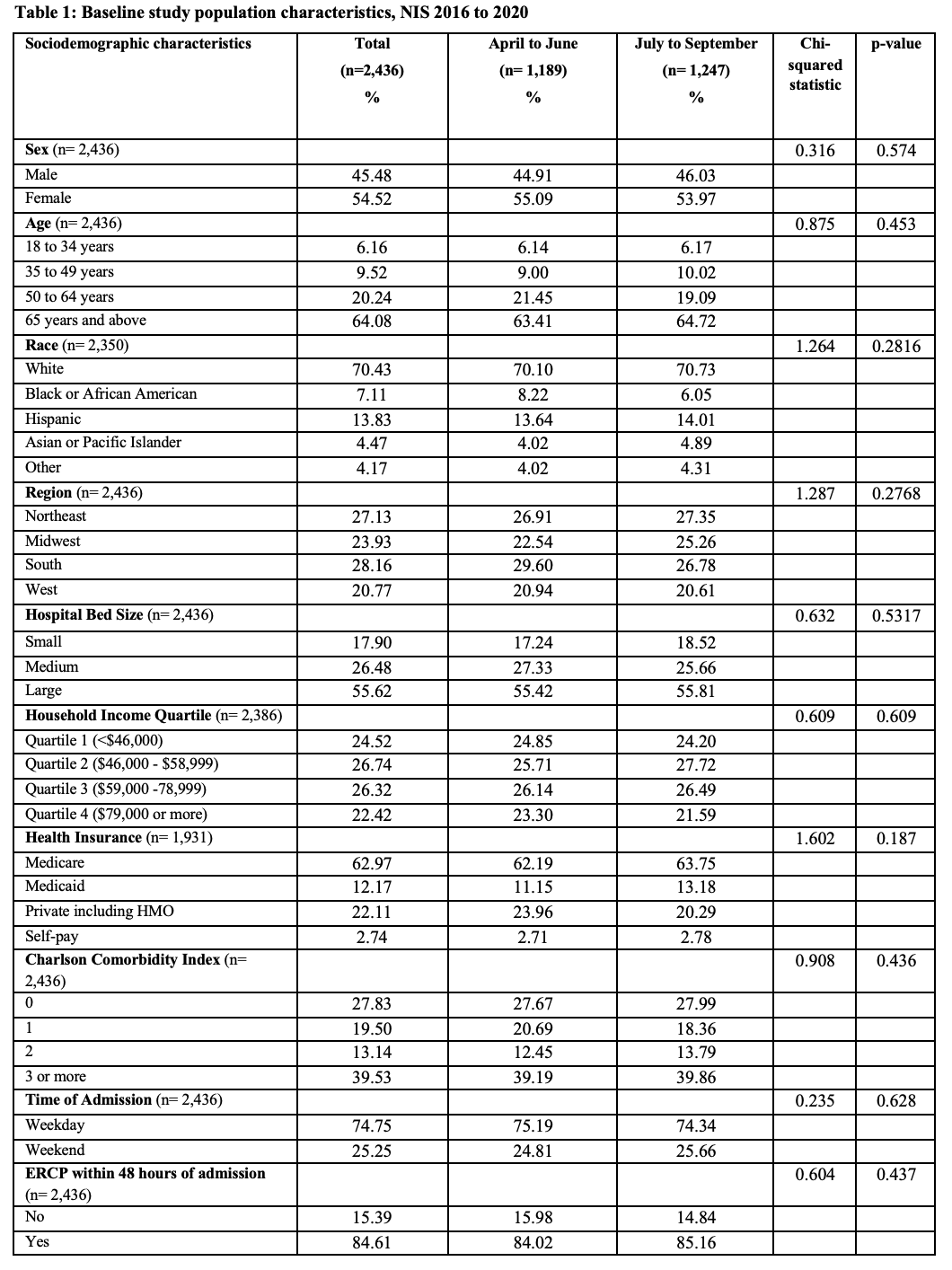
Figure: Table 1:

Figure: Figure 1
Disclosures:
Joseph Atarere indicated no relevant financial relationships.
Chisom Nwaneki indicated no relevant financial relationships.
Boniface Mensah indicated no relevant financial relationships.
Sarpong Boateng indicated no relevant financial relationships.
Eugene Annor indicated no relevant financial relationships.
Seunghee Han indicated no relevant financial relationships.
Kevin Eid indicated no relevant financial relationships.
Michele Ryan indicated no relevant financial relationships.
Christopher Thompson indicated no relevant financial relationships.
Joseph A. Atarere, MBChB, MPH1, Chisom Nwaneki, MD2, Boniface Mensah, MBChB, MPh1, Sarpong Boateng, MD, MPH3, Eugene Annor, MD, MPH4, Seunghee Han, MBChB1, Kevin Eid, MD1, Michele Ryan, MS5, Christopher Thompson, MD, MS5. P5688 - No July Effect on Timing of ERCP for Acute Cholangitis in Teaching Hospitals, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
