Tuesday Poster Session
Category: Interventional Endoscopy
P5683 - Endoscopic Retrograde Cholangiopancreatography in Patients With Heart Failure and Pulmonary Hypertension: A Nationwide, Volume Outcome Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chukwunonso Ezeani, MBBS
Mayo Clinic
Phoenix, AZ
Presenting Author(s)
Chukwunonso Ezeani, MBBS1, Lekhya Kollu, BA2, Oyedotun Babajide, MD3, Bishoy Lawendy, MD4, Chukwuemeka Ogbu, MD, MPH5, Muni Rubens, Bsc6, Philip Okafor, MD, MPH, FACG7
1Mayo Clinic, Phoenix, AZ; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3NYC Health + Hospitals/Metropolitan, New York, NY; 4University of Western Ontario, London, ON, Canada; 5Cape Fear valley Medical Center, Fayetteville, NC; 6Miami Cancer Institute, Miami, FL; 7Mayo Clinic, Jacksonville, FL
Introduction: Heart failure (HF) and pulmonary hypertension (PH) are high-risk cardiopulmonary conditions historically associated with worse outcomes. However, there is a paucity of data for patients with HF or PH undergoing Endoscopic Retrograde Cholangiopancreatography (ERCP). We performed a retrospective analysis of outcomes among inpatients with high-risk cardiopulmonary disease undergoing ERCP using a national database and explored the interaction with hospital volume for patients with HF and PH.
Methods: Patients with HF and/or PH who underwent ERCP between 2016 and 2021 were extracted from the National Inpatient Sample. Hospitals were stratified by quartiles (quartile 1 = lowest volume, quartile 4 = highest volume) based on the annual number of ERCPs done in patients with PH and HF. Multivariable regression analyses were used to compare outcomes by hospital volume (quartiles) after controlling for potential confounders. The primary outcome was all-cause inhospital mortality. Secondary outcomes included cardiac arrest and prolonged length of stay (LOS). Outcomes were reported as adjusted odds ratios (OR) and 95% confidence intervals (CI). A p-value of <0.05 was considered statistically significant.
Results: The cohort consisted of 81,725 patients with HF and PH who underwent ERCP during the study period. There was a higher proportion of females (55 vs 45%, p< 0.001). Among patients with PH and HF, the adjusted odds of death were highest in those treated at the lowest volume hospitals (quartile 1, OR 4.80 [3.33–6.98], p< 0.003) [Table 1]. The same trend was observed for cardiac arrest (quartile 1, OR 8.51 [5.94–12.26], p< 0.0001) and LOS (quartile 1, OR 3.32 [2.88–3.94], p< 0.0001). In the higher volume hospitals, no difference in mortality (quartile 3, OR 2.94 (0.95–8.82, p=0.14), (quartile 4, OR 1.82 (0.52–6.23, p=0.31), cardiac arrest (quartile 3, OR 4.88 (0.95–25.68, p=0.12) (quartile 4, OR 2.19 (0.4–11.26, p=0.32) or prolonged LOS (quartile 3, OR 2.24 (0.95–5.16, p=0.11) (quartile 4 OR 1.42 (0.55–3.91, p=0.29) were observed. Patients with either HF or PH had also had worse outcomes when treated at the lowest volume hospitals (Table 1).
Discussion: Patients with HF and PH undergoing inpatient ERCP at low-volume hospitals have worse outcomes compared to similar-risk patients treated at high-volume hospitals. The difference may be related to competency that develops from a higher volume of ERCPs and availability of specialty expertise such as cardiac anesthesia for these high-risk patients.
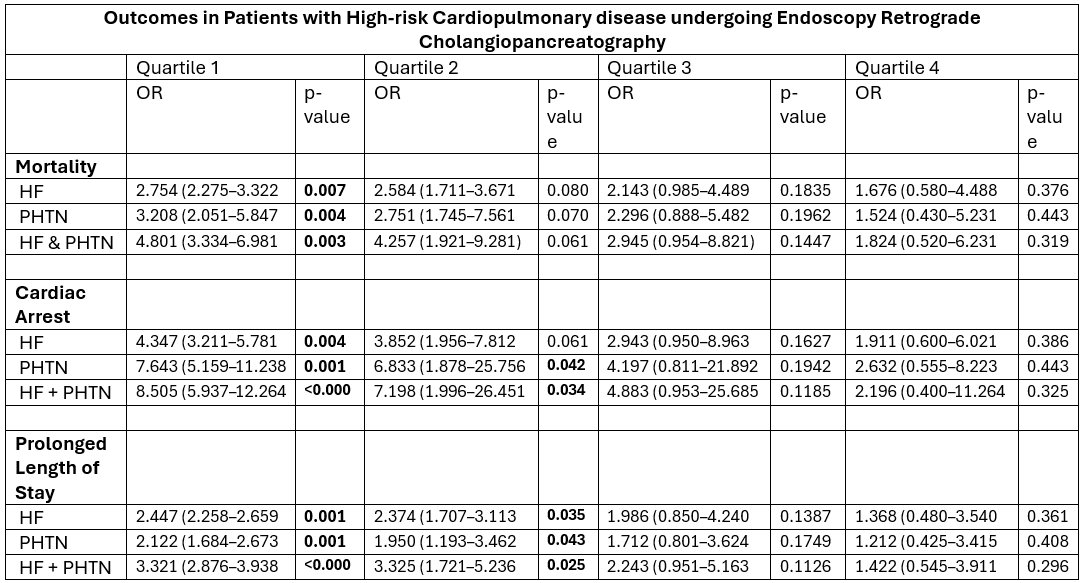
Figure: Table 1: Outcomes in Patients with High-risk Cardiopulmonary disease undergoing Endoscopy Retrograde Cholangiopancreatography
Disclosures:
Chukwunonso Ezeani indicated no relevant financial relationships.
Lekhya Kollu indicated no relevant financial relationships.
Oyedotun Babajide indicated no relevant financial relationships.
Bishoy Lawendy indicated no relevant financial relationships.
Chukwuemeka Ogbu indicated no relevant financial relationships.
Muni Rubens indicated no relevant financial relationships.
Philip Okafor indicated no relevant financial relationships.
Chukwunonso Ezeani, MBBS1, Lekhya Kollu, BA2, Oyedotun Babajide, MD3, Bishoy Lawendy, MD4, Chukwuemeka Ogbu, MD, MPH5, Muni Rubens, Bsc6, Philip Okafor, MD, MPH, FACG7. P5683 - Endoscopic Retrograde Cholangiopancreatography in Patients With Heart Failure and Pulmonary Hypertension: A Nationwide, Volume Outcome Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Phoenix, AZ; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3NYC Health + Hospitals/Metropolitan, New York, NY; 4University of Western Ontario, London, ON, Canada; 5Cape Fear valley Medical Center, Fayetteville, NC; 6Miami Cancer Institute, Miami, FL; 7Mayo Clinic, Jacksonville, FL
Introduction: Heart failure (HF) and pulmonary hypertension (PH) are high-risk cardiopulmonary conditions historically associated with worse outcomes. However, there is a paucity of data for patients with HF or PH undergoing Endoscopic Retrograde Cholangiopancreatography (ERCP). We performed a retrospective analysis of outcomes among inpatients with high-risk cardiopulmonary disease undergoing ERCP using a national database and explored the interaction with hospital volume for patients with HF and PH.
Methods: Patients with HF and/or PH who underwent ERCP between 2016 and 2021 were extracted from the National Inpatient Sample. Hospitals were stratified by quartiles (quartile 1 = lowest volume, quartile 4 = highest volume) based on the annual number of ERCPs done in patients with PH and HF. Multivariable regression analyses were used to compare outcomes by hospital volume (quartiles) after controlling for potential confounders. The primary outcome was all-cause inhospital mortality. Secondary outcomes included cardiac arrest and prolonged length of stay (LOS). Outcomes were reported as adjusted odds ratios (OR) and 95% confidence intervals (CI). A p-value of <0.05 was considered statistically significant.
Results: The cohort consisted of 81,725 patients with HF and PH who underwent ERCP during the study period. There was a higher proportion of females (55 vs 45%, p< 0.001). Among patients with PH and HF, the adjusted odds of death were highest in those treated at the lowest volume hospitals (quartile 1, OR 4.80 [3.33–6.98], p< 0.003) [Table 1]. The same trend was observed for cardiac arrest (quartile 1, OR 8.51 [5.94–12.26], p< 0.0001) and LOS (quartile 1, OR 3.32 [2.88–3.94], p< 0.0001). In the higher volume hospitals, no difference in mortality (quartile 3, OR 2.94 (0.95–8.82, p=0.14), (quartile 4, OR 1.82 (0.52–6.23, p=0.31), cardiac arrest (quartile 3, OR 4.88 (0.95–25.68, p=0.12) (quartile 4, OR 2.19 (0.4–11.26, p=0.32) or prolonged LOS (quartile 3, OR 2.24 (0.95–5.16, p=0.11) (quartile 4 OR 1.42 (0.55–3.91, p=0.29) were observed. Patients with either HF or PH had also had worse outcomes when treated at the lowest volume hospitals (Table 1).
Discussion: Patients with HF and PH undergoing inpatient ERCP at low-volume hospitals have worse outcomes compared to similar-risk patients treated at high-volume hospitals. The difference may be related to competency that develops from a higher volume of ERCPs and availability of specialty expertise such as cardiac anesthesia for these high-risk patients.
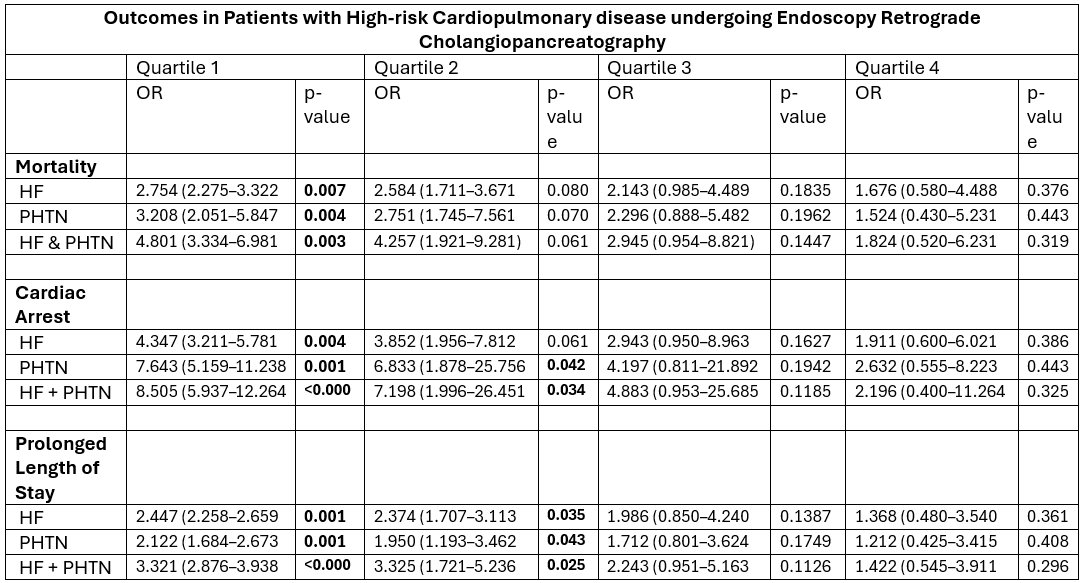
Figure: Table 1: Outcomes in Patients with High-risk Cardiopulmonary disease undergoing Endoscopy Retrograde Cholangiopancreatography
Disclosures:
Chukwunonso Ezeani indicated no relevant financial relationships.
Lekhya Kollu indicated no relevant financial relationships.
Oyedotun Babajide indicated no relevant financial relationships.
Bishoy Lawendy indicated no relevant financial relationships.
Chukwuemeka Ogbu indicated no relevant financial relationships.
Muni Rubens indicated no relevant financial relationships.
Philip Okafor indicated no relevant financial relationships.
Chukwunonso Ezeani, MBBS1, Lekhya Kollu, BA2, Oyedotun Babajide, MD3, Bishoy Lawendy, MD4, Chukwuemeka Ogbu, MD, MPH5, Muni Rubens, Bsc6, Philip Okafor, MD, MPH, FACG7. P5683 - Endoscopic Retrograde Cholangiopancreatography in Patients With Heart Failure and Pulmonary Hypertension: A Nationwide, Volume Outcome Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
