Tuesday Poster Session
Category: Interventional Endoscopy
P5661 - Primary Needle-Knife Fistulotomy Is an Effective and Safer Alternative to Conventional Cannulation in ERCP: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Saqr Alsakarneh, MD, MS (he/him/his)
Mayo Clinic
Rochester, MN
Presenting Author(s)
Saqr Alsakarneh, MD, MS1, Mohamad Adam, MD2, Razan Aburumman, MD3, Farah Khraisat, MD4, Mohammad Abuassi, MD5, Mahmoud Y. Madi, MD6, Bashar Qumseya, MD, MPH7
1Mayo Clinic, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Henry Ford Health, Detroit, MI; 4University of Florida, Jacksonville, FL; 5University of Central Florida, HCA Healthcare GME, Gainesville, FL; 6University of Texas at Austin Dell Medical School, Austin, TX; 7University of Florida College of Medicine, Gainesville, FL
Introduction: In patients at high risk for post-ERCP pancreatitis (PEP), conventional ERCP cannulation (CEC) carries a PEP risk of up to 14%. Primary needle-knife fistulotomy (pNKF) has emerged as an alternative technique, allowing selective biliary access while minimizing trauma to the papillary orifice. This meta-analysis aims to compare the efficacy and safety of pNKF versus CEC.
Methods: A systematic literature search was performed using PubMed, Scopus, Embase, and Web of Science through May 2025. Studies were included if they compared pNKF (as the primary access method) to CEC in biliary drainage. Studies using pNKF as rescue/salvage therapy were excluded. Pooled odds ratios (ORs) and mean differences (MDs) with 95% confidence intervals (CIs) were calculated using random-effects models and the Mantel-Haenszel method. Heterogeneity was assessed via the I² statistic. The primary outcome was PEP. Secondary outcomes included cannulation success, procedure time, and other adverse events.
Results: Our search strategy resulted in 1874 citations, of which, 36 were reviewed in full text and a total of five studies (4 RCTs and 1 retrospective study) met the inclusion criteria and included in the final analysis. Our analysis included 948 patients (pNKF= 473 vs. CEC= 475) [Table 1/2]. Compared to CEC, pNKF was associated with a significantly lower risk of PEP (1.5% vs. 6.7%; OR = 0.24, [95% CI: 0.09-0.63], p < 0.01; Figure 1-A) with no observed heterogeneity between included studies (I2 = 0%). Although there was no difference in the cannulation success rate between the two cohorts (OR=4.16, [95% CI: 0.69-25.25], p=0.89, I2 = 83%), NKF was associated with a lower rate of overall adverse events (OR=0.39, [95% CI: 0.20-0.75], p=0.01, I2 = 0%; Figure 1-B). Furthermore, there was no difference in the total procedural time (MD = 5.43, [95% CI: - 986 to 997], p=0.95, I2 = 96%) between both cohorts. No significant differences were observed in bleeding, perforation, cholangitis, or mortality.
Discussion: Primary needle-knife fistulotomy significantly reduces the risk of post-ERCP pancreatitis and overall adverse events without compromising cannulation success. These findings support the selective use of pNKF as a first-line approach in patients at elevated risk for PEP.
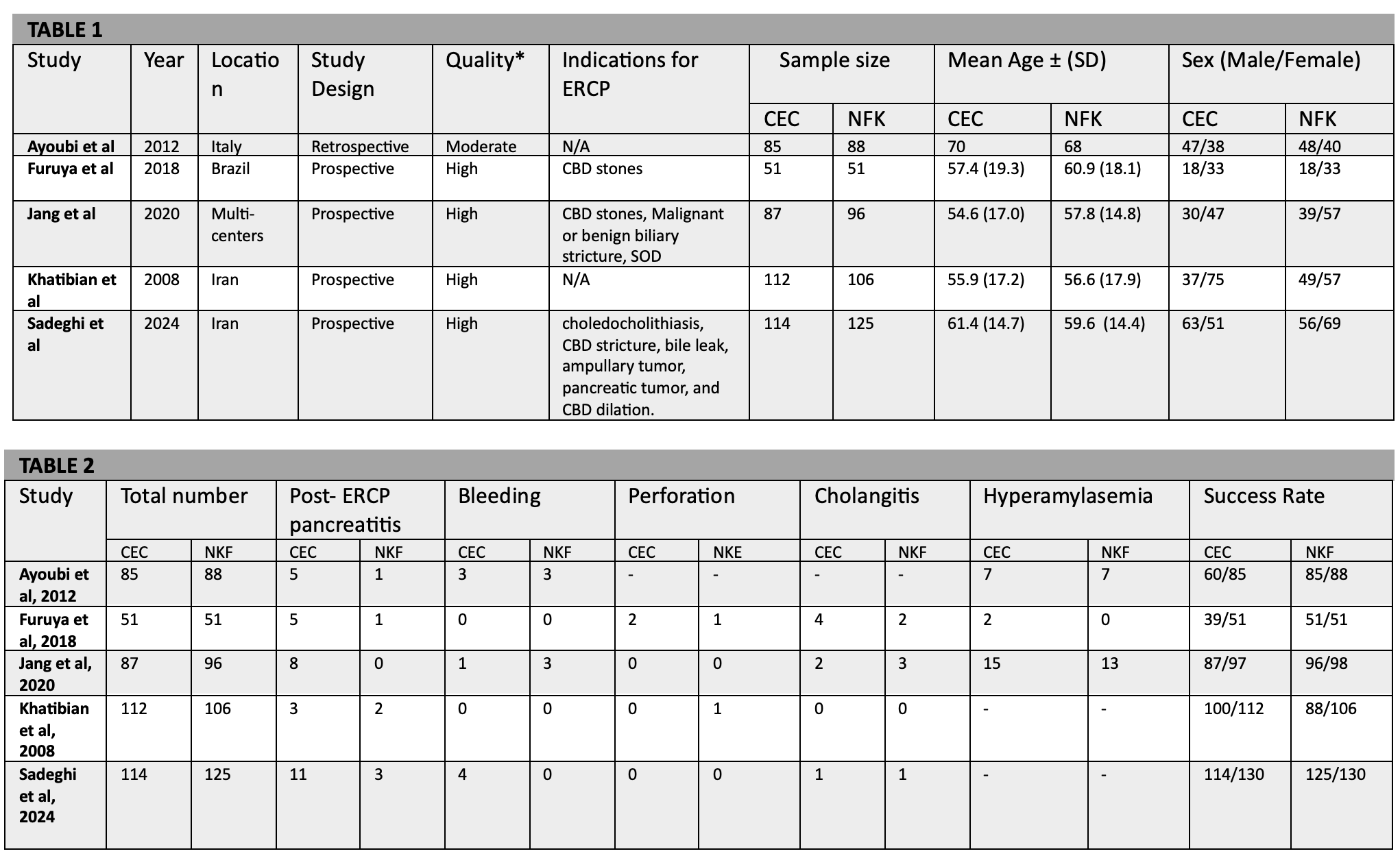
Figure: Table 1. Study details and baseline patient characteristics of included studies.
Table 2. Summary of primary and secondary outcomes across included studies.
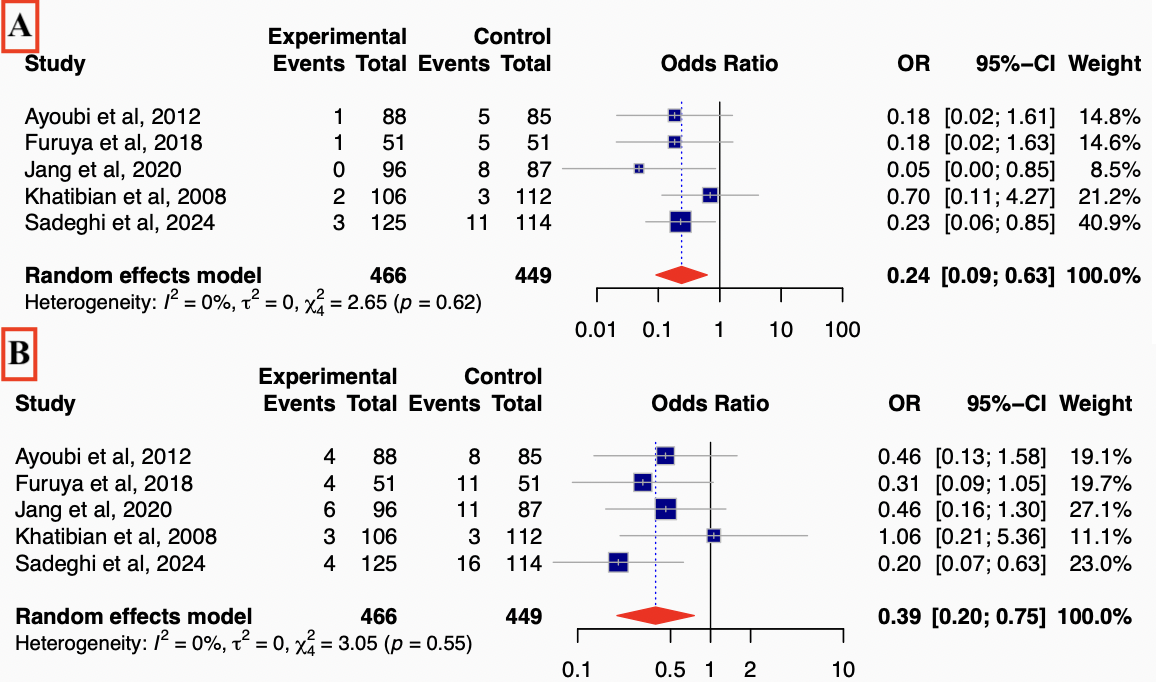
Figure: Figure 1. Forest plots showing (A) lower risk of post-ERCP pancreatitis (PEP) and (B) adverse events with pNKF compared to CEC.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Mohamad Adam indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Farah Khraisat indicated no relevant financial relationships.
Mohammad Abuassi indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Bashar Qumseya: Assertio Management – Consultant. Castle Biosciences – Food and beverage compensation. Endogastric Solutions – Consultant. Medtronic – Consultant.
Saqr Alsakarneh, MD, MS1, Mohamad Adam, MD2, Razan Aburumman, MD3, Farah Khraisat, MD4, Mohammad Abuassi, MD5, Mahmoud Y. Madi, MD6, Bashar Qumseya, MD, MPH7. P5661 - Primary Needle-Knife Fistulotomy Is an Effective and Safer Alternative to Conventional Cannulation in ERCP: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Mayo Clinic, Kansas City, MO; 2University of Missouri - Kansas City School of Medicine, Kansas City, MO; 3Henry Ford Health, Detroit, MI; 4University of Florida, Jacksonville, FL; 5University of Central Florida, HCA Healthcare GME, Gainesville, FL; 6University of Texas at Austin Dell Medical School, Austin, TX; 7University of Florida College of Medicine, Gainesville, FL
Introduction: In patients at high risk for post-ERCP pancreatitis (PEP), conventional ERCP cannulation (CEC) carries a PEP risk of up to 14%. Primary needle-knife fistulotomy (pNKF) has emerged as an alternative technique, allowing selective biliary access while minimizing trauma to the papillary orifice. This meta-analysis aims to compare the efficacy and safety of pNKF versus CEC.
Methods: A systematic literature search was performed using PubMed, Scopus, Embase, and Web of Science through May 2025. Studies were included if they compared pNKF (as the primary access method) to CEC in biliary drainage. Studies using pNKF as rescue/salvage therapy were excluded. Pooled odds ratios (ORs) and mean differences (MDs) with 95% confidence intervals (CIs) were calculated using random-effects models and the Mantel-Haenszel method. Heterogeneity was assessed via the I² statistic. The primary outcome was PEP. Secondary outcomes included cannulation success, procedure time, and other adverse events.
Results: Our search strategy resulted in 1874 citations, of which, 36 were reviewed in full text and a total of five studies (4 RCTs and 1 retrospective study) met the inclusion criteria and included in the final analysis. Our analysis included 948 patients (pNKF= 473 vs. CEC= 475) [Table 1/2]. Compared to CEC, pNKF was associated with a significantly lower risk of PEP (1.5% vs. 6.7%; OR = 0.24, [95% CI: 0.09-0.63], p < 0.01; Figure 1-A) with no observed heterogeneity between included studies (I2 = 0%). Although there was no difference in the cannulation success rate between the two cohorts (OR=4.16, [95% CI: 0.69-25.25], p=0.89, I2 = 83%), NKF was associated with a lower rate of overall adverse events (OR=0.39, [95% CI: 0.20-0.75], p=0.01, I2 = 0%; Figure 1-B). Furthermore, there was no difference in the total procedural time (MD = 5.43, [95% CI: - 986 to 997], p=0.95, I2 = 96%) between both cohorts. No significant differences were observed in bleeding, perforation, cholangitis, or mortality.
Discussion: Primary needle-knife fistulotomy significantly reduces the risk of post-ERCP pancreatitis and overall adverse events without compromising cannulation success. These findings support the selective use of pNKF as a first-line approach in patients at elevated risk for PEP.
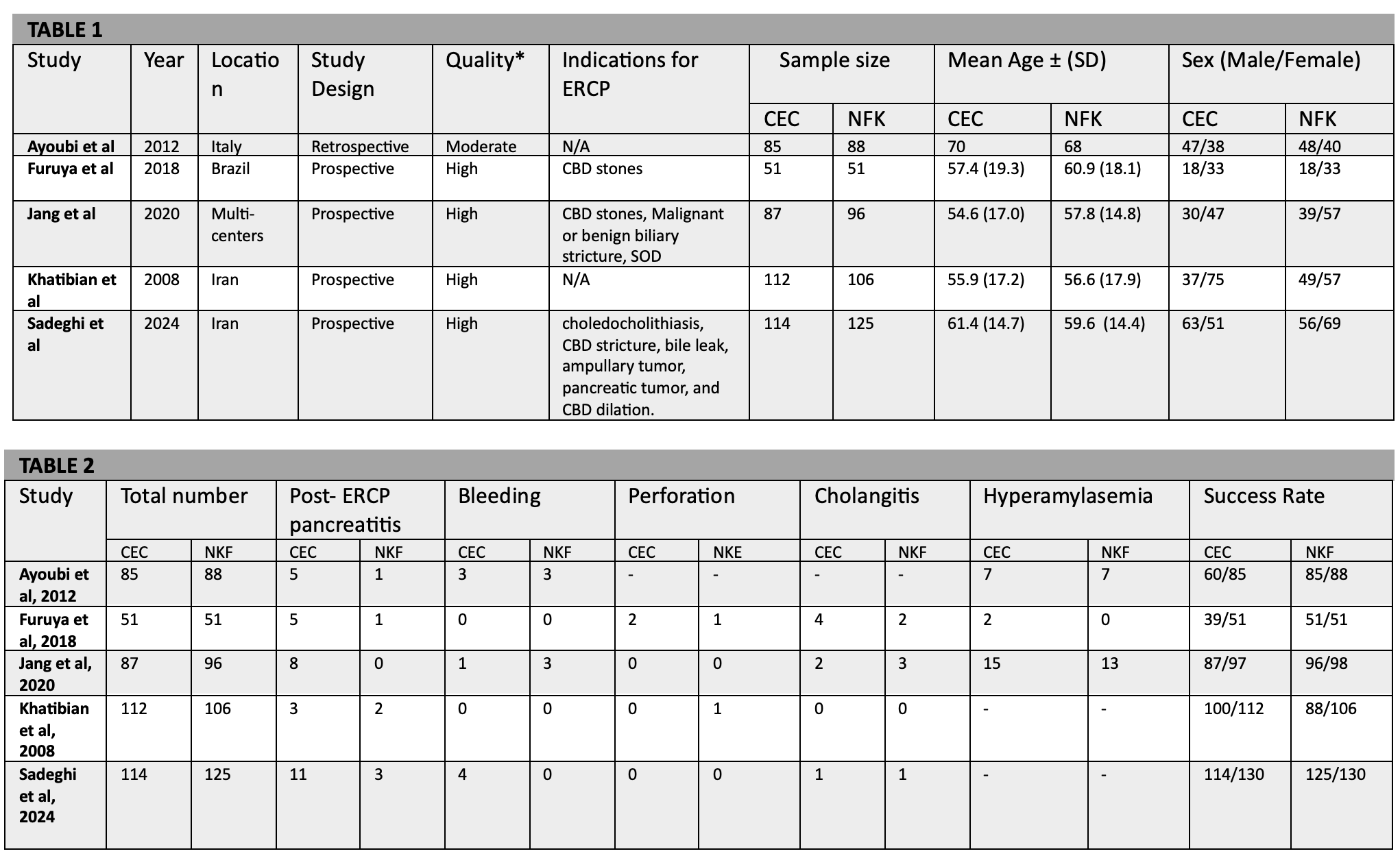
Figure: Table 1. Study details and baseline patient characteristics of included studies.
Table 2. Summary of primary and secondary outcomes across included studies.
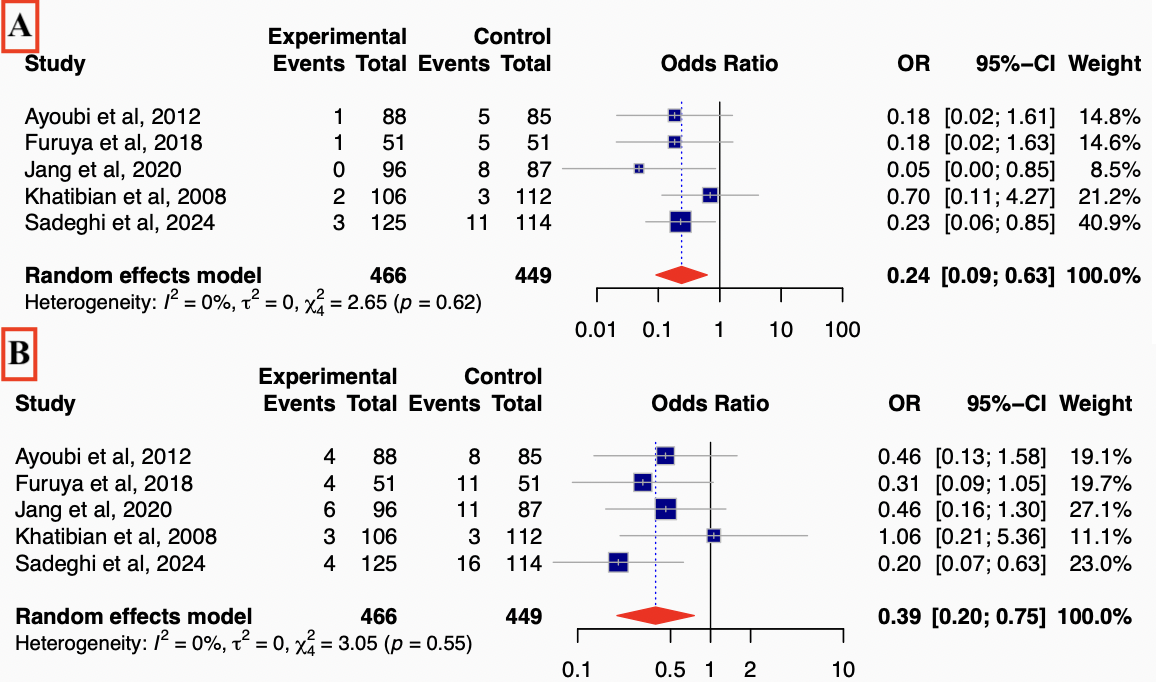
Figure: Figure 1. Forest plots showing (A) lower risk of post-ERCP pancreatitis (PEP) and (B) adverse events with pNKF compared to CEC.
Disclosures:
Saqr Alsakarneh indicated no relevant financial relationships.
Mohamad Adam indicated no relevant financial relationships.
Razan Aburumman indicated no relevant financial relationships.
Farah Khraisat indicated no relevant financial relationships.
Mohammad Abuassi indicated no relevant financial relationships.
Mahmoud Madi indicated no relevant financial relationships.
Bashar Qumseya: Assertio Management – Consultant. Castle Biosciences – Food and beverage compensation. Endogastric Solutions – Consultant. Medtronic – Consultant.
Saqr Alsakarneh, MD, MS1, Mohamad Adam, MD2, Razan Aburumman, MD3, Farah Khraisat, MD4, Mohammad Abuassi, MD5, Mahmoud Y. Madi, MD6, Bashar Qumseya, MD, MPH7. P5661 - Primary Needle-Knife Fistulotomy Is an Effective and Safer Alternative to Conventional Cannulation in ERCP: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
