Tuesday Poster Session
Category: Interventional Endoscopy
P5656 - Efficacy and Safety of Endoscopic Transcecal Appendectomy: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mohammed Y. Youssef, MD
Hunt Regional Medical Center
Greenville, TX
Presenting Author(s)
Mohammed Y. Youssef, MD1, Mohammed Al-Aquily, MD2, Mohamed A. Aldemerdash, 3, Ahmed Aref, MD4, Layth Alzubaidy, MD5, Muhammad Elsharkawy, MD6, Omar Abdelhalim, MD7, Nermin Elhossiny, 8, Ahmed Salem, MD9, Mohamed Eldesouki, MD10, Hazem Abosheaishaa, MD11
1Hunt Regional Medical Center, Greenville, TX; 2Norwalk Hospital/Yale University, Norwalk, CT; 3Sohag University, Faculty of Medicine, Sohag, Suhaj, Egypt; 4Corewell Health William Beaumont University Hospital, Royal Oak, MI; 5UT Health Science Center-Tyler, Tyler, TX; 6Cairo University School of Medicine, Cairo, Al Qahirah, Egypt; 7Icahn School of Medicine at Mount Sinai, Queens, NY; 8St Mary General hospital prime healthcare , NJ , USA, Passaic, NJ; 9Maimonides Medical Center, Brooklyn, NY; 10Saint Michael's Medical Center, New York Medical College, Newark, NJ; 11Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Appendiceal orifice polyps are rare with prevalence of 0.08%. The increased colon cancer screening led to more frequent detection. Surgical approach is the standard approach. Endoscopic Transcecal Appendectomy (ETA) has several potential advantages when compared to surgery including direct visualization of the appendiceal orifice, absence of abdominal incision and an alternative to non-surgical candidates. In this study, we conducted a systematic review and metanalysis to review the efficacy and safety of ETA for the management of appendiceal lesions
Methods: A systematic literature search was conducted across PubMed, Embase, Scopus, Web of Science, and Cochrane databases up to Feb. 28, 2025. Three studies comparing efficacy and safety of ETA for managing appendiceal orifice lesions were included. The primary outcome was the efficacy of ETA in achieving technical success and en-bloc resection. Secondary outcomes included recurrence rate, bleeding events, the mean hospital stay, and adverse events. A single arm meta-analysis was performed using a random-effects model.
Results: The total number of participants is 45 patients. The mean age is 61.8 SD (14.22). Females constituted 53.3 % of the clinical trials. The mean lesion size is 21.6 mm SD (10.54 mm). Tubular adenoma was the most common type of pathology with 12 adenomas.
The achieved technical success rate was 100% (95% CI: 92%–100%) (I² = 0%, τ² = 0, p = 1.000). The en-bloc resection had a success rate of 97% (95% CI: 90%–100%) (I² = 0%, p = 0.5913). The Recurrence rate was 0.0% (95% CI: 0.0%–5.0%) (I² = 0%, p = 1.000). No bleeding events were observed across studies with rates of 0.0% (95% CI :0.00-0.05) (I² = 0%, p = 1.000). Perforation was observed in 2 of 45 patients with rates of 3.0% (95% CI: 0.0%–9.0%) (I² = 0%, p = 0.475). The mean hospital stay was 7.27 days (95% CI: 2.94-11.6) (I² = 95.8%, p < 0.0001). The average procedure duration was 123.30 minutes (95% CI: 82.37-164.24) (I²=12 = 91.6%, p < 0.0001).
Discussion: This Meta-analysis shows that ETA is a promising, minimally invasive technique for appendiceal polyps. It demonstrated high efficacy with success rates reaching 100%. It also showed very minimal complication, with absent recurrence or bleeding and low perforation rates of 3%. This technique requires a high level of expertise with advanced endoscopic techniques. Given the limited sample size, future large-scale multicenter studies are warranted to further validate these results and establish a standardized guideline.
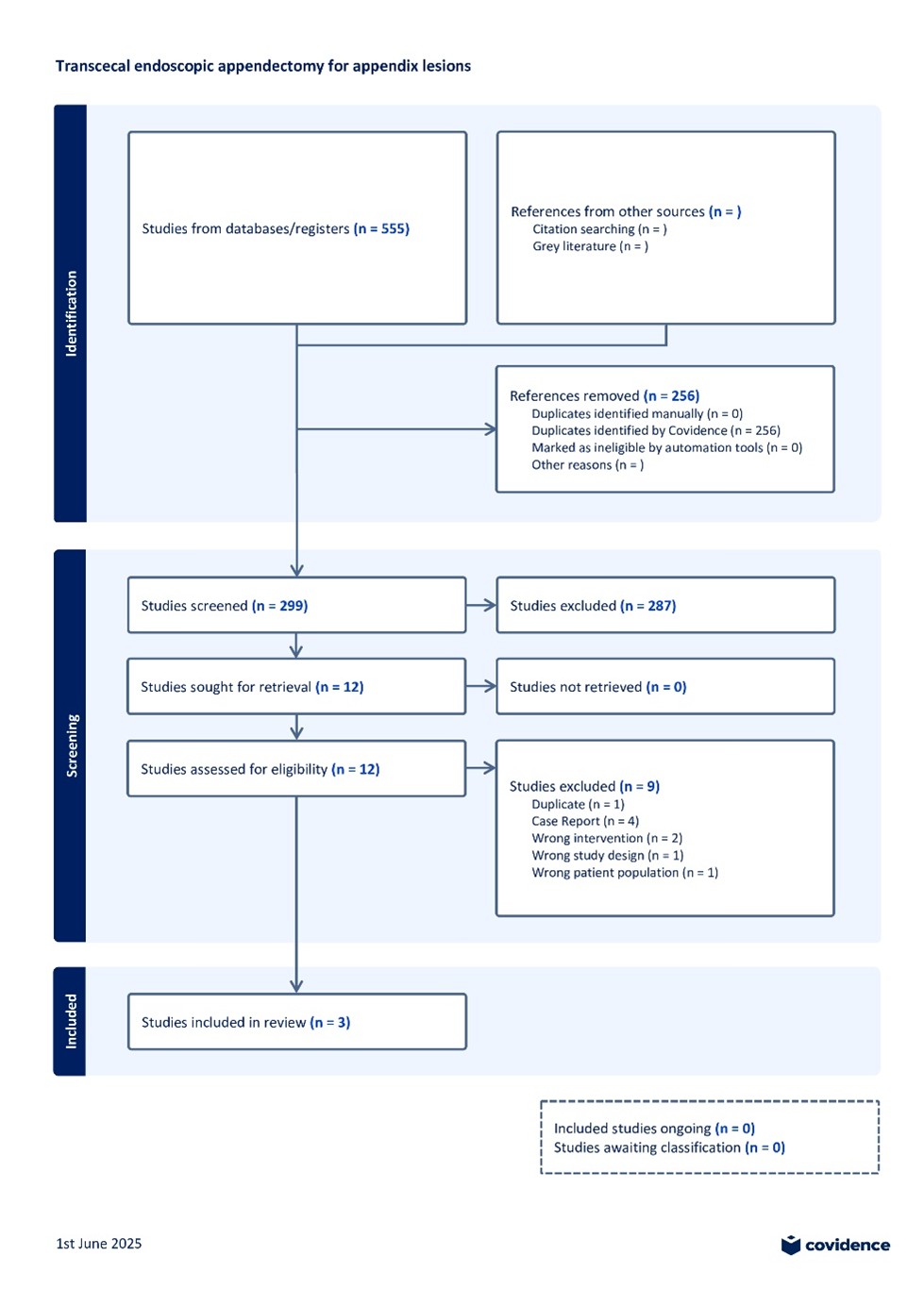
Figure: PRISMA flow diagram outlining the study selection process for a systematic review on transcecal endoscopic appendectomy for appendix lesions. Of 555 studies identified, 299 were screened, 12 assessed for eligibility, and 3 met inclusion criteria.
Disclosures:
Mohammed Y. Youssef indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Mohamed A. Aldemerdash indicated no relevant financial relationships.
Ahmed Aref indicated no relevant financial relationships.
Layth Alzubaidy indicated no relevant financial relationships.
Muhammad Elsharkawy indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Nermin Elhossiny indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohammed Y. Youssef, MD1, Mohammed Al-Aquily, MD2, Mohamed A. Aldemerdash, 3, Ahmed Aref, MD4, Layth Alzubaidy, MD5, Muhammad Elsharkawy, MD6, Omar Abdelhalim, MD7, Nermin Elhossiny, 8, Ahmed Salem, MD9, Mohamed Eldesouki, MD10, Hazem Abosheaishaa, MD11. P5656 - Efficacy and Safety of Endoscopic Transcecal Appendectomy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Hunt Regional Medical Center, Greenville, TX; 2Norwalk Hospital/Yale University, Norwalk, CT; 3Sohag University, Faculty of Medicine, Sohag, Suhaj, Egypt; 4Corewell Health William Beaumont University Hospital, Royal Oak, MI; 5UT Health Science Center-Tyler, Tyler, TX; 6Cairo University School of Medicine, Cairo, Al Qahirah, Egypt; 7Icahn School of Medicine at Mount Sinai, Queens, NY; 8St Mary General hospital prime healthcare , NJ , USA, Passaic, NJ; 9Maimonides Medical Center, Brooklyn, NY; 10Saint Michael's Medical Center, New York Medical College, Newark, NJ; 11Mount Sinai West, Icahn School of Medicine at Mount Sinai, Queens, NY
Introduction: Appendiceal orifice polyps are rare with prevalence of 0.08%. The increased colon cancer screening led to more frequent detection. Surgical approach is the standard approach. Endoscopic Transcecal Appendectomy (ETA) has several potential advantages when compared to surgery including direct visualization of the appendiceal orifice, absence of abdominal incision and an alternative to non-surgical candidates. In this study, we conducted a systematic review and metanalysis to review the efficacy and safety of ETA for the management of appendiceal lesions
Methods: A systematic literature search was conducted across PubMed, Embase, Scopus, Web of Science, and Cochrane databases up to Feb. 28, 2025. Three studies comparing efficacy and safety of ETA for managing appendiceal orifice lesions were included. The primary outcome was the efficacy of ETA in achieving technical success and en-bloc resection. Secondary outcomes included recurrence rate, bleeding events, the mean hospital stay, and adverse events. A single arm meta-analysis was performed using a random-effects model.
Results: The total number of participants is 45 patients. The mean age is 61.8 SD (14.22). Females constituted 53.3 % of the clinical trials. The mean lesion size is 21.6 mm SD (10.54 mm). Tubular adenoma was the most common type of pathology with 12 adenomas.
The achieved technical success rate was 100% (95% CI: 92%–100%) (I² = 0%, τ² = 0, p = 1.000). The en-bloc resection had a success rate of 97% (95% CI: 90%–100%) (I² = 0%, p = 0.5913). The Recurrence rate was 0.0% (95% CI: 0.0%–5.0%) (I² = 0%, p = 1.000). No bleeding events were observed across studies with rates of 0.0% (95% CI :0.00-0.05) (I² = 0%, p = 1.000). Perforation was observed in 2 of 45 patients with rates of 3.0% (95% CI: 0.0%–9.0%) (I² = 0%, p = 0.475). The mean hospital stay was 7.27 days (95% CI: 2.94-11.6) (I² = 95.8%, p < 0.0001). The average procedure duration was 123.30 minutes (95% CI: 82.37-164.24) (I²=12 = 91.6%, p < 0.0001).
Discussion: This Meta-analysis shows that ETA is a promising, minimally invasive technique for appendiceal polyps. It demonstrated high efficacy with success rates reaching 100%. It also showed very minimal complication, with absent recurrence or bleeding and low perforation rates of 3%. This technique requires a high level of expertise with advanced endoscopic techniques. Given the limited sample size, future large-scale multicenter studies are warranted to further validate these results and establish a standardized guideline.
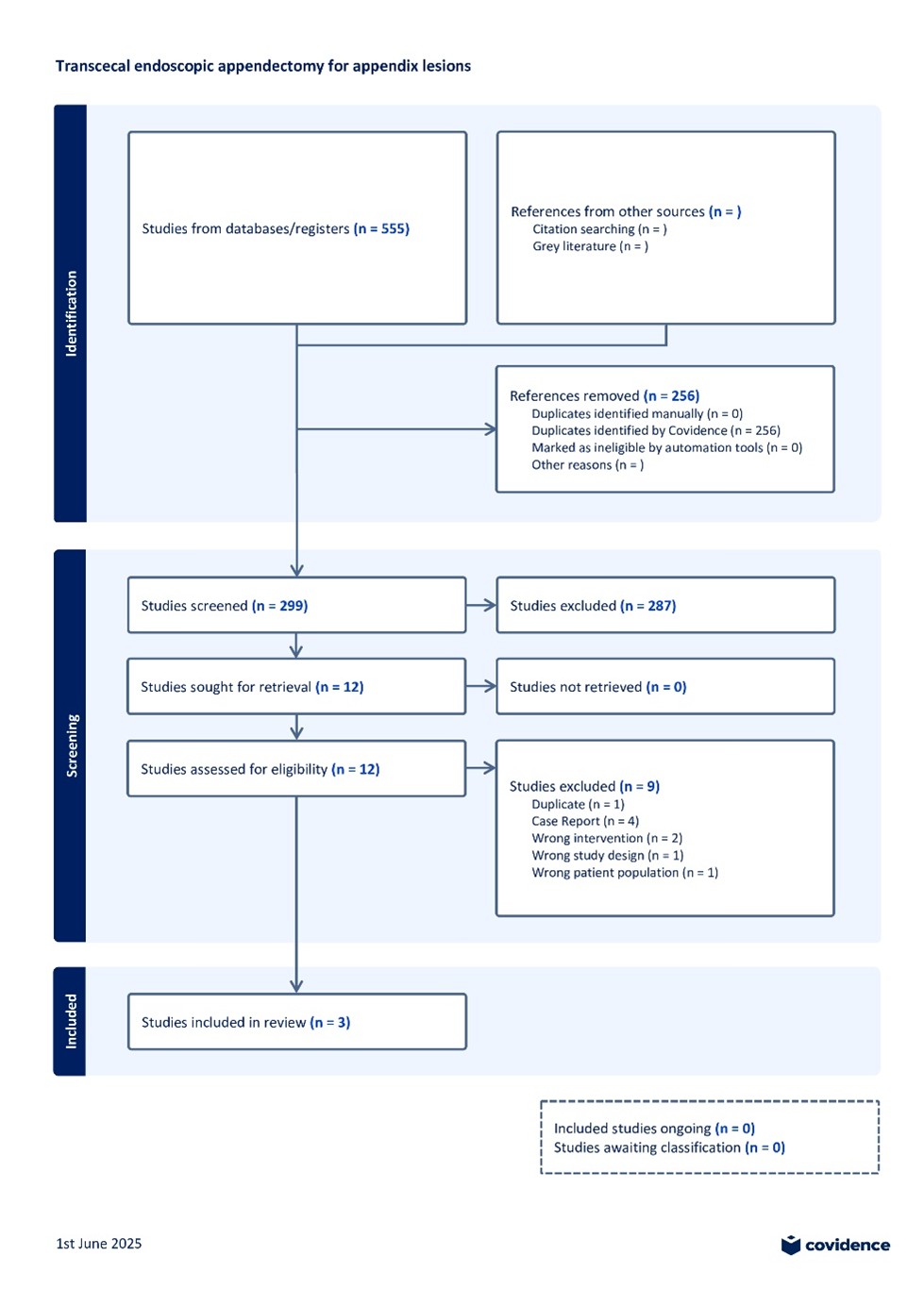
Figure: PRISMA flow diagram outlining the study selection process for a systematic review on transcecal endoscopic appendectomy for appendix lesions. Of 555 studies identified, 299 were screened, 12 assessed for eligibility, and 3 met inclusion criteria.
Disclosures:
Mohammed Y. Youssef indicated no relevant financial relationships.
Mohammed Al-Aquily indicated no relevant financial relationships.
Mohamed A. Aldemerdash indicated no relevant financial relationships.
Ahmed Aref indicated no relevant financial relationships.
Layth Alzubaidy indicated no relevant financial relationships.
Muhammad Elsharkawy indicated no relevant financial relationships.
Omar Abdelhalim indicated no relevant financial relationships.
Nermin Elhossiny indicated no relevant financial relationships.
Ahmed Salem indicated no relevant financial relationships.
Mohamed Eldesouki indicated no relevant financial relationships.
Hazem Abosheaishaa indicated no relevant financial relationships.
Mohammed Y. Youssef, MD1, Mohammed Al-Aquily, MD2, Mohamed A. Aldemerdash, 3, Ahmed Aref, MD4, Layth Alzubaidy, MD5, Muhammad Elsharkawy, MD6, Omar Abdelhalim, MD7, Nermin Elhossiny, 8, Ahmed Salem, MD9, Mohamed Eldesouki, MD10, Hazem Abosheaishaa, MD11. P5656 - Efficacy and Safety of Endoscopic Transcecal Appendectomy: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
