Tuesday Poster Session
Category: Interventional Endoscopy
P5647 - Reassessing Bleeding Risk in Antithrombotic Patients Undergoing Upper GI Dilation: Insights From a TriNetX Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- OA
Osama Alshakhatreh, MD (he/him/his)
Albany Medical Center
Norfolk, VA
Presenting Author(s)
Osama Alshakhatreh, MD1, Omar Arman, MD, MPH2, Tejash E. Sikka, BS3, Tarick Ahmad, BS1, Ibrahim Mohammed, MD1, Arba Goskova, 1, Seth Richter, MD, FACG1
1Albany Medical Center, Albany, NY; 2University at Buffalo, Buffalo, NY; 3Albany Medical College, Albany, NY
Introduction: Endoscopic dilation is essential for managing upper GI strictures. Antithrombotic agents pose procedural bleeding concerns, yet comparative data between anticoagulant (AC) and dual antiplatelet therapy (DAPT) users remain limited. This study evaluates bleeding and clinical outcomes post-dilation in AC vs DAPT patients using a large real-world dataset.
Methods: We conducted a retrospective cohort study using TriNetX, a global federated electronic health record network. Adult patients who underwent upper GI endoscopic dilation were identified using CPT and ICD-10-PCS codes. Two cohorts were defined based on treatment within 7 days prior to procedure: patients on anticoagulation (warfarin or direct oral anticoagulants (DOACs)), and those on DAPT (aspirin with clopidogrel, prasugrel, or ticagrelor), with all patients excluded if on both medication types. Propensity score matching (1:1) was applied to control for demographics, comorbidities including chronic kidney disease, ischemic heart disease, heart failure, thrombocytopenia, and PPI use. The primary outcomes assessed at 30 days of dilation included GI bleeding, hospitalizations, and need for blood transfusions. Falsification endpoints were included to validate the findings.
Results: After matching, 1,436 patients were included in each group. GI bleeding was significantly higher in the DAPT group compared to the AC group (11.4% vs 8.2%; RR 1.39; p=0.004). Transfusion rates were also higher in DAPT users (7.2% vs 3.4%; RR 2.10; p< 0.001), while hospitalization rates were similar between groups (48.4% vs 47.3%; p=0.55). Subgroup analysis revealed GI bleeding occurred in 7.8% of DOAC users and 8.9% of warfarin users. Kaplan-Meier analysis confirmed a greater probability of remaining bleeding free in AC patients over 30 days (91.4%, vs 88%, p=0.005). Falsification endpoints showed no significant differences, supporting the internal validity of the results.
Discussion: Despite conventional concerns, AC use, including DOACs and warfarin, was associated with lower post-dilation GI bleeding and transfusion rates compared to DAPT. This may reflect platelet-driven mucosal injury in DAPT or more cautious periprocedural management in AC patients. These findings challenge existing assumptions and suggest that anticoagulation alone should not delay or preclude upper GI dilation. Further prospective studies are warranted to refine procedural guidelines.
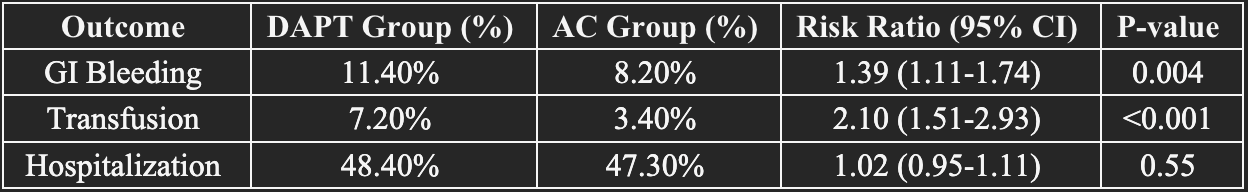
Figure: Table 1. Comparative Risk of Adverse Outcomes After Upper GI Endoscopic Dilation in Patients on Dual Antiplatelet Therapy (DAPT) vs Anticoagulation (DOAC or Warfarin)
Disclosures:
Osama Alshakhatreh indicated no relevant financial relationships.
Omar Arman indicated no relevant financial relationships.
Tejash Sikka indicated no relevant financial relationships.
Tarick Ahmad indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Arba Goskova indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Osama Alshakhatreh, MD1, Omar Arman, MD, MPH2, Tejash E. Sikka, BS3, Tarick Ahmad, BS1, Ibrahim Mohammed, MD1, Arba Goskova, 1, Seth Richter, MD, FACG1. P5647 - Reassessing Bleeding Risk in Antithrombotic Patients Undergoing Upper GI Dilation: Insights From a TriNetX Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Albany Medical Center, Albany, NY; 2University at Buffalo, Buffalo, NY; 3Albany Medical College, Albany, NY
Introduction: Endoscopic dilation is essential for managing upper GI strictures. Antithrombotic agents pose procedural bleeding concerns, yet comparative data between anticoagulant (AC) and dual antiplatelet therapy (DAPT) users remain limited. This study evaluates bleeding and clinical outcomes post-dilation in AC vs DAPT patients using a large real-world dataset.
Methods: We conducted a retrospective cohort study using TriNetX, a global federated electronic health record network. Adult patients who underwent upper GI endoscopic dilation were identified using CPT and ICD-10-PCS codes. Two cohorts were defined based on treatment within 7 days prior to procedure: patients on anticoagulation (warfarin or direct oral anticoagulants (DOACs)), and those on DAPT (aspirin with clopidogrel, prasugrel, or ticagrelor), with all patients excluded if on both medication types. Propensity score matching (1:1) was applied to control for demographics, comorbidities including chronic kidney disease, ischemic heart disease, heart failure, thrombocytopenia, and PPI use. The primary outcomes assessed at 30 days of dilation included GI bleeding, hospitalizations, and need for blood transfusions. Falsification endpoints were included to validate the findings.
Results: After matching, 1,436 patients were included in each group. GI bleeding was significantly higher in the DAPT group compared to the AC group (11.4% vs 8.2%; RR 1.39; p=0.004). Transfusion rates were also higher in DAPT users (7.2% vs 3.4%; RR 2.10; p< 0.001), while hospitalization rates were similar between groups (48.4% vs 47.3%; p=0.55). Subgroup analysis revealed GI bleeding occurred in 7.8% of DOAC users and 8.9% of warfarin users. Kaplan-Meier analysis confirmed a greater probability of remaining bleeding free in AC patients over 30 days (91.4%, vs 88%, p=0.005). Falsification endpoints showed no significant differences, supporting the internal validity of the results.
Discussion: Despite conventional concerns, AC use, including DOACs and warfarin, was associated with lower post-dilation GI bleeding and transfusion rates compared to DAPT. This may reflect platelet-driven mucosal injury in DAPT or more cautious periprocedural management in AC patients. These findings challenge existing assumptions and suggest that anticoagulation alone should not delay or preclude upper GI dilation. Further prospective studies are warranted to refine procedural guidelines.
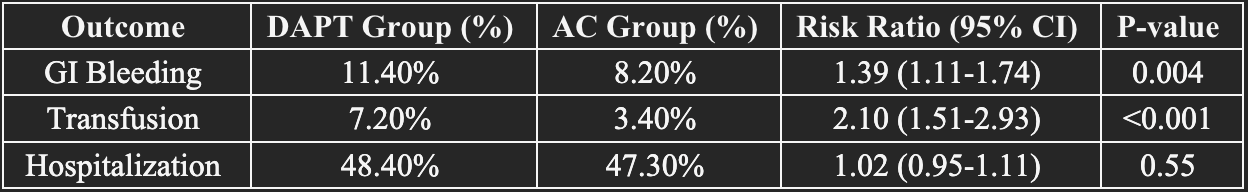
Figure: Table 1. Comparative Risk of Adverse Outcomes After Upper GI Endoscopic Dilation in Patients on Dual Antiplatelet Therapy (DAPT) vs Anticoagulation (DOAC or Warfarin)
Disclosures:
Osama Alshakhatreh indicated no relevant financial relationships.
Omar Arman indicated no relevant financial relationships.
Tejash Sikka indicated no relevant financial relationships.
Tarick Ahmad indicated no relevant financial relationships.
Ibrahim Mohammed indicated no relevant financial relationships.
Arba Goskova indicated no relevant financial relationships.
Seth Richter indicated no relevant financial relationships.
Osama Alshakhatreh, MD1, Omar Arman, MD, MPH2, Tejash E. Sikka, BS3, Tarick Ahmad, BS1, Ibrahim Mohammed, MD1, Arba Goskova, 1, Seth Richter, MD, FACG1. P5647 - Reassessing Bleeding Risk in Antithrombotic Patients Undergoing Upper GI Dilation: Insights From a TriNetX Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
